Official Journals By StatPerson Publication
|
Table of Content - Volume 8 Issue 2 - November 2018
Association of dyslipidemia in lichen planus patients at KIMS, Hubli – A case control study
Manasa D R1, Chandru M C2*, Ravi M Rathod3, Vidya Kuntoji4
{1,4PG Student, 2Professor and HOD, Department of Biochemistry}, {3Professor and HOD, Department of Dermatology, Venereology and Leprosy}, Karnataka Institute of Medical Sciences, Hubali, Karanataka, INDIA.
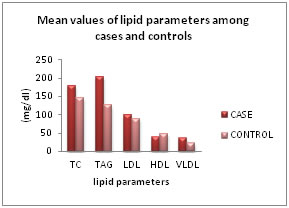
Abstract Background and Objective: Lichen planus (LP) is an idiopathic chronic inflammatory skin disorder where it etiopathogenesis is not fully understood. Persistent inflammation causes lipid disturbances, which precipitate the increase of cardiovascular risk. However, there are limited data about the lipid levels in LP patients and hence this study was undertaken to estimate the lipid levels in LP patients. Methods: A case control study was conducted, including 50 LP patients and 50 age and sex matched controls. Serum levels of TC (CHOD-PAP method), TAG (GPO-PAP method), and HDL-C (CHOD-PAP method) were estimated. LDL-C was calculated by Friedewala’s formula. Results: Patients with LP presented higher significant triglyceride values (182.93 vs. 113 mg⁄ dl), total cholesterol values (178.69 vs. 145.56 mg⁄ dl), LDL-C values (100.5 vs. 81.5 mg⁄ dl), and lower HDL-C values (40.36 vs. 47.6 mg⁄ dl) vs. controls. Interpretation and Conclusion: The results obtained in this study indicate the association of dyslipidemia in LP patients. Thus, dyslipidemia may play a role in its etiopathogenesis, hence, the lipid levels screening in LP patients will be useful to detect individuals at risk and start preventive treatment against the development of cardiovascular disease. Key Words: Cardiovascular diseases; Dyslipidemias; Inflammation; Lichen planus;
INTRODUCTION Atherosclerosis is one of the major contributing risk factors for cardiovascular diseases. Moreover, current predictions estimate that by the year 2020 cardiovascular diseases, notably atherosclerosis1 will become the leading global cause of the total disease burden. Many subclinical diseases and inflammatory pathologies go undiagnosed for the risk of cardiovascular diseases where its etiopathogenesis still remains perplexing. Chronic inflammatory skin disorders such as psoriasis are associated with increased cardiovascular comorbidity which is a well-known fact. Leaving aside a few, majority of studies conducted worldwide have clearly pointed towards a positive association between psoriasis and dyslipidemia. Recently this association has been extended to various other dermatological conditions such as androgenic alopecia, skin tags, lichen planus, and even skin cancers. Lichen planus (LP) is a chronic inflammatory skin disorder and affects everyone irrespective of age, sex and geographical location. The etiology and pathogenesis of LP are not fully understood and still remains unknown. It is thought to be a T-cell-mediated inflammatory disorder and has been associated with multiple disease processes and agents, including viral infections, autoimmune diseases, medications, vaccinations and dental restorative materials2,3,4. Recently, a case-control study showed that LP was associated with dyslipidemia5. Persistent inflammation causes the disturbances in lipid metabolism such as decrease in High Density Lipoproteins – Cholesterol (HDL-C), increase in Very Low Density Lipoprotein-Cholesterol (VLDL-C) and hypertriglyceridemia. Prolonged dyslipidemia, due to chronic inflammatory condition enhances the formation of atherosclerotic plaques and thereby augments the risk of cardiovascular disease in such patients. Various cytokines are involved in the pathogenesis of LP and induction of the IFN-a-inducible CXCR3 ligands CXCL9, CXCL10 and CXCL11 has been reported. These inflammatory processes could potentially explain the link between LP and dyslipidemia6,7. All these factors contribute to the development of cardiovascular risks in LP. Knowledge of the distribution of cardiovascular risk factors in LP patients would allow us to apply the preventive measures in the patients. Hence, the present study was undertaken to assess the association of dyslipidemia in lichen planus patients and to evaluate the possible mechanisms that leads to cardiovascular risks in lichen planus patients.
