Official Journals By StatPerson Publication
|
Table of Content - Volume 7 Issue 1 - July 2018
Serum lipid profile and Psoriasis – A case control study
Arati Ganiger1*, K Mallikarjuna Swamy2
1Department of Biochemistry, 2Department of ENT, KIMS, Koppal-583231, Karnataka, INDIA. Email: coolarati123@gmail.com
Abstract Background: Psoriasis is a chronic inflammatory skin disease characterized by excessive cellular replication. It is associated with an atherogenic lipid profile. The prevalence of cardiovascular disorders in these patients is remarkably higher compared to normal individuals, which seems to be associated with the hyperlipidemia. This study was designed to study the serum lipid profile levels in psoriatic patients to see its association with the severity of disease. Objectives: To evaluate serum lipid profile in serum of patients with psoriasis. Materials and Methods: It is a case control study. The study was conducted on 60 clinically diagnosed patients of psoriasis attending the outpatient department (OPD) of dermatology. Sixty (60) age and sex matched healthy subjects were taken as controls. Venous blood sample of 5 ml was collected, serum was separated and serum lipid profile was measured – total cholesterol (TC), triglycerides (TGL), high density lipoprotein (HDL). Results: Serum TC, TGL, low density lipoprotein(LDL) and Very low density lipoprotein (VLDL) levels were significantly increased in cases of psoriasis as compared to controls (p<0.001). Serum HDL levels were significantly reduced in cases of psoriasis as compared to healthy controls. Conclusion: Our study showed a significantly elevated levels of serum lipids in cases, which may aggravate the risk of atherosclerosis and other cardiovascular disorders. So screening of diagnosed cases for lipid profile is recommended to reduce the further compications. Key Words: Psoriasis, TC, HDL, LDL, Atherosclerosis, lipid profile.
INTRODUCTION Psoriasis is a chronic inflammatory skin disease characterized by erythematous scaly plaques over extensor aspects of the body and scalp1.It is an autoimmune disorder with unknown etiology. It affects 2 - 3% of world population2. The pathophysiology of psoriasis includes an increase in antigen presentation by dendritic cells, their presentation to T-cell with resultant T-cell activation and secretion of type 1 (TH1) cytokines by these cells3,4. Increased antigen presentation by dendritic cells and their presentation to T-lymphocytes lead to the following changes: T-cell activation and secretion of type 1 (TH1) cytokines like interferon, interleukin-2 and tumor necrosis factor alpha (TNF-a). These cytokines induce inflammatory changes in the epidermis, yielding thick scaly plaques. Psoriasis is considered as a systemic inflammatory disease causing various complications and co-morbidities which have significant impact on patients’ health and quality of life5. Early cardiovascular deaths have been reported in psoriatic patients as compared to general population. This may be related to the fact that the risk factors of cardiovascular disease and metabolic syndrome appear to be more common in patients with psoriasis compared with the general population which leads to accelerated atherosclerosis and coronary heart disease. These risk factors include obesity, smoking, diabetes mellitus, hypertension and dyslipidemia5,6. Recently, the role of Tlymphocytes in pathogenesis of psoriasis and atherosclerosis has been clarified7. Psoriasis has been associated with abnormal plasma lipid metabolism and diabetes, probability related to alterations in insulin secretion and sensitivity8. Furthermore, there is increased oxidative stress which is accompanied by a high frequency of cardiovascular disease9. The high rate of cardiovascular events is related to the severity of the disease which occurs more frequently in patients with large areas of the body affected by psoriasis lesions. Although hyperlipidemia is one of the cardiovascular risk factors, but the results are inconsistent10. Several studies have shown that psoriatic patients have proatherogenic lipid profile with raised levels of serum TGL, TC including LDL and VLDL cholesterol and lower levels of cardioprotective HDL cholesterol11,12. The aim of present study was to measure the serum lipid profile of psoriatic patients and to compare the mean with the lipid profile of healthy controls after exclusion of other risk factors of hyperlipidaemia like increased smoking, hypertension, diabetes, alcoholics, hepatic or renal diseases and drugs causing hyperlipidaemia.
MATERIALS AND METHODS It is a case control study. The study was conducted on 60 clinically diagnosed patients of psoriasis attending the outpatient department (OPD) of dermatology at SNMC Bagalkot. Sixty (60) age and sex matched healthy subjects were taken as controls. The study was conducted over a period of 18 months from August 2012 to February 2014. Informed consent was taken from all the subjects. Ethical clearance was obtained from institution’s ethical clearance committee. The clinical severity of the disease was determined according to the PASI score. By estimating the extent of the body surface involvement, scaling in percentage and scoring the erythema, thickening of the affected areas (scalp, trunk, the lower limb and upper limb), the severity of the disease was determined. Patients were classified according to rule of nine in to 3 types:
Mild to moderate cases of psoriasis on topical therapy only were included in study. Inclusion Criteria: Recently diagnosed cases of psoriasis were included in the study Exclusion Criteria
Biochemical Analysis: A fasting blood sample of 5 ml venous blood was collected under aseptic precautions in a plain vial. It was allowed to clot and serum was separated by centrifugation. Lipid profile was analysed using automated analyser by following methods:
LDL = TC – (HDL + TG/5) Statistical Methodology: Data was expressed in terms of mean±SD. Chi- square test was applied to estimate the difference between the two groups of population. Unpaired ‘t’-test was used to study the changes in serum lipid levels between the study groups. Pearson correlation was performed to establish the relationship between study variables. p value <0.05 was considered statistically significant.
