Official Journals By StatPerson Publication
|
Table of Content - Volume 7 Issue 1 - July 2018
Serum lipid profile in diabetic retinopaty – A case control study
Arati Ganiger1*, K Mallikarjuna Swamy2
1Department of Biochemistry, 2Department of ENT, KIMS, Koppal-583231, Karnataka, INDIA. Email: coolarati123@gmail.com
Abstract Background: Uncontrolled hyperglycemia has been recognized to be in association with high incidence of microvascular complications like retinopathy and nephropathy in Type II diabetes mellitus. Diabetic retinopathy (DR) is a microvascular complication of diabetes, which is a cause of visual impairment and blindness. Its development and progression have been linked to dyslipidaemia. Objectives: To evaluate serum lipid profile among type 2 diabetes mellitus (T2 DM) patients with and without retinopathy .To determine the effect of dyslipidaemia on diabetic retinopathy (DR). Materials and Methods: It is a case control study. The study included 50 cases of clinically diagnosed type 2 DM with retinopathy and 50 cases of type 2 DM without retinopathy used as controls. Venous blood sample of 5 ml was collected, serum was separated and serum lipid profile was measured – total cholesterol (TC), triglycerides (TGL), high density lipoprotein(HDL) in both cases and controls. Statistical analysis was done using student 't' test. Pearson's correlation was performed to establish the relationship between study variables Results: There was markedly increased levels of serum concentration of TC and LDL in diabetic retinopathy cases as compared to controls and was statistically highly significant. (p<0.001) .There was mild increase in serum TG it was also significantly correlated (p<0.01). There was significant decrease in HDL levels in diabetic retinopathy cases as compared to controls. Conclusion: Our study shows dyslipidemia is highly prevalent in diabetic retinopathy and that increased lipid levels has a role in the causation and progression of diabetic retinopathy. Key Words: Diabetes Mellitus, Diabetic retinopathy, trigkycerides, TC, LDL, Lipid profile
INTRODUCTION Type II Diabetes Mellitus (DM) is a metabolic disorder primarily characterized by hyperglycemia. It is caused by insulin resistance and/or relative insulin deficiency1. Chronic hyperglycemia is a major initiator of microvascular complications, including nephropathy, retinopathy and neuropathy2. Diabetic retinopathy is one of the dangerous complication of DM and also is a leading cause of acquired blindness in adults. Several risk factors are related to the development and progression of retinopathy such as the duration of DM, poor glycemic control, dyslipidemia, hypertension and hypomagnesemia3,4. DR can be classified into mild, moderate and severe non-proliferative diabetic retinopathy (NPDR), proliferative diabetic retinopathy (PDR) and advanced diabetic eye disease (ADED)5. NDPR is characterised by formation of microaneurysms and retinal vascular permeability and leakage, and PDR is characterised by neovascular proliferation and vitreous haemorrhage6. Dyslipidaemia has been linked to the pathogenesis of DR, but results from past research showed discrepancy on the association of serum lipids with DR severity. The mechanism by which high serum lipids may cause the progression of diabetic retinopathy is not clearly understood. It has been postulated that elevation of blood viscosity and alterations in the fibrinolytic system occurs in hyperlipidemia causing hard exudate formation. There may also be incorporation of triglycerides into the cell membrane leading to changes in membrane fluidity7 and leakage of plasma constituents into the retina. This results in haemorrhage and oedema in the retina. Thus, the aim of this study was to determine the association between dyslipidaemia and DR severity in type 2 diabetic patients with and without retinopathy.
