Official Journals By StatPerson Publication
|
Table of Content - Volume 4 Issue 1 - October2017
Glycated hemoglobin in diagnosis of diabetes mellitus: Descriptive clinical study
Vinod V Wali1, Kirankumar Akka2*
1Associate Professor, Department of Biochemistry, Smt Kashibai Navale Medical College and General Hospital, Pune, Maharashtra, INDIA. 2Assistant Professor, Department of Biochemistry, MRMC, Gulbarga, Karnataka, INDIA. Email: docvinod80@yahoo.com
Abstract Background: Type 1 and type 2 are the two broad categories of diabetes mellitus. Insulin deficiency as a result of autoimmune immunodeficiency leads to Type 1 Diabetes. Type 2 diabetes mellitus is a heterogeneous group of disorders characterized by variable degree of insulin resistance, impaired insulin secretion and increased glucose production. Common phenotype of hyperglycemia in type 2 diabetes mellitus is caused by distinct type of genetic and metabolic defect in insulin action and / or secretion. Methodology: A hospital based prospective study was undertaken among the patients attending the outpatient department. About 133 patients who were visiting the OPD with symptoms suggestive of Diabetes were included as sample size. An informed Bilingual consent was obtained before the study was started. Results: About 69.6% of those with abnormal HbA1c had abnormal FBS and 26.7% had normal FBS. About 30.4% of those with normal HBA1c had abnormal FBS. About 73.3% of subjects with normal FBS also had normal HbA1c.Conclusion: OGTT requires second blood sample and is therefore more costly and time consuming, bringing inconvenient in logistics and causes discomfort to the individuals. Keywords: HBA1c, FBS, OGTT
INTRODUCTION The International Diabetes Federation in 2012, noted that around 371 million diagnosed cases of Diabetes Mellitus around the world. About 50% of undiagnosed cases of diabetes are living in the communities. About 155 million cases of diabetes mellitus are living in China and India only. The prevalence of diabetes is low in Micronesia, Nauru, Mashal Islands with 8.3% and high in Kribhathi with a prevalence of 25% in 20 – 79 years age group.1 The Global statistics shows that about 187 million patients of diabetes mellitus are undiagnosed and African continent has highest number of such cases amounting to 81% of the total cases. In Middle East, North America, South East Asia and Western Pacific countries almost 50% of the cases are not diagnosed yet. Four patients of diabetes out of five cases live in low and middle income countries. About half of the people who die from diabetes are aged less than 60 years. Around 4.8 million people died and 471 billion USD were spent due to diabetes in 2012.2 India is often called as “Capital of diabetes of the world”. According to Diabetes atlas, around 63 million people with diabetes are living in India. The prevalence of the diabetes mellitus is around 9.01%. One million cases die due to diabetes mellitus in 20 – 79 years age group.3 During 1970s, the prevalence of diabetes mellitus among urban Indians was reported to around 2.1% and has increased to 12.1% now. In the year 2010, the prevalence fo diabetes mellitus in India was estimated to be 0.2% in the individuals aged less than 20 years and 11.3% among the individuals aged more than 20 years. The prevalence was 26.9% among the individuals aged more than 65 years.4 The available studies have shown that the prevalence of rate diabetes mellitus to be 2.4% in rural and 4 to 11% among the urban dwellers. The difference in prevalence of diabetes is often attributed to the industrialization and urbanization.5 The diabetes mellitus was considered as the diseases of middle ages initially. Nowadays, the type 2 diabetes mellitus is the disease of all age groups including the younger age groups and adolescents in high risk population. Type 2 Diabetes (noninsulin dependent diabetes, NIDDM) is the commonest form and it constitutes nearly 90% of the diabetic population in any country.5 Type 1 and type 2 are the two broad categories of diabetes mellitus. Insulin deficiency as a result of autoimmune immunodeficiency leads to Type 1 Diabetes. Type 2 diabetes mellitus is a heterogeneous group of disorders characterized by variable degree of insulin resistance, impaired insulin secretion and increased glucose production. Common phenotype of hyperglycemia in type 2 diabetes mellitus is caused by distinct type of genetic and metabolic defect in insulin action and / or secretion. The current classification of two types of diabetes mellitus is different from the previous classification i.e., insulin dependent diabetes mellitus (IDDM) and non-insulin dependent diabetes mellitus (NIDDM) where the terms are no longer used. Many people of type 2 diabetes mellitus requires insulin treatment for control of hyperglycemia and hence the term NIDDM created confusion. Age is not a criterion in the classification system. The autoimmune beta cell destruction can develop at any age and not necessarily before the age of 30. About 5 to 10% of people of type 1 diabetes mellitus can develop disease after the age of 30 years. Likewise diabetes mellitus is more typically developed with increase in age, but it also occurs in children, particularly in obese adolescents.6
METHODOLOGY A hospital based prospective study was undertaken among the patients attending the outpatient department. About 133 patients who were visiting the OPD with symptoms suggestive of Diabetes were included as sample size. An informed Bilingual consent was obtained before the study was started. The inclusion and exclusion criteria were as follows, Inclusion criteria
Exclusion criteria
A detailed clinical history was obtained from the patients. The detailed history suggestive of symptoms including polyuria, polydypsia, polyphagia and weight loss were recorded in a predesigned proforma. All the patients’ blood sample were sent for estimation of FBS, PPBS and HbA1c levels. HbA1c In the study HbA1c was measured by using Latex enhanced Immunoassay method. It is based on interactions between antigen molecules (HbA1c) and HbA1c specific antibodies coated on latex beads.