MATERIAL AND METHODDS Source of data: A case-control prospective study was carried out for a period of one year from July 2015 to June 2016 at Karnataka Institute of Medical Sciences, Hubli, Karnataka. The study group consists of 50 diagnosed lichen planus patients from the Department of Dermatology OPD and the 50 healthy controls. Both the cases and controls are interviewed to obtain relevant data after taking informed consent. The institutional The cases were selected based on the inclusion and exclusion criteria. Convenient sampling method was used to determine the sample size as the exact prevalence of the disease is unknown. Inclusion Criteria: Cases
Control
Exclusion criteria: 1) Lichenoid drug eruption 2) Receiving treatment for LP such as systemic corticosteroids, retinoic acid, methotrexate. Diagnosis was made based on clinical symptoms and confirmed by histopathological features. Weight and height was measured and body mass index (BMI) was calculated by the formula: weight in kg/ height in m2. Method of collection of data: After relevant history taking and informed consent, about 5 ml of fasting venous blood was drawn under aseptic precautions in vacutainer with clot activator. The serum was separated by centrifugation and used for analysis of serum total cholesterol, triglycerides, HDL-C and LDL-C by fully automated biochemistry analyzer. Serum total cholesterol was measured by cholesterol oxidase-phenol aminoantipyrine (CHOD-PAP) method, serum triglyceride was measured by glycerol phosphate oxidase-phenol aminoantipyrine(GPO-PAP) method, serum HDL-C was measured by phosphotungstic acid and cholesterol oxidase phenol aminoantipyrine (CHOD-PAP) method by using reagent kits from ERBA diagnostics Mannheim GmbH, Germany. Whereas LDL-C and VLDL-C was calculated by Friedewald’s formula. LDL cholesterol (mg/dl) = Total cholesterol – (HDL + Triglycerides) 5VLDL cholesterol (mg/dl) = Triglycerides / 5 In addition, TC/HDL-C and LDL-C/HDL-C ratios were calculated. Data were also gathered on age, sex, habits like smoking, alcohol consumption and hypothyroidism, personal or family history of cardiovascular disease and whether the patients were on antihypertensive, cholesterol lowering drugs. The presence of dyslipidemia was defined if one of the following parameters were present: 1) Triglycerides >150mg/dl; 2) Total cholesterol > 200mg/dl; 3) LDL-C >130mg/dl; or 4) the patient received treatment for dyslipidemia. Statistical Analysis: Results were expressed as mean ± standard deviation (SD). Statistical analysis was done using IBM SPSS software version 20.0 Student‘t’ test was used to compare the means between the cases and the controls. Pearson’s correlation co-efficient was used to measure the relationship between different parameters. For all the tests, the probability value (p value) of less than 0.05 was considered statistically significant. RESULTS A total of 100 individuals were studied, 50 with LP and 50 healthy controls. Among 50 cases, 29 were males and 21 were females. Table No.1 shows mean age, height, weight and BMI among lichen planus patients and controls. Height, weight, and BMI values shows higher mean in cases than controls which is statistically highly significant at p<0.0001 Table 1: Mean values of age, height, weight and BMI among cases and controls
Values are expressed as mean ± SD
Table 2: Comparison between serum levels (Mean ± SD) of TC, TAG, LDL-C AND HDL-C in cases and controls
Table No.2 shows comparison of mean levels of lichen planus patients and controls. It is observed from table, that patients showed higher mean TC, TAG and LDL levels than the controls which was highly significant (p<0.0001) by application of student’s t test. Mean levels of HDL showed lower levels in patients than the controls which was statistically highly significant (p<.0001) by application of student’s t test.
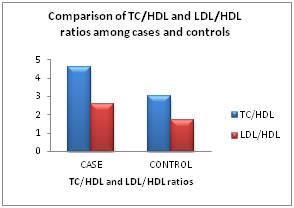
Table 3: Comparison of TC/HDL ratios and LDL/HDL ratios among cases and controls
Table No.3 shows the comparison of TC/HDL and LDL/HDL ratios among lichen planus patients and controls. It is observed from table that both TC/HDL and LDL/HDL ratios represents higher mean values among the cases than the controls which was highly significant (p<0.0001) by application of student’s t test.
Table 4: Dyslipidemia among cases
X2 = 1. 39, df =1, p < 0.05, Significant Table No.4 shows dyslipidemia among lichen planus patients. Among 50 cases, 62% of them had dyslipidemia. It was more among the males (58.1%) than compared to females (41.9%) by application of chi-square test. The observation was found to be statistically significant at p<0.05. X2: chi-square test; df: difference of freedom.
