Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 3 - December 2019
B Bhanuja Rani1, Devi Kinnera T2*, C V Sarada3, Lavanya4
1Assistant Professor, Department of Biochemistry, Gandhi Medical College, Secunderabad. 2Consultant in Lucid Diagnostics, Department of Bio Chemistry, Hyderabad. 3Professor and HOD, Department of Bio Chemistry Government Medical College, Suryapet, Telanagana. 4Consultant in Krishna Institute of Medical Sciences, Department of Bio Chemistry, Minister Road, Secunderabad
Abstract Background: Polycystic ovary syndrome, is the most common endocrinopathy affecting women of reproductive age presenting with amenorrhea, infertility, features of hyperandrogenemia, signs of metabolic disturbances like insulin resistance and dyslipidemia. Insulin resistance is a common feature in obese and, to a lesser extent, lean women with PCOS; Insulin signaling in the peripheral tissue is initiated through binding and activation of its cell-surface receptor, followed by a cascade of phosphorylation and dephosphorylation events, second messenger generation, and protein-protein interactions that result in diverse metabolic events. Methods and materials: The present study was done at Gandhi Hospital and Medical College, Secunderabad. 50 PCOS patients and 50 controls attending Obstetrics and Gynaecology Out Patient department were included in this study and blood samples collected was analysed for IRS2 Gly1057Asp polymorphism by PCR – RFLP method, Insulin Resistance calculated, and serum lipid profile levels were analysed in Autoanalyzer. Results: The mean age of cases was 25.7 years and mean age of the controls was 27.2 yrs. Slightly higher mean BMI, waist/hip ratio was observed in cases than in controls was statistically significant p-value <0.001. High mean Insulin resistance was recorded in cases (4.49) than in controls (2.2). The difference in mean Insulin resistance between the two groups is statistically significant (p-value <0.001). serum total cholesterol, triglycerides, LDL were higher in cases as compared to controls where as HDL was lower. Presence of IRS2 Gly1057Asp Polymorphism has been evaluated between the two groups. 35% of cases had 2 sets of polymorphic D allele (homozygotes, DD), 50% subjects with 1 polymorphic D allele (heterozygotes, DG) and 15% cases with normal alleles (GG).Conclusion: The present study, suggests that PCOS women have higher indices of obesity and central adiposity ie; BMI, waist circumference and waist/hip ratio, insulin resistance and lipid profile parameters as compared to age matched healthy non PCOS controls. Moreover, higher proportion of patients with atleast one polymorphic allele (homozygous DD or heterozygous DG) in the IRS2 gene (Gly1057Asp) had abnormal BMI and normal BMI was more frequent in the patients with Normal homozygous alleles (GG). Key Words: Poly cystic ovary syndrome, Insulin resistance, IRS2 gene polymorphism abnormality.
INTRODUCTION Polycystic ovary syndrome (PCOS), also called hyperandrogenic anovulation, or Stein-Leventhal syndrome, is the most common endocrinopathy affecting women of reproductive age 1 with a prevalence estimated to be 4-25% depending on the diagnostic criteria used 2,3 One of the fascinations of PCOS is that it is no longer just a gynecological curiosity , but a syndrome in its full blown form that can affect almost every organ in the female body from the hypothalamus to the hair follicles and the pituitary to the pancreas, from adolescence to menopause. PCOS patients may present with amenorrhea, infertility, features of hyperandrogenemia, signs of metabolic disturbances like insulin resistance (IR) and dyslipidemia. The IRS-2 gene is located on chromosome 13q34 and encodes a protein of 1,354 amino acids. The most common variant Gly1057Asp (rs1805097) in the IRS-2 gene has been reported to influence susceptibility to IR and type 2 diabetes in PCOS women. It was also shown that women with IRS-2 homozygous Asp variant may be considered as a risk factor for PCOS and need early detection to prevent further complications 4. However, the results of different studies from various countries were in considerable disagreement and, therefore, the role of these variants in the pathogenesis of insulin resistance and PCOS remains debatable. Insulin Resistance is also considered to play a role in causing abnormalities in lipid profile. It is estimated that 70% of women with PCOS have at least one abnormal lipid constituent 5. Obese women with PCOS are more prone to dyslipidemia, particularly elevated triglycerides (TG) and decreased high-density lipoprotein cholesterol (HDL-C) 6, 7. Some studies are suggestive of significantly lower levels of HDL-C in PCOS women compared to weight-matched controls 8. However, in other investigations, no difference was observed in lipid profile between PCOS women and control participants 9, 10. Therefore, due to the paucity of studies in the Indian population correlating IRS2 gene polymorphism with insulin resistance and dyslipidemia the present study was undertaken to investigate if IRS-2 Gly1057Asp influences insulin resistance and lipid profile in PCOS women.
