Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 3 - March 2018
Electrolyte abnormalities in chronic heart failure patients on treatment with two different drug regimens
A Khadeja Bi1, S Suganya2*, Jnankumar Chaudhuri3
1Assistant Professor, 2Tutor, 3Professor, Department of Biochemistry, Karpaga Vinayaga Institute of Medical Sciences and Research centre, Chinnakolambakkam taluk, Kanchipuram Dst, Pin code 603 308, Tamil Nadu, INDIA. Email: sugansasi7@gmail.com, akhadbi@gmail.com, jc1973@rediffmail.com
Abstract Background: Heart failure is a complex clinical syndrome, impairing the ability of the cardiac ventricles to fill with or eject blood. Drug therapy for Chronic Heart Failure (CHF) is aimed at providing symptomatic relief and has to be continued indefinitely. Currently Angiotensin Converting Enzyme Inhibitor (ACEI), beta blocker and diuretic form the basis of treatment for CHF. These drugs can cause a wide array of electrolyte disturbances which frequently result in potentially dangerous complications. Early identification of these electrolyte disturbances and knowledge of the pathophysiological mechanisms underlying them will help in the effective management of these patients, when complex combinations of drugs are used. Objectives: 1.To estimate the serum sodium and potassium levels in ‘stable’ Chronic Heart Failure (CHF) patients on treatment. 2. To study the impact of Angiotensin Converting Enzyme inhibitors (ACEI), beta blockers and spironolactone with or without furosemide on serum sodium and potassium levels in stable CHF patients receiving the above drugs. Materials and Methods: A cross-sectional study was conducted on 120 stable chronic heart failure patients. In this, 60 patients were under Angiotensin Converting Enzyme inhibitors(ACEI), beta blockers, spironolactone and furosemide, while the other 60 patients were under Angiotensin Converting Enzyme inhibitors(ACEI), beta blockers and spironolactone regimen. Serum creatinine, sodium and potassium levels were analyzed in both the group. Conclusion: Majority of the drugs used in the treatment of CHF cause electrolyte disturbances. Hyponatremia in patients receiving all the four drugs and hyperkalemia in patients receiving only three drugs, was observed in our study. Key Words: Heart failure, electrolytes, Sodium, Potassium.
INTRODUCTION Chronic Heart Failure (CHF) is a condition, where the heart fails to pump adequate blood to the peripheral tissues, due to a structural or functional abnormality of the heart muscle. It is a disabling condition associated with high morbidity and mortality rates globally1. Drug therapy for Chronic Heart Failure (CHF) provides symptomatic improvement but has to be continued indefinitely, thereby increasing the life-long cost on treatment. Electrolyte disturbances are occurring very frequently in patients with heart failure. The major contributing factors for electrolyte disturbances in CHF are chronic activation of Renin-Angiotensin Aldosterone System (RAAS), sympathoadrenergic activation, renal dysfunction and adverse effect of the drug therapy2. Currently Angiotensin Converting Enzyme Inhibitor (ACEI), beta blocker and diuretics form the basis of treatment for CHF3. These drugs can cause a wide array of electrolyte disturbances like hyponatremia, hypo or hyperkalemia, which occur frequently resulting in potentially dangerous complications like arrythymias and sudden cardiac death in these patients4. Hence, this study was conducted to evaluate the impact of two different drug regimens (consisting of an Enalapril ( ACEI), Carvedilol ( beta blocker) and spironolactone (potassium sparing diuretic) with or without furosemide (a loop diuretic)) on serum sodium and potassium levels in stable CHF patients who were on regular treatment with these drugs. The early identification of these electrolyte disturbances and the knowledge of the pathophysiological mechanisms underlying the disturbance will help in the management of these patients.
MATERIAL AND METHODS A cross sectional study was conducted in a tertiary care teaching hospital in Tamil Nadu with stable CHF patients with Left ventricular ejection fraction <45% by echocardiography. Study design: Cross sectional study Study area: Rajiv Gandhi Government General Hospital, Tamil Nadu Study duration: October 2012 to November 2013. Data collection: 120 stable CHF patients who were on regular treatment for ≥3months were included in this study and were further subdivided into two groups based on their treatment regimen. Group I (n=60) received Enalapril 5mg, Carvedilol 20mg, Spironolactone 25mg and frurosemide 40mg while group II (n=60) were under Enalapril 5mg, Carvedilol 20mg and Spironolactone 25mg tablets on a daily basis. Inclusion Criteria: Stable CHF patients with Left ventricular ejection fraction <45% by echocardiography. Exclusion Criteria: Newly diagnosed heart failure patients of < 6months duration, acute or de-compensated heart failure patients, renal failure (eGFR <90mL/min) and patients on insulin therapy were excluded from the study. 2ml of blood was collected from the anti-cubital vein of the patients. Serum creatinine was estimated by kinetic Jaffe’s method (using an IDMS calibrator). eGFR calculated by MDRD formula. Serum sodium and potassium levels were measured using Ion selective electrode method. Statistical Analysis: The statistical analysis was calculated by using SPSS software 17.0v at 5% level of significance.
