Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 3 - March 2019
Our experience Seema Patel1, A Z Nitnaware2*, Vaibhav Lahane3, R T Pawar4
1Associate Professor, 2Professor and HOD, 3SR, 4Assistant Professor, Department of ENT, GMC Nagpur-440003, Maharashtra, INDIA. Email: drpatelseema@gmail.com, drpatelseema@gmail.com, vaibhavlah09@gmail.com, ram.pawar10@gmail.com
Abstract Head and Neck cancer (HNCA) is a recognized major public health concern all over the world. Aims- To study types of cancers at various subsites of head neck regions and treatment modalities.A retrospective study including 1257 patients with HNCA presented to ENT OPD at GMC Nagpur between period January 2013 to February 2018. Detailed history, clinical, cytological and radiological examination was done. Oral cavity cancers were 621(49.40%), followed by larynx (20%). Maximum patients between 50-60 years with male preponderance except for thyroid. Surgery was the mainstay treatment modality for oral, salivary, nasal and thyroid cancers whereas laryngeal, hypopharyngeal and oropharyngeal cancers were managed with chemo-radiotherapy. Early detection and widespread awareness should be done to overcome such major public health issue. Early detection and proper selection of treatment modality is key for successful outcome. Key Word:Head neck cancers (HNCA), Squamous cell carcinoma (SCC), Surgery, Chemotherapy, Radiotherapy.
INTRODUCTION The global cancer burden is estimated to have risen to 18.1 million new cases and 9.6 million deaths in 20181 (WHO 2018). Worldwide, head neck cancers (HNCA) represent the sixth most common neoplasia and accounts for 6% of all cases, being responsible approximately for 1%–2% of tumor deaths (2). Head neck cancers (HNCA) are a heterogeneous disease, encompassing a variety of tumors that originate in the hypopharynx, oropharynx, lip, oral cavity, nasopharynx, or larynx and has a variant demographic profile, etiological factors, food and personal habits. HNCA can lead to structural and functional deformities depending on the site, size and pattern of spread. More than 90% of head and neck cancers are squamous cell carcinoma (SCC).Because of complex nature of head neck cancers, management needs multidisciplinary approach not only for treatment but also in supportive care (swallowing, nutritional, dental, and voice). The treatment options for HNCA are surgery, radiotherapy (RT) and chemotherapy (CT). The main goals of therapy are:
In present study, management of patients with head and neck cancers with various modalities were studied over 5 years with an aim to study the management of choice as per the type and stage of disease at our centre and patients compliance for treatment modality.
AIMS AND OBJECTIVES To study types of cancers at various subsites of head neck regions and treatment modalities.
MATERIALS AND METHODS A retrospective study conducted at tertiary hospital Government Medical College, Nagpur between the period of January 2013 to February 2018. This study included 1257 cases of head and neck cancers presented to ENT OPD. Detail history and examination was done in all patients. History related to personal addiction habits like tobacco, alcohol and smoking was noted in details. Radiological investigations like x ray, USG, CT scan and histopathological examination of biopsy tissue were done in all cases. Staging of the cancer were done according to TNM staging. Various sites of Head and neck region included in present study were; oral cavity, oropharynx, larynx, Hypopharynx, nose – paranasal sinuses –nasopharynx, salivary gland, thyroid gland, occult primary with neck secondaries and ear. Treatment modalities like surgery with or without plastic reconstruction followed by postoperative radiotherapy, radiotherapy alone, chemotherapy and radio-chemotherapy. Treatment modalities were advised as per stage of disease, patients’ willingness and general conditions of patients.