OBJECTIVES
The present study was done at Gandhi Hospital and Medical College, Secunderabad after being approved by Institutional Ethics committee of Gandhi Hospital, Secunderabad. PCOS patients and controls attending Obstetrics and Gynaecology Out Patient department are taken into this study. A total of fifty cases, diagnosed as PCOS and fifty controls during the period from March 2014 to October 2015 were included in the study. In this study IRS2 Gly1057Asp polymorphism, Insulin Resistance, and serum lipid profile levels were analysed in blood samples from 50 PCOS patients and 50 controls at Clinical Chemistry laboratory and Microbiology laboratory, Gandhi hospital, attached to Gandhi medical college, Secunderabad. PCOS patients in the age group 18 – 45 years, new and old cases diagnosed according to Rotterdam criteria were included in the study. Presence of any two out of the three following Criteria required (i) Oligo- and/or anovulation (<8 menstrual periods per year), (ii) Clinical and/ or biochemical signs of hyperandrogenism, including hirsutism (Ferriman-Gallwey score >8) and (iii) Polycystic ovaries on sonography (i.e. at least 1 ovary containing 12 or more peripheral follicles measuring 2-9 mm in diameter and/or ovarian volume of at least 10 mL). Type 1 Diabetes mellitus, Cushing’s syndrome, Congenital adrenal hyperplasia, Androgen secreting tumors, Patients on anti-obesity drugs and diet were excluded. We measured height and weight of the patients to calculate BMI, waist circumference and hip circumference to calculate waist/hip ratio, estimated IRS2 Gly1057Asp polymorphism, fasting Insulin, fasting glucose to calculate Insulin Resistance and serum lipid profile levels (TC, TG, HDL, LDL, VLDL) in the present study. Statistical analysis was based on two sample unequal variance ‘t’ test and comparison of percentages of proportions using Microsoft excel software. Values were analysed in terms of mean, standard deviation, unpaired ‘t’ test and percentages. P value was considered strongly significant if <0.01.
RESULTS The cases and controls were divided into 4 groups based on age (<20 yrs, 21 – 25 yrs, 26 – 30 yrs, >30yrs).There were 8 cases <20 yrs of age, 20 cases between 21- 25 yrs, 13 cases between 26- 30 yrs, and 9 cases > 31 yrs. The maximum number of cases were in the age group of 21 – 25yrs (40%). The mean age of cases was 25.7 yrs and mean age of the controls was 27.2 yrs with Standard deviation (SD) 4.79 and 4.74 respectively. The p-value obtained on comparing the mean age of cases and controls was not significant (p-value >0.001). Slightly higher mean BMI was observed in cases than in controls. The difference in mean BMI between the case (26.3 kg/m2) and control (24.97 kg/m2) groups was statistically significant (p-value <0.001). Slightly higher mean Waist Circumference was recorded in cases (95.44 cm) than in controls (81.2 cm) and the difference in mean Waist Circumference between the two groups was statistically significant (p-value <0.001). Slightly higher mean Waist/Hip Ratio was recorded in cases (0.92) than in controls (0.82). The difference in mean Waist/Hip Ratio between the two groups was statistically significant (P<0.001). High mean Insulin resistance was recorded in cases (4.49) than in controls (2.2). The difference in mean Insulin resistance between the two groups is statistically significant (p-value <0.001). Slightly higher mean Serum Total Cholesterol level was recorded in cases (216 mg/dl) than in controls (178 mg/dl). The difference in mean Serum Total Cholesterol levels between the two groups was statistically significant (p-value <0.001). Slightly higher of mean Serum Triglycerides level was recorded in cases (137 mg/dl) than in controls (113 mg/dl). The difference in mean Serum Triglycerides level between the two groups was statistically significant (p-value <0.001). Comparatively lower level of mean Serum HDL Cholesterol was recorded in cases (37 mg/dl) than in controls (45 mg/dl). The difference in mean Serum HDL Cholesterol level between the two groups was statistically significant (p-value <0.001). Comparison of Serum LDL Cholesterol levels between the case and control groups was carried out. A comparatively higher level of mean Serum LDL Cholesterol was recorded in cases (142 mg/dl) than in controls (109 mg/dl). The difference in mean Serum LDL Cholesterol level between the two groups was statistically significant (p-value <0.001). Comparatively higher level of mean Serum VLDL Cholesterol was recorded in cases (26.9 mg/dl) than in controls (22.6 mg/dl). However, the difference in mean Serum VLDL Cholesterol level between the two groups was not statistically significant (p-value > 0.001). Presence of IRS2 Gly1057Asp Polymorphism has been evaluated between the two groups. There were 7 out of 20 cases with 2 sets of polymorphic D allele (homozygotes, DD), 10 subjects with 1 polymorphic D allele (heterozygotes, DG) and 3 cases with normal alleles (GG).