RESULTS Table 1: Age distribution of the subjects
Table 2: Gender distribution of the subjects
Table 3: Comparison of serum lipid levels between controls and Psoriasis patients
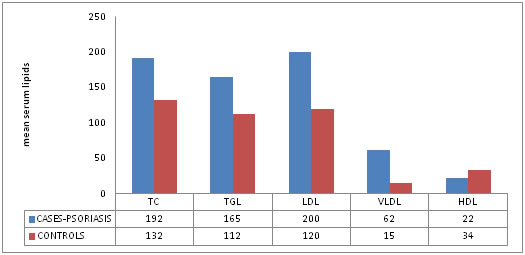
This was a comparative case control study conducted on 60 diagnosed cases of psoriasis patients (n=60) and 60 age and sex matched healthy controls (n=60). Serum lipid levels were estimated and analyzed in cases and controls. The results were expressed as mean±standard deviation. The age distribution of cases and controls is depicted in Table 1. The mean age (in years) of cases is 40.3±10.7 years and that of controls is 41.2 ±10.3 years and is not significant (p>0.05).Table 2 shows the gender distribution. Out of 60 cases of psoriasis, 30 (50%) were males and 30 (50%) were females. Out of 60 controls, 30 (50 %) were males and 30 (50%) were females and it was not statistically significant (p=0.38). Figure 1: Comparison of serum lipids between cases (psoriasis) and controls
The mean serum Cholesterol, serum HDL, serum LDL, serum VLDL and serum TGL levels in psoriasis cases and control group are shown in Table 3. A statistically significant increased values of TGL, LDL, VLDL, total cholesterol (p<0.001) was noted in cases as compared to controls. The serum HDL levels were found to be decreased in cases as compared to controls (Figure 1). TC-total cholesterol. TGL- triglyceride, LDL-low density lipoprotein, VLDL-very low density lipoprotein, HDL- high density lipoprotein.
DISCUSSION A total of 120 subjects were included in the study. Among them, 60 were cases of psoriasis and 60 were controls. Our finding suggests that levels of serum total cholesterol, triglyceride, high density lipoprotein, low density lipoprotein were altered in psoriasis patients than in age- matched control subjects. Serum TC, TGL, LDL, VLDL levels were significantly increased in cases where as serum HDL levels were significantly reduced (p<0.001). The degree of elevation of serum total cholesterol is associated with the progression of psoriasis. Several studies have demonstrated that serum total cholesterol levels are higher in psoriasis13,14. These findings supports our results. Psoriasis is now considered as immunometabolic syndrome15. The abnormal fat metabolism was considered to be an important factor in the etiopathogenesis of psoriasis16.The pathophysiology of psoriasis includes activation of Th1 and Th17 helper T-cells with production of pro-inflammmatory cytokines like TNF-alpha, INF-gamma, IL-1, IL-6, IL-8 and IL-17. These cytokines maintain a pro-inflammatory environment in psoriatic skin. These cytokines also cause obesity, insulin resistance, dyslipidemia, endothelial dysfunction, increased oxidative stress and therefore, are pro-atherogenic17. Therapy with retinoids and cyclosporine may also cause hyperlipidaemia in psoriatic patients18.Structural andfunctional changes in gastrointestinal tract of psoriatic patients may lead to increased absorption of dietary lipids leading to hyperlipidaemia. Hyperlipidaemia along with other risk factors like diabetes mellitus, increased BMI, and smoking cause premature atherosclerosis which leads to increased cardiovascular morbidity and stroke in these patients19.These lipid abnormalities seen in psoriasis might facilitate and maintain the inflammatory reaction in the skin. The level of antibodies against oxidized LDL is reported to correlate with disease severity20. Therapy with statins may be beneficial to patients with psoriasis, as these reduce LDL oxidation and may even have immunomodulatory activities that may improve the psoriatic skin and cause a shift from pro-inflammatory to antiinflammatory conditions in psoriasis. TNF- alpha inhibitor therapy is associated with beneficial effects on lipid profile. Therefore, psoriasis may be associated with hyperlipidaemia and hyperlipidaemia is associated with more severe psoriatic disease21. There is an emerging consensus as to the role of the chronic inflammatory state in diseases like systemic lupus erythematous and rheumatoid arthritis and the accompanying proinflammatory milieu in promoting development and progression of dyslipidemia and atherosclerosis. It is likely that psoriasis, a chronic immune mediated inflammatory skin disease, may predispose individuals to dyslipidemia22. This association is demonstrably stronger for severe psoriasis and psoriatic arthritis. Psoriasis has also been shown to be an independent risk factor for cardiovascular mortality23,24. In addition, there appears to be a significant association between psoriasis and traditional risk factors for atherosclerosis and heart disease in the general population such as diabetes mellitus type II, coronary artery disease, peripheral vascular disease and hypertensive heart disease25,26. It also demonstrates that the patients should implement a proper strategy for reducing the risk of cardiovascular diseases, particularly in patients with higher level of involvement and with periodic determination of serum lipids. Early screening of hyperlipidemia and treatment of these patients is highly recommended.
CONCLUSION Our study shows that lipid levels were increased with the progression of disease. This rise in lipid levels and decreased High density lipoprotein fraction is an alarming sign that psoriasis is progressing towards Cardiovascular risk. Therefore, controlling the lipid fractions and early management can save psoriasis patients from cardiovascular risk
REFERENCES
|
 Home
Home