Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 1 - January 2019
A comparative study of anatomical variations in nose and paranasal sinuses to establish the etiological basis of chronic rhinosinusitis
Singh S1*, Garg A K2, Veereddy N3
1Senior Resident, Surgical Oncology(Head & Neck) AIIMS, Rishikesh, Uttarakhand, INDIA. 2Professor and HOD, 3DNB Resident, Department of ENT, Jawaharlal Nehru Hospital and Research Centre, Bhilai, Chhatisgarh, INDIA. Email: rlssengar@gmail.com
Abstract Aim: This observational study aimed at finding the anatomical variations in nose and paranasal sinuses in the patients registered for localized or non-localized diseases in the ENT department of our tertiary care hospital and to search whether these variations were actively involved in the etiology of the diseases. Material and Methods: We analyzed 100 patients attending the ENT outdoor department, fulfilling the specific inclusion criteria from December, 2015 to December, 2016 for 1 year and comprised into 2 specific groups, one with chronic rhinosinusitis (CRS) and other group with no sinonasal diseases of same age group. Anatomical variations in nose and paranasal sinuses were noted on CT scan imaging. Result: The rates of anatomical variations in two groups were calculated separately and compared with each other. Septal deviation is the commonest anatomical variation of nose and paranasal sinuses followed by agger nasi cell, concha bullosa respectively. There were no significant statistical differences between the groups concerning the rates of all these mentioned variations. Conclusion: This study using computed tomography scan as the main tool underlined the fact that sinonasal area has very high rate of anatomical variations. Careful assessment of CT in patients is necessary, especially in those undergoing FESS (Functional Endoscopic Sinus Surgery). Key Word: Chronic rhinosinusitis, Functional Endoscopic Sinus Surgery, Ostiomeatal complex, Computer Tomography scan.
INTRODUCTION Nose and paranasal sinuses constitute an anatomical and functional unit. All the paranasal sinuses open into the lateral wall of the nasal cavity through their corresponding ostia. The middle meatus is the space lateral to the middle turbinate, and is often functionally referred to as the ostiomeatal OMC.23 The drainage of maxillary, frontal and anterior ethmoid sinuses occurs in ostiomeatal complex (OMC) thus the blockade in the same area leads to impaired emptying of sinuses thus causing chronic rhinosinusitis (CRS).1 Certain variations in nose and paranasal sinuses noticed once the radio imaging emerged and helped surgeons to be more cautious during the trans nasal surgeries. The various variations seen in the nose and paranasal sinuses described in the literature are as follows- Septal Deviations (SD): These variations in turn may compromise the OMC. Concha bullosa (CB): It is pneumatisation of the middle turbinate. CB is implicated in the pathogenesis of rhinosinusitis because of its tendency to narrow the middle meatus and the infundibulum. Superior Concha bullosa and Inferior concha bullosa: Pneumatisation of the superior and inferior turbinate as well is very rare.7 and both may contribute to sinusitis. Paradoxical middle turbinate: When the convexity is directed laterally, it is termed a paradoxical middle turbinate. Most authors agree that the paradoxical middle turbinate can be a contributing factor to sinusitis. Haller Cells (HC): They are an etiological factor for sinusitis since they vary in size and when large can narrow the ostium of the maxillary sinus or the ethmoid infundibulum. The presence of an infraorbital cell may increase the risk of injury to the orbit during FESS, an unrecognized cell masking the position of the orbital wall2. Agger nasi cells (ANC): Its degree of pneumatisation has significant effect on frontal sinus drainage and surgical access. Recognition of this relationship is crucial in management of chronic frontal sinusitis.5 Onodi cells (OC): Extensive pneumatisation can expose the circumference of optic nerve, which is surrounded by air spaces, mainly the inferior half.15 Uncinate Process (UNC): Pneumatisation of the uncinate process is known as uncinate bulla and is rarely the cause obstruction of the infundibulum.3,27 Bulla ethmoidalis (BE): A giant/prominent bulla may fill the entire middle meatus and force its way between the uncinate process and the middle turbinate. Supraorbital cells (SOC): can compromise posteriorly the frontal sinus drainage, in a similar way as the agger nasi anteriorly. During FESS, supraorbital cells can be mistaken for the frontal sinus by inexperienced surgeons. Maxillary sinus hypoplasia: uncommon condition that is misdiagnosed as chronic sinusitis.22 and it may impede mucociliary clearance and is liable to retention of mucus. Failure to recognize maxillary sinus hypoplasia intraoperatively can lead to injury to the medial orbital wall.4 Sphenoid sinus variations and Frontal sinus variations: should also be noticed not only for ENT surgeries but also while doing neurosurgical procedures. The role of CT is to display the regional anatomy and to identify the anatomic factors that may be the cause of recurrent chronic inflammatory disease.14Some anatomic variants are probably not responsible for development of disease per se, but knowledge of their presence is paramount. Coronal CT of the sinonasal complex has been shown to be the best imaging technique for simulating the endoscopic spatial orientation, thus improving the surgeon’s perception in an attempt to reduce complications of surgery.101Hence, in our study we will be evaluating presence of individual anatomical variations of nose and paranasal sinuses in our 2 separate groups using CT scan, and will evaluate the presence of anatomical variations as an associating factor in patients with chronic rhinosinusitis.
