Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 3 - March 2019
Is “Headache”, ‘head’ of all aches – where are we ‘head’ing to…???!!!
Venkatesh Ballal1, Sphoorthi Basavannaiah2*, B T Subramanya3, Lohith S4
1,3,4Associate Professor, Department of ENT, Subbaiah Institute Of Medical Sciences, NH-13, Purle, Holebenavalli Post, Shimoga-577222, Karnataka, INDIA. 2 Assistant Professor, Department of ENT, Subbaiah Institute Of Medical Sciences, NH-13, Purle, Holebenavalli Post, Shimoga-577222, Karnataka, INDIA. Email: sphoorthi86@rediffmail.com
Abstract Background: Headache is one of the most common complaint people come across at some point in their life. It is one of the prime concerns to both surgeons and clinicians in the present day scenario due to its varied presentations. Headache has a diverse genre ranging from simple stress to complex stroke. Aims and Objectives: To find out cause for headache from Otolaryngologist’s perspective and its impact on health and how lifestyle variations can better the situation and bring in positive and progressive changes in day to day regime. Methodology: 119 patients who consulted the ENT outpatient department were clinically evaluated and diagnosis was made and treated accordingly. Results: Interlinking of Migraine with Laryngopharyngeal reflux disease was found to be the most common cause for headache at our set up. Conclusion: Going by the present trend, headache in any form should not be neglected. It can be mainly avoided by inculcating changes in daily routine and inhibiting stress which is an innate triggerer to headache in the present day setting. Key Word: Headache, Laryngopharyngeal reflux, Migraine, Stress.
INTRODUCTION Since over a decade, both surgeons and physicians are in a dilemma regarding arriving at a diagnosis for headache pertaining to its diverse causes. Headache can be result from a minor stress or a major stroke, hence timely action is mandatory due to its various differentials. On daily basis, we come across mixed patient presentations with regards to headache as a primary or secondary symptom or as an associated symptom which has indeed made way for a second thought to prescribe apt management algorithm. AIMS AND OBJECTIVES
MATERIALS AND METHODS Study design: Prospective follow up study. Place of study: Tertiary Care Hospital, Subbaiah Institute Of Medical Sciences, Shimoga. Study period: 2 years (from December 2016 to December 2018). Selection criteria: A random sample of 119 patients who consulted the ENT outpatient department with headache were clinically evaluated. Inclusion criteria
Exclusion criteria
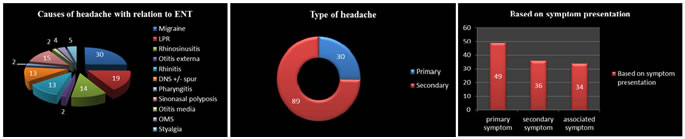
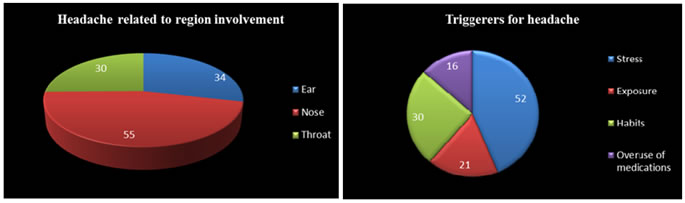
Procedure of the study: A random sample of 119 patients who consulted ENT outpatient department with headache were selected for the study. A thorough history with detailed ENT with Head and Neck examination was done for all of them to evaluate the cause for headache. The relevant laboratory, radiological investigations were done to arrive at a diagnosis. Treatment protocols were prescribed based on the diagnosis. Informed written consent was taken during the study period. Ethical clearance has been taken from Institutional Ethics Committee before the start of the study. Statistical analysis: is done with the help of Open-epi software and Chi-square test is applied. RESULTS Figure 1: Figure 2: Figure 3: Figure 4 Figure 5 Figure 1: Causes for headache shown in “Exploded pie 3D” representation, Figure 2: “Doughnut diagram” showing type of headache at our set up. Figure 3: Based on symptom presentation of headache during consultation shown in the form of “Stacked column” representation. Figure 4: Causes for headache are shown here as per area of concern in “3D pie diagram”. Figure 5:“Pie diagram” showing list of triggering factors for headache.
Table 1: Chi- square test was done to find the difference between the proportion of symptom presentation across region involvement with relation to ENT. The test showed that proportion is significantly different across region involvement with Chi-square value as 106.6, with 4 degrees of freedom and p-value < 0.0001 at 5 % level of significance.