RESULTS
Table 1: Comparison of characteristics of Group I and Group II
Table 2: Mean, standard deviation and range of sodium and potassium in the two groups
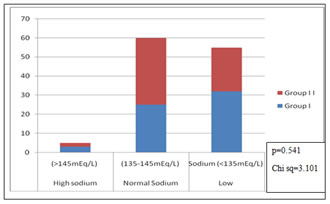
p=0.541 Chi sq=3.101
Chi sq=3.101
Figure 2: Distribution of study population with respect to their potassium levels
DISCUSSION CHF patients develop multiple electrolyte abnormalities as a result of several pathophysiological mechanisms. Diuretics (furosemide, spironolactone) are one of the most common causes of drugs induced hyponatremia5. Neurohormonal blockade using ACE inhibitors, beta-blockers and aldosterone antagonists may cause hyperkalemia6. In our study, group I andgroup II patients were analyzed for age, gender, diabetes mellitus,hypertension, left ventricular ejection fraction, serum creatinine and estimated GFR using SPSS software 17.0v and were found to be similar. Distribution of serum sodium and potassium levels in group I and group II patients were compared. Results showed that 53% and 38% had low serum sodium, 42% and 58% had normal sodium levels in group I and group II. 35% and 53% had high potassium levels in group I and group II while 38% had normal potassium levels in both the groups. Marcelo Villaca Lima et al observed in decompensated heart failure patients a two-fold increase in the incidence of hyperkalemia in patients using spironolactone, which was not statistically significant. A higher serum urea level in these patients correlated with hyperkalemia7. Cruz et al observed that the incidence of hyperkalemia (serum potassium >5.5mEq/L) in decompensated heart failure patients using ACEI and spironolactone was 32%. Functional class of heart failure, elevated basal serum creatinine and the presence of diabetes mellitus were identified as predictors of risk for the development of hyperkalemia in their study8. Low potassium levels causes diastolic dysfunction9, while high potassium is protective against hypertensive endothelial dysfunction10. A study conducted in the National Hospital Organization Osaka Medical Centre says that the occurrence of hyperkalemia is dose dependent in patients using spironolactone, but when it is administered along with enalapril, losartan or candesartan, the occurrence of hyperkalemia greater than 5.5 mEq/L increases even when low dose 25mg of spironolactone is used11. Scientific evidence supports that, the serum potassium level should be maintained above 4.5 mEq/L in heart failure patients to minimize the risk of sudden cardiac death12. Milionis HJ et al observed in their study, an incidence of 33.7% of hyponatremia in patients with congestive heart failure13. The OPTIME-CHF study concluded that serum sodium levels predicted mortality in outpatients with chronic heart failure14,15. In a study of 355 subjects admitted for HF, a serum sodium concentration 130 mEq/L (hyponatremia) was associated with a higher in-hospital death rate16. A meta-analysis from 22 studies predicted that the risk of death by 3 years increased linearly when serum sodium levels were less than 140 mEq/L17. Deubner et al observed in their study that, serum sodium levels of 135-139 mmol/L had an increased risk of mortality, whereas sodium levels of 140-145 mmol/L were associated with best prognosis in heart failure patients18. Several clinical studies have shown that hyponatremia is often encountered in patients with heart failure and is associated with increased rate of re-hospitalization, length of stay, hospital resource use and complications19,20. This in line with earlier studies predicting that electrolyte disturbances in sodium and potassium are more frequent in chronic heart failure patients on treatment with complex combination drug regimens.
CONCLUSION This study concludes that low serum sodium levels are more frequent in patients receiving enalapril, carvedilol, spironolactone and furosemide while high potassium levels are more frequent in patients receiving enalapril, carvedilol and spironolactone. As many of the electrolyte disturbances are drug-induced, during treatment with complex combination of drugs, one must anticipate and monitor them at frequent intervals in-order to prevent and to correct these electrolyte imbalances.
LIMITATIONS
REFERENCES
|
 Home
Home