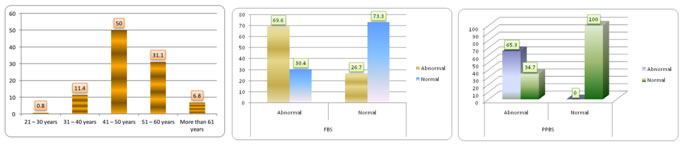
RESULTS Figure 1: Distribution of the study group according to age group; Figure 2: Distribution of the study group according to HbA1c and FBS levels; Figure 3: Distribution of the study group according to HbA1c and PPBS levels.
About 50% of the subjects in the study belonged to 41 – 50 years of age group. About 31.1% belonged to 51 – 60 years, 11.4% to 31 – 40 years and 6.8% to more than 60 years of age group. About 69.6% of those with abnormal HbA1c had abnormal FBS and 26.7% had normal FBS. About 30.4% of those with normal HBA1c had abnormal FBS. About 73.3% of subjects with normal FBS also had normal HbA1c. About 65.3% of the subjects with abnormal PPBS had abnormal HbA1c and 34.7% had normal HbA1c. All the patients with normal PPBS also had normal HbA1c.
DISCUSSION Diabetes is a common public health problem. The diagnosis of diabetes mellitus is mainly based on fasting and post prandial plasma glucose. Inclusion of HbA1c as a diagnostic test for diabetes has submitted rigorous examination upon the evidence based medicine. The cut off level of HbA1c is important in increasing the yield of diabetics. This study had shown that the HbA1c can be used as screening test and lower cut off levels can increase the yield of diabetic patients. However, recent onset diabetes or prediabetes could not be diagnosed using HbA1c. However, there are clear advantages of using HbA1c over oral glucose tolerance test (OGT). But this study is without limitations. The study methodology used is cross sectional study and sample size was not calculated which precludes the generalization of results. However, this study had brought out important factors in diagnosis of diabetes mellitus which can be an important area of further research. About 50% of the subjects in the study belonged to 41 – 50 years of age group. About 53.4% of the males and 43.2% of females belonged to 41 – 50 years age. Diabetes mellitus is a disease which mainly affects after 40 years. The results of this study also shown that majority of the study subjects were aged more than 40 years. In a similar study in China, the mean age of the study group was 54 years ranging from 48 – 61 years.7 In a similar study in Pakistan, the mean age of the 53.6 (± 13.7) years.8 In a study of comparison between the HbA1c and OGTT, the mean age of the study subjects was 53.6 years similar to the results of this study.9 In this study, about two third of the study subjects were males. In contrary to these study findings the most of the study subjects were females in a study in China.7 Azim et al have also found similar results in Pakistan.8 The mean (± SD) FBS levels of subjects of this study was 155.42 (± 44.99) mg /dl among all the subjects in this study. This study had shown age dependent increased fasting and post prandial blood sugar levels. The mean HbA1c levels in the study group was 7.57 (± 0.97) percent. The mean FBS levels was 5 mmols in similar study in China. The two hours PPBS was 6 mmols and HbA1c was 5.5 percent in contrary to the results of this study.7 In a study in Pakistan, the mean HbA1c level was 6.34 percent in contrary to the results of this study.8 In a study form Indiana, Perry et al have observed that about 24% high risk diabetics had Fasting plasma glucose level of 100 – 109 mg/dl and 50% had FBS levels between 110 – 125 mg/dl.9 The mean (± SD) of HbA1c level was high in more than 60 years of age group and lesser in subjects aged between 21 – 30 years. There was a significant difference between the mean FBS levels in different age group patients but not significant with PPBS levels. In study in Pakistan, there was no correlation between the age of the patients and HbA1c levels.8 The mean (± SD) of FBS among males was 157.4 (± 48.98) mg/dl and among females was 151.45 (± 35.9) mg/dl. There was no significant difference between the mean FBS levels of males and females in this study. The mean (± SD) PPBS levels of males was 224.72 (± 41.36) mg/dl and females was 223.02 (± 37.04) mg/dl. The mean (± SD) of HbA1c was 7.59 (± 1.0) percent in males and 7.53 (± 0.9) percent in females. There was no significant difference between the HbA1c levels of males and females. In a similar study in China, the mean FBS, PPBS, and HbA1c were 5 mmol, 5.9 mmol and 5.5 percent among males and 5 mmol, 6 mmol and 5.5% respectively among females in contrary to the results of this study.7
CONCLUSION HBA1c test is most commonly used to measure the chronic hyperglycemia. The availability is main constraint especially in resource poor settings due to its high cost. The HbA1c test provides unreliable information especially in conditions such as the conditions reducing the life span of RBCs or hemoglobinopathies.
REFERENCES
|
 Home
Home