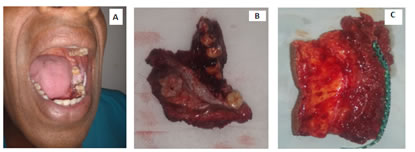
RESULTS AND DISCUSSION Head and neck cancers are major health problem and have become one of the ten leading causes of death in India. Takiar and Vijay (2011) have reported an increase of 55.8% cancer incidence in past 2 decades as per the national urban registries3. Data from population based registries under NCRP indicate that the leading sites of cancer are the oral cavity, lungs, oesophagus and stomach amongst men and cervix, breast and oral cavity amongst women. The head and neck region constitute several delicate, intricately organized structures vital for basic physiological needs and crucial for appearance, expression and social interactions. HNCA can lead to structural and functional deformities depending on the site, size and pattern of spread. Thus treatment of head neck cancers need proper counseling, nutritional and swallowing evaluation, dentary preparation, and pain management before, during, and after concomitant treatment. Multidisciplinary approach should include ear, nose, throat surgeon, radiologist, radiation oncologist and medical oncologist, dietician, dentist, pain physician, and swallowing physician. Proper selection of patients is essential for good outcome of treatment modality. Present study included 1257 cases of proven HNCA out of which, 910 were males and 347 were females with Male to female ratio of 2.6:1. Age range was 23 to 84 years with mean age of 52.89 years. Maximum patients were in the age group of 50 – 60 years. Four percent patients were in less than 30 years age group. Oral cavity cancers contributed maximum patients 621 (49.40%) followed by laryngeal cancers 252 (20%) (Table 1). There was male preponderance in all subsites of head neck except in thyroid and postcricoid cancers which showed female dominance. Stage of presentation was noted in all cases (table 2). Various treatment modalities done were; Surgery (WLE of primary lesion with neck dissection with or without plastic reconstruction), radiotherapy, chemotherapy, combined therapy. All patients who underwent surgery were subjected to postoperative radiotherapy irrespective of margin and nodal status. Oral cavity:- Total patients 621 (49.40%) including 440 (70.85%) males and 181 (29.15%) females with M: F ratio of 2.43:1. Maximum patients were in the age group of 40 – 50 years with youngest patient of 29 years. Growth or ulcer in oral cavity was the most common complaint. Tongue was involved in 220 (35.43%), buccal mucosa (alveolobuccal complex + hard palate) in 280 (45 %), alveolus 107 (17.23%) and lip in 14 (2.25%) patients. Maximum patients presented in stage III and IV except in case of tongue where maximum patients were in stage I (29%) and II (41.82%). Late stage presentation may be attributed to; remote rural population, lack of awareness among patients, relatives and referring doctors. Sharma P et al(4) and MS Alam5 reported buccal mucosa as most common site among oral cavity cancers. Akheel Mohammad et al(6) reported tongue cancer (32.38%) as most common subsite whereas Shenoi P et al7 showed mandibular alveolus as most common subsite followed by buccal mucosa. In our study, two types of oral cavity cancers; SCC 604 (97.26%) and verrucous carcinoma 17 (2.74%). In a study by Shubha P Bhat et al8SCC was the most common histological type (82.6% cases) followed by Verrucous carcinoma (7.9%).In present study, out of 280 patients of buccal mucosa + alveolobuccal complex, 199 (71%) patients were managed with surgery. In cases of tongue and alveolar cancers, 181 (72.27%) and 88 (82.24%) underwent surgical treatment. In case of tumours in proximity with bone, subperiosteal striping or marginal mandibulectomy was done and in case of obvious cortical erosion segmental resection was undertaken (figure 1).In case of lip cancers, surgical management was done in 11 cases and chemo-radiotherapy was advised in 3 cases. Reconstruction was decided depending upon the length of the defect (Table 3). Supraomohyoid neck dissection (SOND) was done in N0 neck. But in cases of node positive necks and primary tumour size more than 4 cm, modified radical neck dissection (MRND) was performed. Patients with advanced stage of primary cancer, medically unfit for surgery and not willing for surgery were managed with radiotherapy. (Table 4) We documented recurrence and margin positivity in 4 cases each, of alveolobuccal complex which were managed with chemo-radiotherapy. Among tongue cancers 2 cases had posterior margin positive which were excision with 1 cm margin. 3 cases had recurrence which were managed with palliative chemotherapy. The periosteum itself is relatively resistant to tumour spread and close proximity of the tumour with no evidence of mandibular invasion does not normally mean that extensive jaw resection is necessary. In this situation subperiosteal stripping of the specimen from the bone, or possibly a marginal resection, is all that is needed. This type of partial resection is done when there is definite evidence of bone involvement is more debatable and it is usually not feasible in the thin edentulous jaw9. Post-operative radiotherapy was advised in all patients who underwent surgical management irrespective of margin and nodal status. Post-operative concurrent chemo-radiotherapy was given in patients with positive margins or extracapsular spread in neck nodes. Two prospective randomized