Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 3 - September 2019
Can early evaluation of ‘routinely assayed TSH’ predict the risk of preeclampsia?
Rimsha Saleem F1, Swetha Chandru2*, Monalisa Biswas3
13rd Year MBBS student, 2Assistant Professor, Department of Biochemistry, MVJ Medical College and Research Hospital, Bangalore, Karnataka, INDIA. 3PhD Fellow. Department of Biochemistry, Kasturba Medical College, Manipal Academy of Higher Education (MAHE), Manipal, Karnataka, INDIA. Email: drswethac@gmail.com, rimshasaleem59@gmail.com, monalisabiswas89@gmail.com
Abstract Objectives: To study the potential of cost effective and routinely assessed TSH in preeclampsia in the South Indian rural population. Methodology: This is a cross-sectional study with 30 patients of preeclampsia and 30 normotensive gestational age matched healthy controls, blood samples from participants were analysed for TSH and LDH. Results: Our study showed a higher prevalence of hypothyroidism in preeclampsia when compared to controls, preeclampsia patients with hypothyroidism showed a significantly elevated LDH when compared to those with normal serum TSH. Conclusions: Our study indicates that women with preeclampsia show a higher incidence of hypothyroidism, hypothyroidism may be related to improper placentation and development if hypertension in pregnancy. Being an affordable and easily accessible marker, it can be used as a predictor and risk assessor of preeclampsia, of validated by multicentric prospective studies and more studies of such accessible markers should be carried out to design an effective screening panel in a rural and sub urban dominant Indian population. Key Words: ANC check-ups, Eclampsia, LDH, Maternal mortality, Preeclampsia, TSH.
INTRODUCTION The fifth Millennium Development Goals pledges commitment to achieve 75% reduction in maternal mortality and universal access to reproductive health.1,2 Despite the progress made in medical science, approximately 800 women die around the world every day from preventable causes related to pregnancy and childbirth (20% from India).3 Haemorrhage, infections, hypertensive disorders (preeclampsia and eclampsia) account for 80% of all maternal deaths.4 Globally, preeclampsia is a leading cause of maternal and infant illness and mortality claiming upto 76,000 maternal and 5,00,000 infant deaths per year, according to conservative estimates.5 India reports a preeclampsia incidence of 8 – 10 %.6 Preeclampsia is a pregnancy specific syndrome that can affect every organ system. It is a rapidly progressive condition characterised by increased blood pressure (140/90 mm Hg), with fluid retention and proteinuria that occurs after 20 weeks of gestation.7 Nulliparity, multifetal gestations, obesity, diabetes mellitus, maternal age above 35 years etc predispose to preeclampsia.8 The condition becomes further challenging and enigmatic since it often develops without noticeable symptoms and shows a sudden and acute onset. A delay in diagnosis can lead to serious and even fatal complications for both the mother and the baby including IUGR, IUD, preterm birth, placental abruption, HELLP syndrome, eclampsia and severe damage to major organs like liver and kidneys and even death warranting markers for effective diagnosis, management and desirable maternal and foetal outcomes. Once called “the disease of theories”, a lot of breakthroughs have been made in an attempt to search for the causes and markers of preeclampsia, in the recent times. Current research on this subject aim to evaluate the role of hormones, proteins, enzymes and metabolites produced or the levels altered in preeclampsia and the early predictive values of the potential markers.5 Though a lot of novel and promising signalling markers, angiogenic and growth factors have been proposed, yet none has been implemented into routine and widespread clinical practice for early risk assessment and diagnosis of preeclampsia. This could be due to shortcomings in translation of these markers into the routine laboratory analytical platform and the associated high expenses. In a developing country like India, with a huge rural population, social norms and socio-economic factors often affect the accessibility to health care services. Further, their low economic status and ignorance lead to non-compliance to visiting ANC clinics for regular check-ups, to the medications prescribed and tests ordered. Hence the need of the hour is the investigation of easily accessible and affordable markers and screening panels for risk assessment which could be cater to and could be effectively implemented especially in our resource and technology constrained rural and sub urban setups.This report based on our ICMR STS project “A cross sectional hospital based study of serum TSH, LDH and uric acid in preeclampsia and normotensive pregnant women” presents excerpts of the findings of our study and aims to highlight the promise and importance of the routine assayed biomarkers in prediction and diagnosis of preeclampsia.