Table 1: consolidated table for comparision of mean of variables in cases and controls
Table 2: Consolidated table for comparison of gene polymorphism with other parameters in PCOS cases
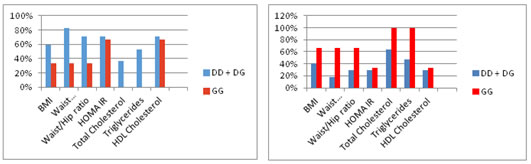
Graph 1 Graph 2 Graph 1: Comparison of percentages of PCOS women with Abnormal parameters in DD+DG and GG subgroups. Graph 2: Comparison of percentages of PCOS women with Normal parameters in DD+DG and GG subgroups DISCUSSION In the present study, gene polymorphism in PCOS women is compared with their anthropometric and biochemical parameters viz; BMI, Waist circumference, Waist/Hip ratio, HOMA IR index, Total Cholesterol, Triglycerides and HDL cholesterol levels. For comparison of parameters, the cases have been divided into two groups: Group 1 - homozygous polymorphic + heterozygous polymorphic cases (DD+DG) constituting 85% and Group 2 -homozygous normal (GG) cases constituting 15% of PCOS cases in whom IRS2 G1057D gene polymorphism is analyzed. Percentages of proportion of each parameter are compared between the two groups. Ramanand et al (2013) study on 120 Indian PCOS women showed that PCOS was present in both obese and non-obese subjects, of whom 75% had abnormal BMI (28% overweight + 47% obese) and mean BMI was 27.32 ± 6 11. In another study by Thathapudi S et al (2014) in 204 PCOS women, 70% had abnormal BMI with mean BMI of 27.25 ± 5.02 and 26.0 ± 4.1 in their subgroups 12. These studies are in agreement with the present study where 74% have abnormal BMI (24% overweight + 50% obese) and the mean BMI is 26.3 ± 4.9. thus, only 26% have normal BMI. Asian Indians have higher percentage body fat, abdominal adiposity at lower BMI levels due to the difference in body composition ie, higher percentage body fat, abdominal adiposity. Hence they are more predisposed to develop insulin resistance and cardiovascular risk factors as compared to other ethnic groups. Several studies have found higher mean waist circumference and waist/hip ratio in PCOS women as compared to age matched healthy controls. Thathapudi S et al in a study on South Indian PCOS women found higher mean waist circumference and standard deviation values 37.10 + 4.28, as compared to the parameters in controls 30.36 + 3.30 inches.13 Similarly, waist/hip ratio was higher in PCOS women 0.94+ 0.04 cm as compared to the control values 0.79 + 0.05 cm. Kandapa Charnvises et al in Bangkok, Thailand studied anthropometric parameters in 121 PCOS women of mean age 29.1±6.1 years attending their Reproductive Endocrinology and Infertility Unit. The mean age and standard deviation of body mass index (BMI) and waist/hip ratio (WHR) was, 27.4±6.8 kg/m2 and 0.84±0.6 respectively.14 In the present study also PCOS cases have higher waist circumference (mean ± SD 95.44 ± 15.2 cm) and waist/hip ratio (mean ± SD 0.92 ± 0.13) more than the cut off levels for Asians – (waist circumference >80cm and waist/hip ratio >0.8) as compared to the controls indicating greater visceral adiposity in them. In healthy women with normal body weight and preserved insulin sensitivity, the adipocytes release small amounts of free fatty acids (FFAs) and have a normal activity of the lipoprotein lipase (LPL). In obese women there is increased production of FFA and decreased activity of LPL due to prominent insulin resistance. In addition to these conditions, high androgen levels additionally worsen disturbances in the lipid metabolism. The dyslipidaemia in PCOS patients occurs independent of BMI, however there is a synergistic deleterious effect of obesity and insulin resistance in PCOS analogous to that seen in type 2 diabetes. The causes of dyslipidaemia in PCOS are again multifactorial. Insulin resistance appears to have a pivotal role by stimulating lipolysis and altering expression of lipoprotein lipase and hepatic lipase. As with studies of insulin action, studies of lipid metabolism in PCOS have been confounded by differences in body weight and ethnicity between patient and control groups. The study of Cupisti et al. analysed differences among the 8 most frequent phenotypes of PCOS women with regard to metabolic changes in terms of markers of lipid profile (LDL, HDL, cholesterol, and triglycerides).15 Only HDL was significantly lower in women with hyperandrogenemia, hirsutism, and oligomenorrhea than in controls and in comparison with women with oligomenorrhea and polycystic ovaries. This is in agreement with the present study where among all the parameters of lipid profile, abnormal HDL is the most frequently found proportion, 64% of PCOS cases. In the present study, 80% of PCOS women have at least one abnormality in the lipid profile parameters. A study conducted by Sidhwani et al demonstrated that independent of body weight, PCOS was associated with changes in lipoprotein profile that increases risk for cardiovascular disease. They also demonstrated an increase in LDL particle number and a borderline decrease in LDL size.16 Hyperandrogenism may lead to the abnormalities in lipoprotein profile by working directly on the liver, or it may alter the body composition by favoring central adiposity. Some investigators have found that LDL and HDL changes in PCOS can be accounted for by obesity and that only modest increases in total triglyceride levels appear secondary to PCOS-related insulin resistance. Cristian-Ioan IUHAS et al in Romania studied lipid Parameters in Patients with Polycystic Ovary Syndrome and healthy age matched controls. In their study, PCOS patients had higher levels of the total and LDL cholesterol and low HDL-cholesterol when compared with healthy women. 