trials of adjuvant chemo-radiotherapy have shown that patients who have extracapsular extension of disease in metastatic cervical lymph nodes and those who have positive margins have a significant improvement in local regional control and disease free survival by addition of chemotherapy to post-operative radiation therapy compared to post-operative radiation therapy alone10. The ultimate goal of treatment of cancer of the oral cavity is to eradicate the disease, preserve or restore morphological and functional aspect, minimize the sequelae of treatment and prevent recurrence. The currently available treatment modalities include surgery, radiotherapy, chemotherapy, combined modality treatments and primary and secondary prevention strategies including lifestyle changes as well as chemoprevention. Curative surgery involves resection of tumour with 1-2 cm margin and subsequent reconstruction of the tissues with local or distant flaps. The size and location of the primary tumour determine access procedures. Many tumours in the anterior aspect of the oral cavity can be accessed via the transoral route which maintains the circumferential muscular sphincter. However, as tumours increase in size and become more posteriorly placed, a controlled resection may only be possible by performing either a lingual release or resorting to lip-split and mandibulectomy. Neck dissection: The supraomohyoid dissection covers the nodal sites most often affected and may be used electively as a sampling procedure in node-negative necks (11). With increasing size, the risk of regional lymph node metastases increases bringing into consideration the need for elective treatment of the clinically negative neck, which is at risk of harboringmicrometastases. In our study we addressed neck nodes with MRND if primary tumour size is more than 4 cm even if they were negative for metastasis. Tumors of the oral tongue and floor of mouth have an increased risk of lymph node metastases compared to similar staged lesions of the hard palate or upper gum. Tumors located in the anterior part of the oral cavity have a lesser risk of dissemination to regional lymph nodes compared to similar staged lesions in the posterior part of the oral cavity or oropharynx. The presence of clinically palpable cervical lymph node metastases requires a neck dissection as an integral part of surgical treatment. The extent of neck dissection, however, varies depending on the extent of nodal metastases and the location of palpable lymph nodes. Reconstruction: Defects after resection of primary tumour needs reconstruction for anatomical and functional integrity. Out of 199 surgically managed cases of alveolobuccal mucosa complex, 148 (74.37%) patients required reconstruction. Nasolabial flap, PMMC flap, anterolateral thigh, forearm flap and free fibula flap were the tissue of choice for reconstruction. (Table 4)Loss of a significant part of the tongue, floor of mouth or buccal mucosa, and segment of the mandible need reconstructive surgery. Larger defects of the tongue exceeding one half of the tongue or large surface areas of the floor of the mouth, gum and buccal mucosa require a free tissue transfer. A radial forearm free flap provides excellent tissue for resurfacing mucosal defects and is also an excellent choice for reconstruction of tongue. Fibula free flap reconstruction is currently the choice of reconstruction for defects of mandible12. Other free flaps available for mandible reconstruction are; the iliac crest, scapula, and the radial forearm osteocutaneous flap. The choice of a particular free flap depends upon the location and the length of mandible reconstruction, as well as the need for soft tissue and mucosal lining or skin coverage at the site of resection. Larynx – 252 cases were documented with laryngeal cancers with age range of 37 to 84 years. Maximum patients were in the age group of 55-75 years with mean age of 61.12 years. Male to female ratio was 13.8: 1. Dysphagia or odynophagia was the most common complaint. Change in voice was present in 120 (47.6%) cases. 102 (40.47%) cases presented with stridor to emergency room and tracheostomy was done. Supraglottis 174 (69%) was the most common site involved followed by glottis 70 (27.77%) and subglottis 8 (3.17%). 60.75% patients presented in stage I and II (Table 3). All cases were of SCC. According to recent studies, larynx was most common site of HNCA13. N Arora et al(14) observed supraglottis as most common site for tumour localization and common stage of presentation as T1 and T2 followed by T3 and T4.242 patients were managed with radiotherapy and 10 cases were subjected to total Laryngectomy followed by postoperative radiotherapy. Majority of patients presented in early stage thus radiotherapy was the choice of treatment. Less number of Laryngectomy can be because of; unwillingness to undergo surgery or to remove voice box, unwillingness to accept defect, advanced locoregional disease, comorbidities and some were unfit for surgery.Adeel M et al(15), in their study reported 34% refusal rate for surgery (Laryngectomy). There is hardly any data addressing the issue of salvage Total Laryngectomy refusal in developing countries, but the numbers are likely to be high because of lack of education, poverty, social stigma of loss of voice, permanent tracheostomy and varying spiritual believes that leads them to seek non-medical