Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 2 - February2018
Prevalence of subclinical hypothyroid in rural population
Gulam Saidunnisa Begum1, Amtul Rahaman2*, Chetan Kumar3, Ayesha Jabeen4
1Associate Professor, 2,3Assistant Professor, 4Tutor, Department of Biochemistry, Mahavir Institute of Medical sciences, Vikarabad, Telangana, INDIA. Email: gulambegum1967@gmail.com
Abstract Background: Subclinical Hypothyroidism is a common endocrinological problem worldwide. The present study is a cross sectional study to determine the prevalence of sub clinical hypothyroidism in adults in rural Telangana. Methods: A total of 91 asymptomatic individuals of both sexes attending OPD of a tertiary health care centre and their willing attendants of the age group of 15 to 60 years were included in the study. Thyroid profile was performed on all of them and results were analysed. Results: out of total of 91 participants 15 females were detected hypothyroidism (subclinical as well as one overt). Subclinical hypothyroidism was the commonest entity encountered, females affected more than males. Conclusions: Subclinical as well as overt hypothyroidisms are significantly common in this part of the Telangana. Screening thyroid profile and specific TSH should be done in patients presenting with undiagnosed fatigue and weight gain. Keywords: Subclinical hypothyroidism, rural Telangana, Thyroid profile.
INTRODUCTION The prevalence of hypothyroidism in the developed world is about 4-5%.1,2 The prevalence of subclinical hypothyroidism in the developed world is about 4-15%.1,3 Hypothyroidism is a common endocrinological problem worldwide. Iodine deficiency was considered to be the commonest cause of goitre and hypothyroidism in India. Ever since India adopted the universal salt iodization program in 1983, there has been a decline in goiter prevalence in several parts of the country, which were previously endemic.4-7 Subclinical hypothyroidism is the most common thyroid disorder in adults, being more common in females, elderly age and its incidence increases with greater iodine intake.8-11 Subclinical hypothyroidism is defined as high S.TSH concentration with normal serum Free Thyroxine (FT4) and Free Triiodothyronine (FT3) concentrations, associated with few or no signs and symptoms of hypothyroidism.12 Various studies have shown that ScHt is associated with hyperlipidemia,13,14 neuromuscular15 and neuropsychiatric symptoms16,17 myocardial dysfunction18, and decrease in quality of life with progression to overt hypothyroidism. Due to apparently asymptomatic nature of the illness, the “American Thyroid Association”(ATA) has recommended routine population screening of both sexes at age 35 years and then every 5 years thereafter for early detection and treatment of ScHt. MATERIALS AND METHODS A total of 91 asymptomatic individuals of both sexes attending OPD of a tertiary health care centre of the age group of 15 to 60 years were included in the study. All of the participants were randomly selected. Inclusion criteria: 1. Adults in the age group of 15 to 50 years. 2. Willing to participate in the study. Exclusion criteria: 1. Age less than 15 or more than 60 years. 2. Family history of thyroid disorder. 3. Patient taking steroids, lithium or other drugs which can interfere with thyroid function tests. Data collection procedure: The following parameters are measured for all the study subjects lipid profile. Laboratory investigations: Blood samples were collected from the antecubital vein, in the early morning, after a minimum of 12 hours of fasting period, in a supine position. Assays for thyroid hormone (T3, T4 and TSH) were performed by the Electrochemiluminescence (ECL) technology using Immunoassay Analyzer Roche Cobas e411. Normal Ranges: T3: 69-215 µg/dL, T4 : 5.2-12.7 µg/dL, TSH: 0.35-5.5 µg/dL Hypothyroid: Serum thyroxine (T4) <5 ng/ml and thyroid stimulation hormone (TSH) >5.50μU/mL, Hyperthyroid: Serum T4>14 ng/ml and TSH<0.35 μIU/mL, Subclinicalhypothyroidism: Normal serum T4 and TSH>5.50 μIU/mL. Subclinical hyperthyroidism: Normal serum T4 and TSH<0.35 μIU/ml, STATISTICAL ANALYSIS The data collected was analyzed statistically with the help of SPSS software (version 20.0) Continuous variables are expressed as percentile.
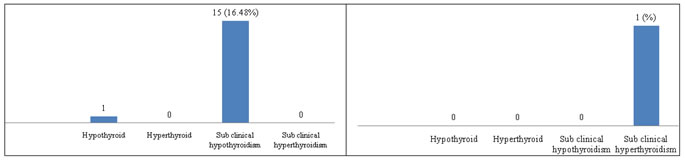
OBSERVATIONS AND RESULTS A total of 91 asymptomatic individuals of both sexes attending OPD of a tertiary health care centre of the age group of 15 to 60 years were included in the study. All of the participants were randomly selected. Subclinical hypothyroidism:Subclinical hypothyroidism was the commonest entity encountered in 15 (16.48%) of participants (Table 1). Subclinical hypothyroidism was found to be more common in females (Table 1, Graph:1). Overt hypothyroidism: Overt hypothyroidism was detected in 1 females individuals, (1%). (Table 1).
Table 1: Prevalence of subclinical hypothyroidism in study group
A total of 91 individuals of both sexes of the age group of 15-60 years were selected, from the OPD patients coming to hospital for illness unrelated to thyroid disease after following the inclusion and exclusion criteria. Out of these 85 were females and 6 were males. The mean age is 31.7 years. Subclinical hyperthyroidism:Subclinical hyperthyroidism was detected in 1 male individuals, (1%). (Table 1, Graph:2). Hyperthyroidism:Out of the 91 participants, none were detected to be havinghyperthyroidism.
Graph 1: Prevalence of Sub Clinical Hypothyroidism in Females Graph 2: Prevalence of Subclinicl Hypothyroidism in Males
DISCUSSION In the present study, we assessed the prevalence of thyroid disorders, particularly subclinical hypothyroidism, in rural population residing in Vikarabad Telangana state. subclinical Hypothyroidism was found to be a common form of thyroid dysfunction affecting 16.48% of the study population. Prevalence of subclinical hypothyroidism has been found to be more common in Females than males. This suggests that a significant proportion of patient population may go undetected and untreated even as it continues to impair the daily quality of life, work performance and economic productivity of an individual. The present study results are similar to the following studies: The majority of this study was could have sub-clinical hypothyroidism.19 The prevalence of hypothyroidism (clinical + subclinical) was 13.3% and 11.5% in the study from Kerala and Pondicherry, respectively.20,21 In the most recent nationwide study in India, the prevalence of overt undiagnosed hypothyroidism was 3.5% and the prevalence of subclinical hypothyroidism was 8.5%.22 In a study from Delhi in 2012 by Marwaha et al., subclinical hypothyroidism was present in 19.3% of subjects and 4.2% had overt hypothyroidism.23
CONCLUSIONS Our study gives an insight of prevalence of this entity in rural part of Telangana. Subclinical hypothyroidism is more common especially in females, usually presenting as vague manifestations. Common presenting complaint being fatigue, body aches, weight gain, constipation, menstrual irregularities, and sometimes infertility. So, any subject presenting with undiagnosed fatigue, weight gain and menstrual irregularities should be subjected to TSH screening.
ACKNOWLEDGMENT The authors would like express our gratitude to management for their continuous support, encouragement and motivation for conducting this study. Our sincere thanks to all the patients, and colleagues of MIMS for their Co-operation and support throughout the study.
REFERENCES
|
 Home
Home