Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 1 - July 2019
Evaluation of serum and pleural fluid protein levels in patients of pleural effusion
Sneha S Narkar1, S A Rane2*, D S Salgaonkar3
1Jr. Scientific Officer, Paediatric Research Laboratory, Seth G.S. Medical College and KEM Hospital, Parel, Mumbai – 400 012, INDIA. 2Associate Professor, Department of Biochemistry, Seth G.S. Medical College & KEM Hospital, Parel Mumbai – 400 012, INDIA. 3Senior Biochemist, Medicine Laboratory, Topiwala National Medical College and Nair Hospital, Dr. A.L. Nair road, Mumbai – 400 007, INDIA. Email: Snarkar64@gmail.com, drsarane@gmail.com, salsan_16@yahoo.com
Abstract Background: Patients with pleural effusion are classified into two different groups, that is either transudative or exudative. This is necessary as the therapy differs. There exist cases of pleural effusion with secondary infection which will also have effect on the biochemical composition of pleural fluid. Classification of cases into transudate and exudates is done mainly on the protein content of pleural fluid. Objective: To evaluate and access the sensitive marker for the differentiation of fluid, protein content was estimated. Material and methods: Patients with pleural effusion attending chest clinic of Nair hospital were selected. For comparison, healthy individuals without any past history of chest disease admitted in the Nair hospital were selected as controls. Serum and fluid were processed estimation protein electrophoresis. Results: Sixty three patients were included in the study. most of the patients were in the age group of 21-40 years. the most common cause of effusion was Tuberculosis followed by Nephrotic syndrome and bacterial empyema. The pleural fluids were classified into transudative and exudative based on the protein content in plasma as well as pleural fluid. The Total protein content and pleural fluid to serum protein ratio were used to classify the pleural fluids. Total protein is significantly reduced in nephrotic syndrome and cirrhosis of liver in serum as well as pleural fluid. Protein content in pseudopancreatic cyst in pleural fluid is reduced. Prealbumin is decreased in tuberculosis, nephrotic syndrome and cirrhosis of liver both in serum as well as in pleural fluid. Conclusion: The protein content of the serum as well as pleural fluid is affected due to underlying pathology. Pleural fluid protein to serum protein ratio is useful indicator to differentiate pleural fluid in exudate or transudate in nephrotic syndrome and cirrhosis of liver. Key Word: Serum, Pleural fluid, Prealbumin, Total Protein, Pleural effusion
INTRODUCTION Pleural effusion is a characteristic clinical finding in certain type of lung diseases, sometimes this is associated with secondary infection. The primary aim of clinician in the examination of pleural fluid is to determine whether it is transudate or exudates in nature. Once nature of pleural fluid is known, further line of treatment on the part of clinician is easy. This is generally achieved by estimation of total protein alone content of pleural fluid. It is also not clearly understood whether estimation of total protein alone is sensitive diagnostic test to decide the nature of pleural fluid. The total protein content in the pleural fluid enables classification into transudate and exudate1. Horace2reported that the total protein contained in pleural effusion is higher due to inflammatory and neoplastic processes than those due to congestive failure, hepatic cirrhosis or nephrotic syndrome. Variations in prealbumin in blood have been reported to have diagnostic significance. Prealbumin is normally present in the serum as a globulin fraction in the concentration of 28-35mg/100ml3,4. Various scientists have carried out work on prealbumin and reported that prealbumin is decreased in inflammation, stress and trauma 3,5,6. Ramkrishnan4 found that in 11 cases of tuberculous pleural effusion and in 12 cases of ascetic fluid tuberculous peritonitis, prealbumin was not detectable in the concerned fluids. It appears thus that prealbumin is highly labile in tuberculous conditions. Helen7 found that the prealbumin also decreased in blood. Ingenbleek6, Wright8 and Helen7 have demonstrated presence of more than one prealbumin fraction in leukemias. Also, an associated secondary infection has an effect on formation and composition of pleural fluid. It was of interest to study the changes in biochemical composition of pleural fluid with respect to protein content.
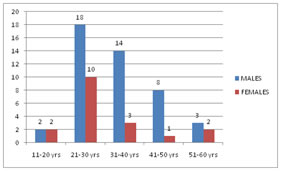
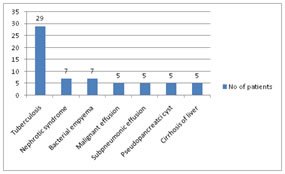
METHODOLOGY It was an observational cross sectional study. The patient population was the patients who attended Chest OPD and admitted in the wards of BYL Nair Charitable Hospital, Mumbai. The individuals who attended Chest Clinic with evidence of accumulation of fluid in lungs on radiological examination, of both gender and all age groups, irrespective of co-morbidities were included in the study. At the same time, healthy individuals without any past history of chest disease admitted in the hospital for minor surgery, who had undergone complete medical and laboratory examinations including chest normal X ray, were selected as controls. Patients and Controls were allowed to have dinner in the evening prior to collection of specimen. Next day morning, after 12-14 hours of overnight fasting, blood was collected in fluoride bulb. Patients as well as control’s blood was processed for the estimation of protein electrophoresis. Estimation of total protein was done by Biuret reaction. Albumin concentration was determined by Bromocresol Green binding method. Pre-albumin was estimated using the Polyarylamide gel electrophoretic method. RESULTS In the present study, 63 patients were included ranging from age of 11 to 60 years. Figure 1: Distribution of patients according to their age group Figure 2: Distribution of patients according to cause of pleural effusion Figure no. 1 shows the distribution of patients in different age group and sex. In the present study, pleural effusion was seen predominantly more common in middle age group ie, 21-40 years (71.4%). Figure no.2 represents diseases associated with pleural effusion. Tuberculosis (46%) was the most common cause of effusion. Table 1: Difference of pleural effusion between exudates and transudates
Table no. 1 shows the classification of pleural fluid in transudate/exudates groups. Pleural fluid protein level of 3g/100ml is frequently used to separate transudate from exudates.
