|
Table of Content - Volume 19 Issue 2 - August 2021
Total cholesterol/high density lipoprotein-cholesterol ratio as an indicator of Dyslipidemia in hypothyroidism
Chandrika N1*, Devaki R N2
1Associate Professor, 2Professor & HOD, Department of Biochemistry, CIMS, Chamarajanagar, INDIA.
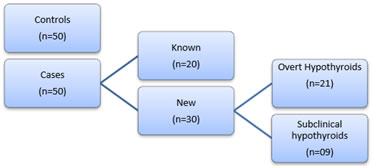
Abstract Background: The thyroid hormones are involved in controlling metabolism, growth and functions of various organ systems of our body. Hypothyroidism, a very common endocrinopathy features reduced production of thyroid hormones. In hypothyroidism we encounter abnormal circulating lipid fractions which is termed as ‘Dyslipidemia’. The coexistence of dyslipidemia and hypothyroidism is associated with development of atherosclerosis. Aim: This research is undertaken to assess the potential of TC/HDL-C ratio to disclose dyslipidemia in hypothyroidism. Methodology: The study consists of two major groups, the ‘Cases’ comprising of Fifty hypothyroid patients and ‘Controls’, with fifty age and gender matched healthy adults. The Cases are further subdivided into Twenty ‘Known cases’ of Hypothyroid patients, already receiving treatment and thirty ‘New cases’. The ‘New cases’ sub group further is subdivided as Twenty-one ‘Overt hypothyroids’(OH) and nine ‘Subclinical Hypothyroids’ (SCH). The Biochemical parameters estimated in all subjects of the study includes, Serum TSH, T3, T4, Total Cholesterol (TC) and High density lipoprotein-cholesterol(HDL-C). TC/HDL ratio was then calculated . Result: The study shows a significant elevation (p = 0.05) in the TC/HDL-C ratio in hypothyroid patients (3.67 ± 1.02) when compared to healthy controls (3.29 ± 0.95). TC/HDL-C ratio is more elevated in OH (4.01 ± 1.28) than in SCH (3.46 ± 0.92). The levels in ‘New cases’ sub-group and OH sub sub group have significantly higher ratio than in healthy controls (p = 0.02 and p = 0.01 respectively). TC/HDL-C ratio value in “known cases’ group who are those hypothyroid patients on Levo-thyroxine therapy is (3.40 ± 0.61) less than those who are newly diagnosed. Conclusion: TC/HDL-C ratio is not only raised in hypothyroid patients but it is seen increasing with severity and prolonged duration of disease. The calculation of TC/HDL-C ratio should be routinely put into practice to detect hypothyroid patients with dyslipidemia. Key words: TC/HDL ratio, Hypothyroidism, Dyslipidemia, Cardiovascular disease.
INTRODUCTION The thyroid gland is one of the largest endocrine glands in the human body.1 The main hormones secreted by the thyroid gland are triiodothyronine (T3) and thyroxine (T4). The thyroid gland, anterior pituitary and hypothalamus together constitute an auto-regulatory nexus known as the hypothalamic-pituitary-thyroid axis. Thyrotropin-releasing hormone (TRH) from the hypothalamus, thyroid-stimulating hormone (TSH) from the anterior pituitary gland, and thyroid hormones work synchronously to maintain metabolic homeostasis.2 The thyroid hormones are involved in controlling metabolism, growth and functions of various organ systems of our body. Thyroid disorders are the second most common type of endocrinopathies after diabetes mellitus in the world.3 Around 200 million people across the world have different types of thyroid disorders and among them 50 % are un-diagnosed. The reason behind this being the vague manifestations of thyroid disorders in early stage of the disease which include depression, obesity and menstrual irregularities. Therefore thyroid disorders are rightly called the ‘silent epidemic’. Approximately 5% of the global population have hypothyroidism and 2% have hyperthyroidism.4 Prevalence of hypothyroidism in India is 11 %.5 Hypothyroidism features reduced production of thyroid hormones. Primary hypothyroidism involves loss of thyroid gland function which occurs most commonly due to autoimmunity or decreased thyroid hormone synthesis as seen in iodine deficiency. Central or secondary hypothyroidism occurs because of insufficient stimulation of a normal gland, by the TRH or TSH hormones due to hypothalamic or pituitary disease. Hypothyroidism can also be classified as Overt or Clinical hypothyroidism(OH) and Sub Clinical hypothyroidism(SCH). Both the conditions are diagnosed based on laboratory findings, where in Overt hypothyroidism presents with elevated TSH and decreased T3 and T4 levels. The