DISCUSSION Chronic inflammation plays a pivotal role in immunopathogenesis of many inflammatory pathologies such as diabetes, metabolic syndrome, cancer, ischemia etc. Whereas, lichen planus is an idiopathic chronic inflammatory skin disorder and its etiopathogenesis are clearly unknown. It is believed to be T-cell immune mediated, where it stimulates the many proinflammatory mediators like cytokines, interleukins etc. But, the persistent inflammation causes the alterations in the lipid metabolism which in turn precipitates the cardiovascular risk factors in patients. Also, the local production of inflammatory mediators can stimulate the production of reactive oxygen species (ROS) which damages the cell membrane by lipid peroxidation. Hence, the present study was undertaken to assess the association of lipid disturbances in LP patients. Table no.1, showed higher mean values of weight and BMI in lichen planus patients than the controls which was statistically highly significant p (<0.0001).Increased BMI is one of the contributing risk factor for cardiovascular disease. Present study showed higher mean values of about 29.4 which is in the range of overweight. Several studies have shown the association of increased BMI in cardiovascular diseases. A high body mass index is a risk factor for mortality from overall cardiovascular disease and for specific diseases, including coronary heart disease, ischaemic stroke and haemorrhagic stroke8. Our study showed higher mean values of TC (178.69± 35.8), TAG (182.93± 127.2) and LDL (100.51± 26.0) and lower mean value of HDL (40.36± 11.4) which was statistically highly significant in LP patients. Also present study showed among 50 cases, 62% of them had dyslipidemia. It was more among the males (58.1%) than compared to females (41.9%). The observation was found to be statistically significant (p<0.05). Study by S. Arias-Santiago et al5, showed higher significant TAG values (p= 0.0007), TC values (p = 0.001), LDL-C values (p< 0.0001) and lower HDL-C values in LP patients compared with other skin diseases. The prevalence of dyslipidemia in patients with LP was 61.3% and 32.5% for controls [P = 0.0005, OR = 3.28, 95% confidence interval (CI) = 1.71–6.28]. The prevalence of dyslipidemia according to gender showed higher in men with LP of 67.5% and 55% of women with LP. Similar case-control study by J. Dreiher et al9 included large number of participitants in Israel showed higher prevalence of dyslipidemia in LP even after controlling for confounders, including age, sex, smoking, hypothyroidism, diabetes, hypertension, socioeconomic status and obesity. Another study by Melita Vuksic Policet al10, conducted research in a case-control study, comprised of 72 patients with LP and 30 participants from control group, showed strong connection between the imbalanced concentrations of one or more serum lipids and the occurrence of LP. Some drugs used for dyslipidemia are associated with lichen planus-like eruption and many drugs used for the treatment of LP such as retinoid acid, methotrexate or systemic corticosteroids are also associated with dyslipidemia. Hence in the present study, we have excluded the lichenoid drug eruption and the one who is receiving the treatment for LP. But we have included the patients who stopped the therapy previously for more than 3 months. Since drugs used for the treatment of lichen planus causes dyslipidemia hence we considered the wash out periods for each drug. The washout period of retinoids, systemic cortico-steriods and methotrexate are 30 days11, 3months12 and 2-3 months13 respectively. Also our study showed higher mean values of ratios of both TC/HDL (4.6±1.17) and LDL/HDL (2.6±1.10) in lichen planus patients compared to the controls. Increased LDL-C/HDL-C ratio has been considered as a sensitive predictor of cardiovascular risk, and recently, total cholesterol/HDL-C ratio has been found an even better predictor metabolic index for cardiovascular risk in large study14.In the present study, patients with lichen planus presented higher values of both ratios. Sharrett et al15stated that higher values of triglycerides and low levels of HDL-C were associated with the transition from atheroma to atherothrombosis and therefore, control of these two cardiovascular risk factors is essential in patients with subclinical disease.
CONCLUSION The results obtained in our study support the association of dyslipidemia in LP patients after controlling the confounding factors. The study also highlights the importance of routine screening for dyslipidemia would be helpful to the individuals at risk for cardiovascular disease at earlier stage and thereby prevent the incidence of atherosclerosis in lichen planus patients.
REFERENCES
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home