DISCUSSION Due to frantic regime in our present day, headache1,17,29 is one of the most common presentation at our outpatient department these days. As per WHO survey, majority of adults worldwide will experience headache in a year at some point or the other in their life. Headache2,8,16,24,31 are broadly classified into 2 types- Primary and Secondary headache. Primary headache3,14,26 occur due to over-activity of pain-sensitive areas like nerves, blood vessels and muscles of head and neck or due to changes in chemical activity of brain. Its causes are Migraine, Cluster headache, Tension-type headache, New daily persistent headaches. While secondary headache4,11,28,32 occur as a result of conditions that stimulate the pain- sensitive areas. Its causes are- Rhinitis (Acute, Chronic, Allergic), Rhinosinusitis (Acute and Chronic), Deviated nasal septum with spur with inferior turbinate hypertrophy, Sinonasal polyposis(Ethmoidal polyposis, Antrochoanal polyp), Septal abscess, Vestibulitis, Sluder’s neuralgia, Otitis externa(Localised, Generalised, Malignant, Herpes zoster oticus(HZO), Perichondritis, Otitis media (Acute, Chronic), Migraine, Pharyngitis, Laryngopharyngeal reflux disease (LPR), Oromandibular syndrome/ Temperomandibular (TMJ) joint arthritis, Styalgia, Rebound headaches(associated with substance abuse, alcohol, excess pain medications, dehydration), Trigeminal neuralgia, Dental pain, Thunderclap headaches(as a result of life threatening conditions: Encephalitis, Meningitis, Brain tumors and abscess, Hydrocephalus, Intracranial hemorrhage, Cerebrovascular thrombosis, ruptured/unruptured aneurysms, exposure to toxins or chemicals), Traumatic headaches( Post-concussion/ Head trauma), ‘Hangover’ headaches, Refractive errors, Glaucoma, Stroke, Other rare causes- Influenza, Panic attacks, Bruxism, CO poisoning, Brain–freeze or ‘Ice-cream’ headaches, Vaccum headache. Now-a-days, people often desire for extravagant luxury in between their chaotic daily routine. Due to this, they overlook upon meek sources of headache but when they get anxious, the focus is automatically diverted towards rarest causes of headache. Life can be made modest by adapting easy, essential and practical lifestyle measures which can sort out most of the basic concerns of headache at the earliest. With every passing day there are uncountable changes happening around us which makes leading simple life complex5,12,23. In this “jet speed” mode to earn and lead a lavish lifestyle, we often tend to neglect or overlook our health in order to fulfil our goals and desires. Life seems like a “snake and ladder” where people strive to attain and achieve the impossible while reach and range towards greater heights in no time at the cost of nature’s most precious gift to us that is “Health”. As per ancient saying “Health is Wealth” but the present situation has become vice versa. In this process of touching skies, outbursts of stress gets released within us time and again as bouts of headache6,13,22. All the 119 patients were evaluated based on their symptomatology and treated accordingly following necessary investigations being done. People with Migraine (30) were given Tablet. Sibelium (Flunarizine)7,15,21,30 for a period of 3 months to be taken once at bedtime. They were followed up initially once in 15 days for first 2 visits and later on once a month. Along with it, analgesics, antacids were given for their accompanying symptoms- nausea, heaviness of head. Patients responded well with this treatment and have shown good results on follow up. But, moreover it is the incorporation of changes in their daily regime that has brought in desirable and satisfactory results to the patients. People with LPR(19)were managed with antireflux treatment for 1 month along with major lifestyle modifications that has brought a major impact in their day to day scenario, when followed up9,18,25. While Rhinosinusitis(14), acute were treated symptomatically with broad spectrum antibiotics, analgesics, nasal decongestants, topical steroids and chronic cases were investigated as adequate treatment was already been given and were treated for the same and accordingly FESS+/- Septoplasty was done under General anaesthesia10,19,27. Similarly, Sinonasal polyposis(15)were treated symptomatically with broad spectrum antibiotics, analgesics, nasal decongestants, topical+/- oral steroids. A proper course of steroids preoperatively is very useful from both patient and surgeon point of view. After adequate conservative line of treatment, FESS (mini/ full house) was done under General anaesthesia2,13,20. While, (13)patients with Rhinitis (Allergic/ Acute)6,18,30 were treated symptomatically. Patients with Acute rhinitis were treated on medical line with oral antibiotics, antihistamines, topical decongestant sprays. But, patients with Allergic rhinitis were treated after getting their absolute eosinophil count (AEC) test. Positive test showed 3-4 times raised values than the normal range (> 440). They were treated with Diethylcarbamazine (DEC) thrice daily for a period of 15 or 21 days after a dose of deworming. In allergic rhinitis, DEC acts as a blocking agent of mediator release in particular of Slow reacting substance of Anaphylaxis (SRS-A) from the sensitised basophil or mast cell. In (13) patients with DNS4,16,23, they underwent Septoplasty