MATERIAL AND METHODS This observational study was approved by the institution ethical committee and informed consent has been taken from each patient and their relatives. A total of 100 patients were taken for the study from Dec, 2015- Dec, 2016 for 1 year and comprised of 2 groups of 50 patients each. In first group, we included clinically diagnosed cases of chronic rhinosinusitis (according to task forces criteria) fulfilling the inclusion criteria while second group includes patients with no sinonasal complaints but attending the ENT OPD owing to other illness. Detailed history and examination were evaluated and recorded. Inclusion criteria
Exclusion criteria
All the enrolled cases underwent Computed Tomography (CT) nose and paranasal sinus (PNS). Plain CT Scan (PNS) was done in coronal planes, with SYMBIA 6 slice CT scanner (Siemens Company). Patient’s position kept supine with extended neck and the plane perpendicular to the infraorbitomeatal line for coronal sections. CT scans performed using the bone algorithm, a 3-mm interval of the coronal view for the anterior groups of PNS (anterior walls of the frontal sinuses to the posterior wall of the sphenoid sinus) and 5-mm section of the coronal view for the posterior PNS groups. We defined minimal disease as more than 2-3 mm mucosal thickening with no obstruction of the sinus drainage passages. Each CT scan was reviewed by an otolaryngologist and a radiologist. Final Reporting of CT scan was done by a senior radiologist. In both the groups the existence of the variants were investigated and noted. Parameters evaluated The study parameters were age, sex, clinical diagnosis and radiographic findings on CT scan. In both the groups the existence of the following variants were investigated.
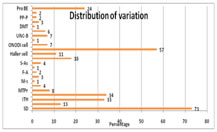
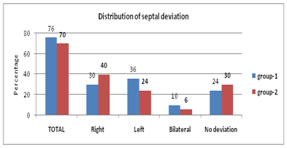
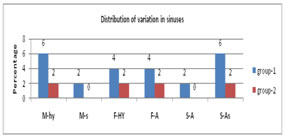
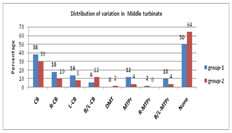
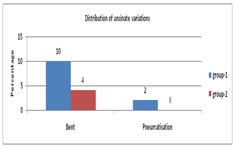
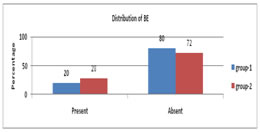
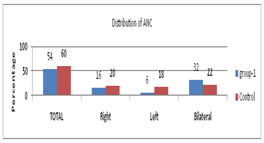
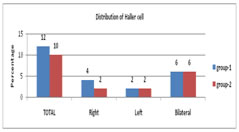
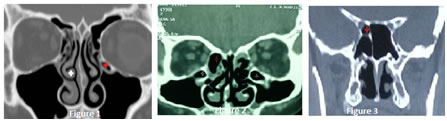
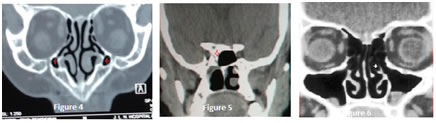
Statistical analysis The CT scans were evaluated for the presence of anatomic variants of the sinonasal cavities. The prevalence of anatomic variants of the paranasal sinuses and nasal cavity was calculated for each group. For all comparisons conducted in this study, p < 0.05 was considered to be statistically significant. Data is analyzed in terms of the number, percentage of the variations according to side and sex. Quantitative data analyzed using mean, Standard deviation, unpaired t test (to compare both groups). Qualitative data analyzed using Percentage, Chi square test. Statistical analyses made using ‘Statistical Package for the Social Sciences'(SPSS) version 18.0 software program. RESULTS The most common anatomic variation in both the groups was detected as septal deviation (73%) followed by agger nasi cell which was noted in 57 (57%) patients. The rates of other anatomical variations were concha bullosa 34 (34%), inferior turbinate hypertrophy (33%), haller cells (11%), frontal cells (18%), onodi cell (7%), paradoxical middle turbinate 8(8%), bent uncinate process in (7%), supraorbital cell (6%) as seen in graph 1. Some other uncommon variants were seen in this study like crista galli pneumatisation (3%), maxillary sinus hypoplasia (4%), frontal sinus aplasia (2%),double middle turbinate (1%), linoid and pterygoid process pneumatisation (2%) each. Figure 1: Anatomical variations distributions of all 100 patients Graph 2 described the septal deviation and septal deviation (SD) was seen in total of 73 (73%) patients in both groups. In 35% of patients it was right sided whereas in 30% it was left sided. Bilateral or ‘S’ shaped deviations was seen in 8(8%) of total patients. No SD was detected in 27 (27%) of patients as seen in graph 2. There is no statistical significance between both the groups in septal deviation. Figure 2: Distribution of septal deviation in both groups As described in graph 3, we observed maxillary sinus hypoplasia (M-hy) in total of 4 (8%) patients, 3 (6%) patients in group-1 and 1 (2%) patient in group-2. Septate maxilla (M-s) was seen in 1 (2%) patient in group-1 and none in group-2. In frontal sinus we observed frontal sinus hyperplasia (F- HY) in total 3 (6%) patients, 2(4%) in group-1, 1(2%) in group-2. Frontal sinus aplasia (F-A) was seen in 3(6%) patients, 2 in group-1 and 1 in group-2. In sphenoid sinus we observed presence of accessory septum(S-A) in 4 (8%). patients, out of which 3(6%) belonged to group-1 and 1(2%) to