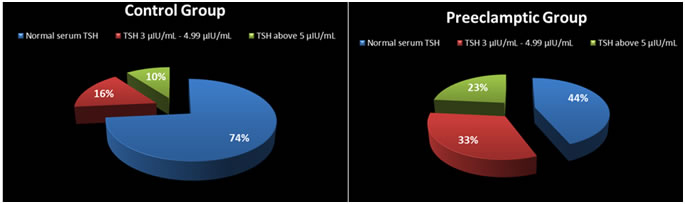
MATERIAL AND METHODS The study is a cross sectional study carried out in 60 women admitted to the Department of Obstetrics and Gynaecology in MVJ Medical College and Research Hospital. 30 women with preeclampsia constituted the case group. 30 normotensive gestational age matched pregnant women admitted to the antenatal ward participated as controls. Ethical approval was obtained from the Institutional Ethical Committee and an informed consent was taken from all the participants of the study. Blood samples collected from the study participants were assayed for TSH (ECLIA) and LDH (DGKC) in the Clinical Biochemistry Laboratory of MVJ Medical College and Research Hospital. RESULTS The preeclampsia group had 16 cases of mild preeclampsia and 14 cases of severe preeclampsia. Figure I and Figure II show the percentage of participants having elevated TSH in control and cases group and it is clearly seen that the preeclampsia group had a substantially higher percentage of women with hypothyroidism. Further, we observed that a large proportion of these patients were unaware of their hypothyroid status throughout their gestational period and hence received no supplementation or treatment for the same, either due to non-attendance to antenatal check-ups in the early gestation or failure to comply to the physician ordered tests which might have aggravated and worsened their adverse outcomes pertaining but not limited to preeclampsia alone. Further, LDH (marker of tissue anoxemia and anaerobiosis) was measured in preeclampsia patients. The serum LDH in patients with normal thyroid function was lower when compared with LDH in patients with elevated TSH levels and difference was found to be statistically significant showing a P value of 0.04 (Table I).
Figure I: Pie chart showing TSH levels in control group Figure II: Pie chart showing TSH values in preeclamptic group
Table I: Comparison of serum LDH in patients with normal and elevated TSH levels
Table II shows the prevalence ratio of hypothyroidism in patients with preeclampsia. Table II: Odds Ratio of acquiring preeclampsia
DISCUSSION The results of our study show that hypothyroidism in early pregnancy might indicate improper placentation, development of hypoxia and may signify the risk of development of preeclampsia and correlate to its severity. Studies show the presence of hypothyroxinemia in preeclampsia, the high prevalence of thyroid disorders associated with adverse maternal and foetal outcomes, a significant correlation of preeclampsia and subclinical hypothyroidism and a high incidence of hypertensive disorders in pregnant women with subclinical hypothyroidism.9-11 A significant increase in serum TSH levels in preeclamptic-eclamptic group has been reported when compared to normotensive pregnant women concluding that moderate decreases in thyroid hormone with concomitant increases in TSH levels correlates with severity of preeclampsia.12 Hence, though thyroid function status has been reported to be associated with preeclampsia, the implementation of this marker in risk assessment of preeclampsia is still not implemented clinically. Further, the results from a KAP questionnaire study by our group indicates that the considerable proportion of the rural population is still unaware of the signs and symptoms of hypertension and the implications of thyroid disorders and hypertensive disorders of pregnancy indicating the need for generating mass awareness among about disorders of pregnancy and the importance of early and regular antennal check-ups.
CONCLUSION Hence, we conclude that there is a pressing need for multicentre and grass root level prospective studies to validate the predictive potential of cost effective, widely assayed and easily accessible biomarkers and set up an implementable screening panel in resource constrained settings for risk assessment of hypertensive disorders of pregnancy. This could prevent the development of severe and adverse outcomes by early prophylactic interventions in “at risk” pregnant women effectively reducing the maternal and neonatal mortality and morbidity rates.
REFERENCES
|
|||||||||||||||||||||||||||
 Home
Home