after taking treatment for their acute symptoms. While the remaining patients with ear (4) and throat (11) related pathology were treated accordingly as headache was an associated symptom in them which subsided on itself by treating the cause per se. Secondary headache8,17,25 forms the bulk of patients when compared to Primary headache. As (25%) of Migraine falls under the category of Primary headache, the rest (75%) patients include all other causes of Secondary headache. Headache has 3 basis of presentation10,14,27- Primary, Secondary and as an Associated symptom. (49)patients presented as primary symptom that is (41%) of which among Ear- Migraine (30) which is a central vestibular disorder, Otitis externa (1), among Nose- Rhinosinusitis(14), Rhinitis (3), among Throat- Pharyngitis (1). (36) patients presented as secondary symptom that is (30%) of which among Ear- Otitis externa (1), among Nose- DNS (13), Rhinitis (10), Sinonasal polyposis(9), among Throat- Pharyngitis (1), LPR (2). (34) patients presented as associated symptom that is (29%) of which among Ear- Otitis media (2), among Nose-(6) Sinonasal polyposis (6), among Throat- OMS (4), Styalgia (5), LPR (17). With respect to region involvement for headache, Ear comprises of (34) patients that is 29%[ Migraine:30, Otitis externa: 2, Otitis media: 2], Nose comprises of (30) patients that is 25% [ LPR:19, Styalgia:5, OMS: 4, Pharyngitis:2] and Throat comprises of (55) patients that is 46% [ Sinonasal polyposis: 15, Rhinosinusitis: 14, each 13 of DNS +/- spur and Rhinitis]. As famously told by Lipton “The way stress gets translated into physiology is through perception. Things are either or not stressful, but thinking makes them so”. But as an add on to headache, there are lots of stimulating factors which aggravates headache taking it to another level. These triggerers are- Stress (52 patients) (44%) that comprise of emotional attachments from family and friends, work pressure, tension, anxiety, depression, Exposure (21 patients) (18%) that includes pollution: air/ noise, lightning, climatic changes, allergens: dust mite, pollens, household chemicals or perfumes, Habits (30 patients) (30%) which contains intake of spicy/ cold/ sour/ oily food plus intake of sweets, tea, pickles, changes in sleep patterns, skip meals, fast or diet, habitual to smoke/alcohol/tobacco or betel nut chewing, Overuse of medications (16 patients) (13%) as now it has become an easy way of accessibility to pharmacy outlets for any cheap medications for temporary relief1,19,28,31. Though with a variety of causes of headache, the most common cause encountered at our OPD is “Migraine”. Migraine3,15,26,32 is both surgeon’s as well as physician’s diagnosis dilemma. Headache results from signals interacting among the brain, blood vessels and surrounding nerves. During the episode, specific nerves of the blood vessels are activated and send pain signals to the brain. It is unclear why these signals are activated in the first place. There is a “migraine pain center” or generator, in the mid-brain area. A migraine begins when overactive nerve cells send out impulses to the blood vessels. This causes the release of prostaglandins, serotonin, and other substances that cause swelling of the blood vessels in the vicinity of the nerve endings resulting in pain. On the other hand, these pain sensitive areas are triggered inadvertently by reflux due to bizarre and untimed food habits. Both MIGRAINE and LPR are usually interlinked to each other and it is better to avoid stimulating factors and provide relieving factors as far as possible at the earliest7,15, 22
In view with the data from the study9,11,20,24, following objectives are fulfilled and the results are arrived at- Going with the causes of headache in relation to ENT, Migraine topped the list among all the causes. Moreover it is the intermingling of both primary and secondary headache which is found to be the most common presentation for headache at our set up as both are interconnected in its occurrence and most of them had both Migraine + LPR (41%)5,12,21,24 but unaware with the way of its presentation. Headache in most patients was seen as a Primary presentation. As per the data, Nose by all means otherwise is the most common area involved in headache. Stress was found to be the most common synergistic factor either directly or indirectly seen affecting the general population with regards to health issues in one way or the other in the study. Headache is most commonly presented as a primary symptom with the combination of Migraine and LPR being the most common cause of headache at our OPD, which is a mishmash of both primary and secondary type of headache. Considering the present day state, changes in the lifestyle is of paramount prominence which itself is a useful tool for any kind of triggerers of headache or any health issues for that matter.
CONCLUSION Any form of headache either minor or major should not be neglected. As it is often seen that people have persuasion towards pharmacy for medicines as their “first choice approach” rather prefer getting a consultation done. In addition to it, putting in practice dietary modifications in the lifestyle on daily mundane can surmount any intruding, interfering, interruptive stressors for headache or any concerns to health.
REFERENCES
|
|
 Home
Home