17 An increased risk of dyslipidemia has been demonstrated in PCOS. Applying the National Cholesterol Education Program guidelines, nearly 70% have at least one borderline or elevated lipid level, although many women with PCOS have entirely normal lipid profiles 64–66. Lipid abnormalities commonly found in these patients are reduced high density lipoprotein-cholesterol (HDL-C), increased triglycerides, and increased low density lipoprotein-cholesterol (LDL-C). A meta-analysis by Wild et al evaluated the difference in lipoproteins from women age 18–45 years with PCOS and compared them to controls. 18 Triglycerides were 26.39 mg/dL (95% CI 17.24–35.54) higher and HDL-C was 6.41 mg/dL (95% CI 3.68–9.14) lower in PCOS. LDL-C was 12.60 mg/dL (95% CI 9.51–15.69) higher inPCOS. In addition, studies have revealed the presence of highly atherogenic small dense low density lipoprotein (LDL) in women with PCOS. Obesity and insulin resistance promote a high hepatic triglyceride content, which, in turn, leads to increased hepatic secretion of very low density lipoprotein (VLDL) particles. There is also associated with reduced clearance of VLDL particles and chylomicrons by reducing the activity of lipoprotein lipase, increasing levels of apolipoprotein C-III, and impairing apolipoprotein E-mediated clearance of triglyceride rich lipoproteins. Also, hepatic triglyceride content determines the size of the VLDL particles produced by the liver. When the hepatic content of triglycerides is high, larger VLDL particles are produced. Djuro Macut et al, determined the values of key lipid and lipoprotein fractions in 75 PCOS women, and 56 age- and BMI-matched controls, and their possible relation to insulin resistance. PCOS patients compared with controls had increased indices of insulin resistance, basal insulin (p < 0.001), and HOMA index (p < 0.001), and worsened insulin resistance-related dyslipidemia with decreased HDL cholesterol (p < 0.01), elevated triglycerides (p = 0.010), and pronounced LDL oxidation (p < 0.001). In conclusion, characteristic dyslipidemia of insulin resistance were present only in women with PCOS and not in controls. 19 In the present study, proportion of PCOS cases with abnormal lipid profiles in both the subgroups is variable. Most of the PCOS patients in the subgroup DD+DG have normal serum total cholesterol (<200mg/dl) and triglycerides(<150 mg/dl) levels – 64% and 47% respectively as compared to the lesser proportions of 36% and 53% patients with abnormal levels of TC and TG in the group. All PCOS cases with GG allele have normal Serum Total Cholesterol and Triglyceride levels. However, HDL cholesterol levels are consistently abnormal (<40 mg/dl) in greater proportion of PCOS women in both the subgroups – 71% in DD+DG and 66.6% in GG but there is no significant difference of proportions between the two sub groups (4.4%).
CONCLUSIONS The present study, suggests th,at PCOS women have higher indices of obesity and central adiposity ie; BMI, waist circumference and waist/hip ratio, insulin resistance and lipid profile parameters as compared to age matched healthy non PCOS controls. Moreover, higher proportion of patients with atleast one polymorphic allele (homozygous DD or heterozygous DG) in the IRS2 gene (Gly1057Asp) had abnormal BMI and normal BMI was more frequent in the patients with Normal homozygous alleles (GG). The D allele though frequently associated with insulin resistance (higher HOMA IR index) has more correlation with central adiposity (waist circumference) as already corroborated by previous studies. Among aberrations in lipid profile, low HDL cholesterol is the frequent finding compared to the other abnormal parameters viz; high Total Cholesterol and Triglycerides. However, HDL cholesterol abnormality may not be affected by the polymorphic alleles as there was no significant difference between the two groups (DD+DG and GG). Presence of the polymorphic D allele may be associated with higher Serum Total Cholesterol and Triglycerides levels. In the present study, the PCOS cases with normal IRS2 alleles (GG) have normal lipid profiles.However, these findings need to be confirmed in the future with studies in larger population with ethnic differences.
REFERENCES
.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home