|
Table of Content - Volume 13 Issue 1 - January 2020
Study of serum homocysteine in patients of type-2 diabetes mellitus with and without hypertension
A A Junaidi*, G S Manoorkar**
1Lecturer, Department of Biochemistry, Tata Memorial Hospital, Mumbai, Maharashtra, INDIA. 2Associate Professor, Department of Biochemistry, Dr. S. C. Government Medical College, Nanded, Maharashtra, INDIA. Email: drganeshmanoorkar@yahoo.in
Abstract Background: Diabetes mellitus (DM) is a complex disease characterized by chronic hyperglycemia, metabolic abnormalities, and long-term macro and micro vascular complications. It is one of the leading global health issues of the 21st century. Homocysteine (Hcy) is a non-protein sulfur containing amino acid. The elevation of homocysteine occurs in patients with type 2 DM. Homocysteine is thought to help regulate glucose metabolism and has been suggested to contribute to the atherosclerotic process of DM. Elevated concentration of serum homocysteine is expected to enhance the production of its oxidation products such as Hcydisulfides and Hcythiolactone. These products lead to endothelial cell damage by extravagant sulfation of collagen which in turn aggravates the progression of thrombosis and arteriosclerosis. Therefore, the present study was conducted to know the correlation of serum homocysteine in patients of type 2 DM associated with and without hypertension. Aims and Objectives: To study the relationship between serum homocysteine level in patients of type 2 diabetes mellitus with hypertension and without hypertension. Material And Methods: The present study was carried in the department of Biochemistry Grant Government Medical College and JJ hospital Mumbai. The study was conducted for a period of 2 years from June 2016 to June 2018. In our study 120 diabetic patients were enrolled and were divided in two groups- cases and controls. Group I (Case) - Diabetes with hypertension Group-II (Control) - Diabetes without hypertension. The serum homocysteine level was estimated by enzymatic method. Results: The average homocysteine level among cases was 20.51 ± 6.92 µmol/L and among control was 17.13 ± 7.11 µmol/L. Significant difference (p=0.01) was seen in the homocysteine level among cases and control. Conclusion: The average homocysteine level was significantly high in type 2 DM patients with hypertension in comparison to type 2 DM patients without hypertension. Key Words: Type-2 diabetes mellitus, hypertension, Homocysteine, arteriosclerosis.
INTRODUCTION Diabetes mellitus (DM) is a complex disease characterized by chronic hyperglycemia, metabolic abnormalities, and long-term macro and micro vascular complications. It is one of the leading global health issues of the 21st century. There has been a drastic increase in the global prevalence of diabetes mellitus in the past few decades. There were 108 million people with DM in 1980, and this number increased fourfold in 2014 according to WHO estimates. In 2017, about 425 million adults were diagnosed with DM, and it is estimated that about 629 million will be living with DM by 2045 1. India is one of the top countries with the largest number of people having DM. In 2017, nearly 73 million people were diagnosed with DM. The rapid shift in the Indian economy is the factor behind the increase in the prevalence of DM. If this trend continues, by 2045, almost 134 million people will have DM. About 79% of the people with DM live in low- and middle-income countries 2.Homocysteine (Hcy) is a non-protein sulfur containing amino acid. The single source of homocysteine in humans is the demethylation of the essential amino acid, methionine (Met), via two intermediate compounds, S-adenosylmethionine (SAM) and S-adenosylhomocysteine (SAH)4. Homocysteine is thought to help regulate glucose metabolism5. High homocysteine levels have been reported in diabetic patients. Elevated concentration of serum Homocysteine (Hcy) is expected to enhance the production of its oxidation products such as Hcydisulfides and Hcythiolactone. These oxidative products leads to the endothelial cell damage by extravagant sulfation of collagen which in turn aggravates the progression of thrombosis and arteriosclerosis6. Hyperhomocysteinaemia (HHcy) in type 2 DM may contribute to the development of chronic vascular complications and hypertension. Often called as a silent killer, hypertension places stress on the target organs, such as kidneys, eyes and heart, causing them to deteriorate over time. Hypertension contributes to 75% of all strokes and heart attacks7. Several studies, some population-based, found plasma homocysteine levels linked to blood pressure, especially systolic pressure. Therefore, the present study was conducted to know the correlation of serum homocysteine in patients of type 2 diabetes mellitus associated with and without hypertension.
AIMS AND OBJECTIVES To study the relationship between serum homocysteine level in patients of type 2 diabetes mellitus with hypertension and without hypertension.