Table 2: Mean serum Pre albumin levels in different disease groups
Table 3: Pleural fluid Pre albumin levels in different disease groups
Level of serum and pleural fluid prealbumin is shown in Table no. 2 and 3. In the present study, prealbumin is decreased in tuberculosis, nephrotic syndrome and cirrhosis of liver both in serum as well as in pleural fluid.
DISCUSSION In a study by Finney, the 274 patients of pleural effusion were diagnosed; the most common cause (30%) was carcinoma9. Hirsch10 found cancer followed by tuberculosis and bacterial infection to the common cause of pleural effusion. Lueallen11, in his study on 436 patients, observed that Tuberculosis was the most common cause (66.6%) of pleural effusion. It can be seen that the prevalence of tuberculosis and malignancy was common among the patients of pleural effusion. Tuberculosis was more common in our setting due to higher prevalence of tuberculosis in community (Figure no.2). Table no. 1 shows the classification of pleural fluid in transudate/exudates groups. The criterion of Pleural fluid protein level of 3g/100ml, which is frequently used to separate transudate from exudates, has consistently led to the misclassification of many effusions. If the fluid protein content is more than 3gm%, then pleural effusion is said to be exudative. In the present study, all the effusion associated with nephrotic syndrome, cirrhosis of liver and pseudopancreatic cystare transudative. In empyema and tuberculosis, majority of the cases are exudative which is similar to the study carried out by Carr12, who found that all 29 tuberculosis pleural fluids he studied contained more than 3gm% protein. Berger13 found 77% of his cases having protein concentration more than 5gm%, while Epstein14 found all his cases as exudates. Light1 observed that 8% of transudates and 11% of exudates in his study being misclassified on the basis of total protein content of pleural fluid. Light1 proposed that any pleural effusion to be termed as exudates, one of the criteria to be Pleural protein to serum protein ratio more than 0.5. In nephrotic syndrome, total protein and pleural fluid to serum protein ratio is the most sensitive indicator to differentiate between exudates and transudate. By using this criterion, all the 7 cases of nephrotic syndrome show transudate nature. Total protein is more useful indicator to differentiate pleural fluid in pseudo pancreatic cyst. In cirrhosis of liver total protein is less than 3gm% in all 5 cases studied. Pleural fluid to serum protein ratio is less than 0.5 in four cases. Total protein and pleural fluid protein to serum protein ratio are useful indicators to differentiate pleural fluid in nephrotic syndrome and cirrhosis of liver. In the present study, prealbumin is decreased in tuberculosis, nephrotic syndrome and cirrhosis of liver both in serum as well as in pleural fluid. Prealbumin level in both serum and pleural fluid is significantly decreased in tuberculosis effusion (Table no. 2 and 3). It is reported that prealbumin is decreased in inflammatory, stress and trauma 3,5,6. Hence in pulmonary tuberculosis due to inflammatory condition prealbumin could be decreased. In fact, Schultze15observed that decrease in prealbumin in CHF in tuberculosis abscesses. Ramkrishnan4 have reported 11 cases of tuberculous meningitis as well as peritonitis each, prealbumin could not be detected by polyacrylamide disc electrophoresis in CSF and ascetic fluid, respectively. It is observed that in tuberculous condition affecting different parts of the body prealbumin levels are specifically and significantly decreases4. The reason for decreased prealbumin in tuberculous conditions could be due to its labile nature and quick degradation in this wasting disease. Its biological half life is just 1.9 days and prealbumin is extremely short lived. There would be negative nitrogen balance and the body protein would be utilized for energy purpose and in this process, free tryptophan accumulated in fluid. In all tuberculous conditions, decrease of prealbumin in the bio-fluids could not be due to defective synthesis as the liver which is the site for prealbumin synthesis is normal and it is only other organs which are affected. Prealbumin is decreased in all 7 cases of nephrotic syndrome in both serum and pleural fluid. It is decreased in nephrotic syndrome due to it’s loss in urine. In empyema prealbumin in pleural fluid is either increased or normal. Its increase or normal value in empyema may due to increased permeability for high molecular weight as well as low molecular weight protein in these conditions. In cirrhosis of liver, prealbumin is decreased in both pleural fluid and in serum. Its value in malignant effusion, synpneumonic effusion and in pseudopancreatic cyst are nonconclusive. In the present study, prealbumin is decreased in tuberculosis, nephrotic syndrome and cirrhosis of liver both in serum as well as in pleural fluid.
CONCLUSION Prealbumin is considerable reduced in tuberculosis, nephrotic syndrome, both in blood as well as in pleural fluid. It also shows considerable decrease in cirrhosis of liver in pleural fluid. Total protein is significantly reduced in nephrotic syndrome and cirrhosis of liver in serum as well as pleural fluid. It also shows reduced protein content in pseudo pancreatic cyst in pleural fluid. Pleural fluid protein to serum protein ratio is useful indicator to differentiate pleural fluid in exudate or transudate in nephrotic syndrome and cirrhosis of liver.
REFERENCES
|
 Home
Home