group-2.m Sphenoid sinus aplasia (S-As) was seen in 1 (2%) patient belonging to group-1. All the results were statistically non-significant on comparison in both the groups. Figure 3: Distribution of variations of sinuses Graph 4 describe the middle turbinate variations as we found that concha bullosa (CB) was identified among 34(34%) of total 100 patients. This was identified in the right among 14(14%), in the left among 11(11%) and in both left and right in 9(9%). Paradoxical middle turbinate (MTPr) was seen in total of 8 (8%) patients, out of which 6(12%) patients were in group-1 and only 2 (4%) in group-2. Bilateral paradoxical middle turbinate was seen in total of 7 (7%) patients. We saw another uncommon variant double middle turbinate (DMT) only in 1 (2%) patient of group-2. Figure 4: Distribution of variations in Middle turbinate As shown in Graph 5-10, the ethmoid sinus variations has been studied in both the groups and no statistical significance was found in all the ethmoid sinus variations. Figure 5: Distribution of uncinate variation Figure 6: Distribution of enlarged Bulla Ethmoidalis Figure 7: Distribution of Agar Nasi cells Figure 8: Distribution of Haller cells Figure 9: Distribution of Onodi cells Figure 10: Distribution of Supra Orbital cells The rates of anatomical variations in two groups were calculated separately and compared with each other. There were no significant statistical differences between the groups concerning the rates of all these mentioned variations. Figure 1 Figure 2 Figure 3 Figure 4 Figure 5 Figure 6 Figure 1: Bilateral paradoxical middle turbinate (white star) and Left Haller cell (red star); Figure 2: Bilateral Haller cells (white star) and Right side Prominent Bulla Ethmoidalis (Red star); Figure 3: Right side Onodi cell; Figure 4: Bilateral Maxillary Hypoplasia; Figure 5: Right Sphenoid aplasia; Figure 6: Left Uncinate process pneumatisation
DISCUSSION The anatomy of the PNS is variable and very complicated, so it becomes important to appreciate the clinical and surgical significance of these anatomic variations. Paranasal sinus CT in coronal plain is one of the main methods used to demonstrate the anatomy and stages of inflammatory diseases preoperatively. The advantage of this approach for endoscopic sinus surgery is that; it can provide anatomical and pathological image with the same perspective to the surgeon. Hence CT examination has become a screening technique for patients who are candidate for FESS. One of the most common variations of sinonasal region is septum deviation. Prevalence of nasal septum deviation has been reported to vary from 20% to 79%25 Mean rate of septum deviation in the literature is about 47.77% 26. In the present study, a moderate frequency of 73% was observed for septum deviation. There are studies8,11 stating that nasal Septal deviation could lead to CRS by coming in contact with enlarged turbinate (hypertrophic or bullous), thus narrowing meatus or impairing normal mucociliary activity and mucus drainage, while there are many other studies16, 21 mentioning lack of any association between septum deviation and CRS. Dasar et al6 noted a frequency of 59.5%, Shpilberg et al19 noted a very high frequency of 98.4%, Sarafraz et al18 48%, Kaygusuz et al12 72.3% in study and 73.5% in control group which was very close to our study. In our study, the incidence of Concha Bullosa (CB) in the group-1 and group-2 were found 38 and 30% (statistically insignificant) respectively in accordance with the literature. In another study by Kaygusuz et al12 CB was seen in 41.5 % in study and 52.9 % in control group (not significant). Sarafraz et al18 observed CB in 66% of diseased and 34% in the control group. CB is thought to affect the OMC by narrowing the nasal passage. Differing definitions of concha bullosa are likely to account for the variation in reported prevalence. The presence of CB is associated with increased risk of sinusitis in the study of Sarafraz et al18. However, Vincent T et al24, Shpilberg et al19, did not reach an evidence of increase in the incidence of CB compared with CRS. Paradoxical middle turbinate in simple words is, when the convexity of the middle concha is on the lateral side. The major consequence of this anatomical variation is narrowing of the middle meatus which can lead to obstruction of infundibular drainage. Various studies showed that presence of paradoxical middle concha could not simply participate in the etiology of CRS, but the size and degree of convexity of the MT may be an important factor to cause the obstruction leading to CRS. Sarafraz et al18 noted frequency of 6.1%, Shpilberg et al19 