term ‘subclinical hypothyroidism’ is a type of primary hypothyroidism where there is an elevated thyroid-stimulating hormone (TSH) concentration with normal serum thyroxine (T4) and triiodothyronine (T3) concentrations.6 Thyroid hormones influence energy metabolism. They increase basal energy expenditure by acting on protein, carbohydrate and lipid metabolism. Thyroid hormones affect synthesis, mobilization and degradation of lipids.7 The balancing act by thyroid hormones between synthesis and clearance of cholesterol maintains the normal serum cholesterol levels in euthyroid state. In hypothyroidism we encounter abnormal circulating lipid fractions which is termed as ‘Dyslipidemia’. The dyslipidemia in hypothyroidism is caused as a result of increased synthesis compared to degradation rate causing elevated levels of Total Cholesterol (TC), mainly Low density lipoprotein-cholesterol (LDL-C). The coexistence of dyslipidemia and hypothyroidism is associated with development of atherosclerosis.8 The traditional way of assessing the lipid status of an individual demands a routine lipid profile assay which includes estimation of serum Total cholesterol, Low density lipoprotein cholesterol, High density lipoprotein cholesterol (HDL-C) and triglycerides(TG). A simple fraction of Total cholesterol by High density lipoprotein cholesterol can come handy in predicting the prevailing dyslipidemia when compared to a whole lipid profile testing. Recent studies have acknowledged that the use of TC/HDL-C ratio in detecting dyslipidemia which for long has been underestimated. TC/HDL-C ratio is found to be predictor of Acute myocardial infarction in middle aged women in one of the recent studies.9 There are not many literatures available which evaluates TC/HDL-C ratio levels in hypothyroidism. This research is undertaken to reminisce the caliber of TC/HDL-C ratio to disclose dyslipidemia in hypothyroidism. METHODOLOGY The study was undertaken between December 2019 to September 2020 in District Hospital, Chamarajanagar. The study design consists of two major groups. The first one is group of ‘Cases” with fifty hypothyroid patients who visited General Medicine Out patient clinic of the Hospital. The age group of the subjects in this group extended from 18 to 55 years. We inducted fifty age and gender matched healthy adults into to the second group assigned the ‘Controls”. Among the ‘Cases’, twenty were Known Hypothyroid patients who were on Levothyroxine therapy and thirty were the Newly Diagnosed patients. Twenty one of the newly diagnosed hypothyroid patients had Overt hypothyroidism (Elevated TSH and decreased T3 and T4 levels) and nine had Subclinical hypothyroidism (TSH levels which was found to be between 4.2 and 10.0 μIU/ml and T3, T4 values within the normal reference ranges). Pregnancy, patients with any medical or surgical illness were promptly excluded from our study. The Institutional Ethics Committee approval was obtained prior to the commencement of the study. An informed consent was taken from all the subjects recruited into the study. The normal reference range that was followed to include subjects in ‘Control’ group is as follows: TSH 0.4 to 4.2 μIU/ml, T3 70 to 204 ng/dl and T4 of 5.5 to 11μg/dl . Figure 1 represents the study group and their different sub divisions. Thyroid profile tests were processed on Chemiluminescence immunoassay based autoanalyzer Maglumi-1000. The venous blood sample of both hypothyroid patients and healthy controls were drawn under all aseptic precautions. This sample was utilized to estimate serum total Cholesterol and HDL-C levels. Both the investigations were analyzed on photometry based fully automated general chemistry analyzer from Transasia company, ERBA XL-640. Serum total cholesterol was estimated by Cholesterol oxidase method, serum HDL-C was measured by Direct method. After estimation, the value of TC was divided by HDL-C levels to get TC/HDL-C ratio for each of the subjects in our study. The values of the lipid fractions in both groups were tabulated and compared using suitable statistical tool. Statistical analysis: The mean value and Standard deviation for all the biochemical parameters was calculated. The Mean ± SD between the cases and controls were compared using student ‘t’ test. The correlation between biochemical parameters were performed using Pearson’s correlation analysis. All statistical analysis was done at 5% level of significance. RESULTS Table 1 shows the Mean and Standard deviation values of various Biochemical parameters in Cases and Control groups of our study Table 2 compares and specifies the significance level when TC/HDL-C ratio of Control group is compared with the different sub groups in our research Table 1: Comparative statement of Biochemical investigations of the two major study groups