MATERIALS AND METHODS Study participants: This was a case control study. The study was carried out on 50 cases of clinically diagnosed type 2 diabetes mellitus with retinopathy and 50 cases of type 2 diabetes mellitus without retinopathy attending the Opthalmology OPD at SNMC and HSK hospital, Navanagar, Bagalkot . The study was conducted over a period of one year from march 2013 to March 2014. Ethical clearance was obtained from the institute’s ethical clearance committee. Informed consent was taken from the cases and controls after explaining the procedure. Diabetes Mellitus was diagnosed as per the WHO diagnostic criteria8. Retinopathy was diagnosed by fundus examination under mydraisis of both eyes using opthalmoscope and 90 D lens9. Inclusion Criteria
Exclusion Criteria
Based on the analysis of medical history, clinical examination and investigation results, the patients were grouped into type 2 DM with and without retinopathy. Biochemical analysis: A fasting blood sample of 5 ml venous blood was collected under aseptic precautions in a plain vial. It was allowed to clot and serum was separated by centrifugation. Lipid profile was analysed using automated analyser by following methods:
LDL = TC – (HDL + TG/5) Statistical Methodology: Data was expressed in terms of mean±SD. Chi- square test was applied to estimate the difference between the two groups of population. Unpaired ‘t’-test was used to study the changes in serum lipid levels between the study groups. Pearson correlation was performed to establish the relationship between study variables. p value <0.05 was considered statistically significant.
RESULTS
Table 1: Age distribution of the subjects
Table 2: Gender distribution of the subjects
Table 3: Comparison of serum lipid levels between cases of DM with retinopathy and controls
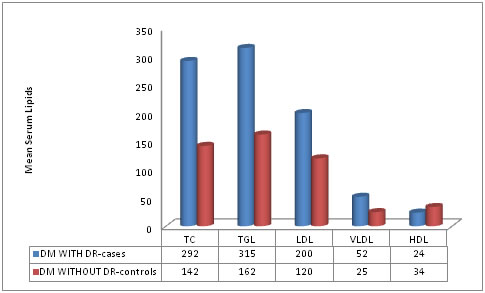
Figure 1: Mean serum lipids in DM with and without retinopathy
TC-Total Cholesterol, TGL-Triglycerides, LDL-low density lipoprotein, HDL- high density lipoprotein, VLDL-very low density lipoprotein. This was a comparative case control study conducted on 50 cases of type 2 DM (n=50) with retinopathy and 50 cases of type 2 DM without retinopathy (n=50). Serum lipid levels were estimated and analyzed in cases and controls. The results were expressed as mean ± standard deviation. The age distribution of cases and controls is depicted in Table 1. The mean age (in years) of cases is 50.3±7.8 years and that of controls is 51.11 ±8.8 years and is not significant (p>0.05). Table 2 shows the gender distribution. Out of 50 cases of type 2 DM with DR, 26 (52%) were males and 24 (48%) were females. Out of 50 controls of type 2 DM without retinopathy, 24 (48 %) were males and 26 (52%) were females and it was not statistically significant (p=0.38). The mean serum total cholesterol, serum HDL, serum LDL, serum VLDL and serum TGL levels in cases of type 2 DM with DR and control group type 2 DM without retinopathy are shown in Table 3. A statistically significant increased values of TGL, LDL, VLDL, total cholesterol (p<0.001) was noted in cases as compared to controls. The serum HDL levels were found to be decreased in cases as compared to controls (Figure 1).
DISCUSSION Diabetes mellitus is an endocrinological disease having high metabolic and oxidative stress. Diabetic retinopathy is a important microvascular complication of uncontrolled diabetes mellitus and is one of the leading causes of acquired blindness. Findings show that oxidative stress has the greatest role in development of the complications. Many risk factors have been related to the development and progression of retinopathy in diabetic patients. In the present study, it was found that TC, LDL and TGL levels were significantly higher (p<0.0001) in diabetic subjects with retinopathy as compared to the control group. This is due to the increased flow of glucose and fatty acids to liver due to lack of insulin. Decreased clearance of LDL and TG is due to over production of apolipoprotein B and low lipoprotein lipase activity. On comparing cases and controls, it was found that TGL levels were significantly raised (p<0.05) in patients of DR. The raised TGL levels leads to increased blood viscosity and altered fibrinolytic activity which leads to formation of hard exudates. Also, TGL incorporates into the cell membrane, altering its fluidity and permeability which leads to hemorrhage and oedema. This also leads to endothelial cell dysfunction and local inflammatory response releasing cytokines and growth factors which are responsible for neovascularisation in retina (Joussen et al, 2001).
CONCLUSION Our study shows that alteration in lipid profile has a role as a risk factor in causation and pathogenesis of severity of Diabetic Retinopathy.
REFERENCES
|
 Home
Home