reported a frequency of 15.6%, Kaygusuz et al12 observed 13.8% in study group and 11.7% in control group. We observed a total frequency of 8%, 12% in group-1 and 4% in group-2. Maxillary sinus hypoplasia was identified in 4(4%) patient. Knowing the presence of serious maxillary sinus hypoplasia before FESS would lower orbital penetration risk during surgery.4 Frontal and Sphenoid sinus aplasia was present in 3% and 1% of patients respectively. In a study by Kaygusuz et al12 the rates of Agger nasi cells were 55.8%, 64.6% in study and control group respectively, and no significant correlation was found between the rate of AN cells and severity of the frontal sinusitis. Gupta et al9 reported an incidence of 68.8%, whereas Mamatha et al13 had 50% prevalence in their study. In our study, ANC were 57%, 54 % in group-1 and 60% in group-2 respectively .The effect of ANC on the drainage way of frontal sinus has been widely discussed in many papers. In the study of Fadda et al8. ANC were detected in 24.3% of cases, and was associated with frontal sinusitis in multivariate analysis. On the other hand, fewer studies have contrary results. Sarafraz et al18 reported the rate of ANC as 23%, and there were no significant relationship between ANC and frontal sinusitis. Haller cell (infraorbital ethmoid cell) if enlarged can constrict the posterior aspect of the ethmoidal infundibulum and superior medial portion of maxillary sinus ostium. Many authors thought that HC as a possible etiologic factor in CRS due to their negative influence on maxillary sinus ventilation by narrowing the infundibulum and ostium depending upon its degree of pneumatisation and size. The rate of HC was ranging from 2 to 56.6% in the literature62. In our study, the rates of Haller’s cell were found 12 % among the cases group-1and 10% in group-2. Out of this accessory septum in sphenoid is of utmost importance, great attention must be paid to the insertion of the main and accessory septa. During transseptal sphenoidectomy care must be taken of the septum manipulation. Preoperative CT diagnosis taken into consideration it’s insertion to the walls of the carotid or optic canal must be sought off. With extended applications of endoscopic sinus surgery into the skull base this has become even more important now days. Because of the foregoing reasons, the preoperative radiological evaluation using CT has to play a major role in patients with indicated endoscopic surgical procedures in the sinuses or the sellar region. It is difficult to comment on whether sinus anatomy can predispose to development of disease due to obstruction of sinus outflow tracts based on this study. The numbers are too small for statistically significant analyses to be concluded between normal and diseased sinuses in this study.
CONCLUSION The results of this prospective observational study showed Septal deviation as the commonest anatomical variation of nose and paranasal sinuses followed by agger nasi cell, concha bullosa respectively. Few of the very uncommon variations were also seen, namely paradoxical middle turbinate, crista galli, clinoid process and pterygoid pneumatisation, Maxillary hypoplasia, frontal and sphenoidal aplasia. Anatomic variations in paranasal sinuses can lead to recurrent sinusitis, mainly due to impaired sinus drainage and ventilation. Understanding the different variations and location is very important. However, in our study no statistically significant correlation was seen in the prevalence of sinonasal anatomical variations in both the groups. This may be due to the fact that we found variations with severity of mild grades in our study population. This study using computed tomography scan as the main tool underlined the fact that sinonasal area has very high rate of anatomical variations. Careful assessment of CT in patients is necessary, especially in those undergoing FESS. However, for patients who are planning to undergo FESS or other skull base surgery, it is also important to be aware of certain anatomic variants, such as sphenoethmoidal (Onodi) cells, pneumatisation of anterior clinoid processes, supraorbital cells, infraorbital ethmoidal (Haller) cells, pneumatisation of the dorsum sella, and dehiscence of the lamina papyracea. Failure to recognize these variants is associated with a higher rate of surgical complications. The limitation of the study are as normal population has not been taken into consideration to compare with the diseased group because the invasive radio-imaging (CT scan) is used to study the variations and there is no randomisation of the study hence chances of biasing is always there.
REFERENCES
|
|
 Home
Home