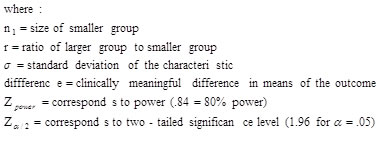
MATERIAL AND METHODS The present study was carried in the department of Biochemistry Grant Government Medical College and JJ hospital Mumbai. Study Design This was a case control study. Study duration The study was conducted for a period of 2 years from June 2016 to June 2018. Study population/ source of data Samples collected from OPD who fulfill the inclusion and exclusion criteria Using this reference for sample size calculations, and Confidence Interval (2-sided): 99% Power: 80% Formula for Sample size calculation for comparing two means:
Sample size: In our study 120 diabetic patients were enrolled and were divided in two groups- cases and controls. Group I (Case) - Diabetes with hypertension Group-II (Control) - Diabetes without hypertension. Ethical considerations: The study was initiated after obtaining approval from the institutional ethics committee and department of Biochemistry. Inclusion criteria: Patients of both gender between age >40 years Patients with type 2 diabetes mellitus with hypertension Patients with type 2 diabetes mellitus without hypertension. Exclusion criteria: Patients below 40 years of age. Patients with Type-1 diabetes mellitus. Patients with renal disease, cardiac disease and liver disease Pregnant and lactating females Patients with significant renal, cardiac, neoplasm Patients taking insulin and on medication of metformin and glitazones. Statistical analysis: Data was collected in Microsoft excel version 2015. Descriptive statistics for quantitative variables was represented as mean +/- SD. Qualitative variables was represented as frequency and percentages. Graphical representations were done wherever applicable. Level of significance will be considered as P < 0.05. Software used for analysis was Graph pad prism. Collection of blood samples: Fasting blood sample of 120 patients was collected in vacuum evacuated plain tubes from cubital vein under aseptic precaution. It is then allowed to clot. All samples then centrifuged at 4500 rpm for 5min to obtain clear serum and plasma. The tests were done on same day after serum separation. The estimation of serum homocysteine level was done by Enzymatic method.
RESULTS
Table 1: Comparing homocysteine level in cases and control
The average homocysteine level among cases was 20.51 ± 6.92 µmol/L and among control was 17.13 ± 7.11 µmol/L.
DISCUSSION The average homocysteine level among cases was 20.51 ± 6.92 µmol/L and among control was 17.13 ± 7.11 µmol/L. Higher level of serum homocysteine was seen among the cases and controls. This was similar to the study conducted by Ramachandran L8 where higher homocysteine levels were found in type-2 DM with hypertension (p<0.001) as compared to control subjects. Kangabam N et.al9 in their study reported significant difference (p<0.0001) in serum homocysteine level in diabetic patient with cardiovascular morbidity (27.20±6.02 µmol/L) and those without cardiovascular morbidity (18.03±4.61 µmol/L). Qureshi, M10 in his study reported homocysteine levels were higher in the diabetic patients with hypertension than in the normotensive diabetic patients. Homocysteine levels are elevated in both systolic and diastolic hypertension. In one large and carefully conducted epidemiological study suggests, each 5 umol/l increase in plasma homocysteine level was associated with an increase in systolic and diastolic blood pressure by 0.7 and 0.5 mmHg in men and by 1.2 and 0.7 mmHg in women respectively, which was independent of renal function11. In addition, observations that homocysteine-lowering therapies with folic acid-based treatments have been followed by decreases in blood pressure raise the possibility that the link between homocysteine and blood pressure is causal, which is important since homocysteine levels can easily be lowered by folic acid-based regimens. Mechanisms that could explain the relationship between homocysteine and blood pressure include homocysteine-induced arteriolar constriction, renal dysfunction, increased sodium reabsorption, and increased arterial stiffness11. The main proposed mechanism by which Hyperhomocysteinaemia produces hypertension and cardiovascular disease is through homocysteine mediated damage to vascular smooth muscle and endothelial cells. This damage in turn, leads to a loss of arterial vasodilation, vascular integrity, and thus increased blood pressure (BP) and accelerated arteriosclerosis. This hypothesis has been supported by findings of both in vitro and in vivo basic science studies12.
CONCLUSION The average homocysteine level was high in type 2 DM patients with hypertension in comparison to type 2 DM patients without hypertension which may in turn may aggravates the progression of thrombosis and arteriosclerosis.
REFERENCES
Policy for Articles with Open Access
|
 Home
Home