Table 2: Comparative statement of TC/HDL-C ratio between Control group and various Sub-groups of the study
Figure 1: Study groups and their sub-divisions
DISCUSSION In the present study we have selected TC/HDL-C ratio as a tool to study dyslipidemia in hypothyroidism. We have been successful to a certain extent in the same endeavor as the study shows a significant elevation (p = 0.05) in the TC/HDL-C ratio in hypothyroid patients (3.67 ± 1.02) when compared to healthy controls (3.29 ± 0.95). This is in line with certain studies which were undertaken to establish TC/HDL-C capacity as marker of dyslipidemia, though not in hypothyroidism.10 The deterioration of thyroid function is directly proportional to the degree of dyslipidemia. Our study findings show that TC/HDL-C ratio is more elevated in OH (4.01 ± 1.28) than in SCH (3.46 ± 0.92). These finds are in accordance with findings seen in study by Dubey et al. who also have shown correlation between failing thyroid function and worsening circulating lipid fractions.11 The levels in ‘New cases’ sub-group and OH sub sub group have significantly higher ratio than in healthy controls (p = 0.02 and p = 0.01 respectively). Interestingly we are also able to prove that Thyroid replacement therapy has positive effects in controlling the lipid derangement as the TC/HDL-C ratio value in “known cases’ group who are those hypothyroid patients on Levo-thyroxine therapy is less than (3.40 ± 0.61) those who are newly diagnosed. A similar improvement in lipid status after levo-thyroxine treatment has been reported earlier study.12 Thyroid hormones influence lipid metabolism. They enhance cholesterol uptake by cells by acting on LDL receptors. Thyroid hormones promote lipolysis and increase circulating non- esterified fatty acids. They also enhance activity of enzymes of lipoprotein metabolic pathways like Hepatic lipase, lipoprotein lipase and Cholesterol ester transport protein (CETP).7 In hypothyroidism the observed lipid profile shows an elevation of TC and LDL-C, Apo A and B, Lp(a) and normal or elevated triglyceride and HDL levels. The degree of TSH elevation is also an important determinant of dyslipidemia in hypothyroidism. The course of duration of the disease is directly related to the severity of lipid derangement.13 Dyslipidemia is characterized either by abnormal quantity or quality of lipoproteins in plasma. It may feature increased lipid particles circulating in the blood or impaired biochemical composition of lipid particles which may be well within their reference ranges. This can lead to the development of atherosclerotic disease. Studies have proved that the increased concentration of total cholesterol (TC) and Low Density Lipoprotein cholesterol (LDL-C) in serum, are independent cardiovascular disease risk factors.14 The pathophysiology of hypothyroidism culminates in dyslipidemia leading to cardiovascular event. The current study has made use of two lipid parameters to assess the abnormal lipid pattern in hypothyroid patients who are at different stages of the disease. Though HDL-C levels is stated to be normal or elevated in hypothyroidism, the increase in TC is so enormous that the TC/HDL-C ratio obviously stands raised. The testament of this fact should be made use of and calculation of TC/HDL-C ratio should be routinely put into practice to detect hypothyroid patients with dyslipidemia. Not only it is cost effective but also patient compliant as it doesn’t require fasting blood sample to analyze TC and HDL-C levels. Once dyslipidemia is detected the progression to untoward cardiovascular event can be alleviated by proper and timely intervention. The limitation of the study is its small sample which could not accommodate to know the correlation between TSH and TC/HDL-C ratio. We recommend the researchers to take up the same for their future ventures.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home