treatment. Therefore, many operable diseases progress to inoperable.For early laryngeal tumors (T1, T2), transoral surgery or radiotherapy alone has shown comparable results16, whereas surgery followed by radiotherapy is considered for advanced cancers17. More recently, concurrent chemo-radiotherapy is replacing surgery as a treatment modality for advanced laryngeal cancers with almost similar outcomes18,19. Oropharynx: Carcinoma oropharynx were in 85 (6.76%) cases.Various subsites included under oropharyngeal cancers; base of tongue and vallecula 50 (58.82%), tonsil 25 (29.4 %), posterior pharyngeal wall 3 (3.52%) and soft palate 7 (8.23%). Dysphagia or odynophagia was noted in all cases. All patients were in the age range of 45 to 79 years with mean age of 56.55 years and maximum patients were between 56-60 years group. Male to female ratio was 1.9:1. Biopsy showed; SCC 78 (91.76%) and Non-Hodgkin’s lymphoma of tonsil 7 (8.23%) cases. Majority of patients presented in early stage. Shetty et al20 diagnosed 22 cases of oropharyngeal cancer out of which 2 were lymphomas from tonsilar region. Shubha Bhat9 reported 11.8% cases of tongue base and tonsil cancers each. Patients with Nod-Hodgkin’s lymphoma were managed with chemotherapy. All patients with squamous cell carcinomas were managed radiotherapy or concurrent chemotherapy. For early stage (T1-T2 N0) oropharyngeal cancer, surgery or radiation is equally effective in loco-regional control. For patients with early nodal involvement (T1N1, T2N1), resection of the primary with neck dissection or adjuvant radiation is effective 21. For patients with more advanced T stage and nodal stage (Stage III, IV a and IV b), concurrent high dose cisplatin with radiation has been considered optimal treatment since the publication of the Intergroup trial22,23. In recent studies, outcomes of IMRT techniques for oropharyngeal cancers have been excellent 24. Hypopharynx – Total 85 (6.76%) cases of hypopharyngeal cancer were diagnosed. Pyriform fossa 57 (67%), postcricoid 18 (21.17%) and posterior pharyngeal wall 10 (11.76%). Age range was 43 – 76 years with maximum patients in 50-60 years with mean age of 53.67 years. Male to female ratio was 2.4:1. Female preponderance was noted in cases of postcricoid cancers 16/18 (88.88%). All cases had SCC. Maximum patients presented in early stage I and II (Table 3). 12 (1%) cases of upper oesophageal cancers were noted in present study.As maximum patients presented in early stage, our mainstay of treatment was radiotherapy. Concurrent chemotherapy was administered in some cases. Historically, total Laryngectomy (TL) with (partial or total) pharyngectomy used to be the gold standard in hypopharynx cancer treatment. However, since the introduction of CRT in the 1990s there has been a shift towards the use of organ preservation strategies. Early stage (I and II) disease can be treated with equal effectiveness with surgery or radiation. Early lesions of the hypopharynx can betreated by transoral resection or open partial laryngo-pharyngectomy with or without reconstruction25,26. Nose, paranasal sinuses (PNS) and Nasopharynx cancers: 31 cases of nasal – paranasal sinus cancer and 7 cases of nasopharyngeal cancers were present. Age range of 33 – 67 years, maximum patients between 40-50 years with mean age of 48.23years. Male preponderance with male to female ratio – 2.16 :1. In nose and PNS, SCC (50%) was the most common, followed by adenocarcinoma (18.42%), Non Hodgkin’s lymphoma (2.63%), olfactory neuroblastoma (7.89%) and rhabdomyosarcoma (2.63%). All nasopharyngeal cancers were SCC. Nose and PNS cancer patients were treated with surgical resection followed by postoperative radiotherapy. Nasopharyngeal cancers, Non Hodgkin’s lymphoma and rhabdomyosarcoma were managed with chemo-radiotherapy (table 5). Thyroid cancers: Total 79 (6.45%) cases of thyroid cancers, with age range of 23 – 69 years with maximum in 40 – 50 years. Female preponderance with M: F ratio of 1: 2.59 was noted. Papillary cancer – 50 (63.29%), Follicular cancer – 12 (15.19%), Medullary cancer – 2 (2.53%), Anaplastic cancer – 15 (18.98%). 20 cases were diagnosed on fine needle aspiration cytology and 30 cases were diagnosed on post-operative histopathology as papillary cancer. Papillary and follicular cancers were managed by total thyroidectomy with central compartment neck dissection. Lateral compartment neck dissection was undertaken in neck node positive cases. Postoperatively, Radio-Iodine131 ablation therapy was given if radioiodine scan showed residual disease. For medullary carcinoma, total thyroidectomy with central compartment node dissection was done in 2 cases. Decision for lateral neck node dissection was taken depending upon calcitonin level. If calcitonin level was more than 300 then lateral neck dissection was done. Anaplastic carcinomas were managed by palliative chemotherapy. Salivary gland cancers: 55 cases of salivary gland cancers in the age range of 29 – 72 years with maximum patients in 40 – 60 years. Male to female ratio – 2.33: 1. Various subsites included; Parotid – 35 (70%), Submandibular – 8 (16%), minor salivary gland and Sublingual –7(14%). Parotid gland was most commonly involved. Among various Histopathological variants adenoid cystic carcinoma was most common (56%) followed by mucoepidermoid carcinoma (42%). Mucoepidermoid carcinoma 20/35 (57.14%) was seen in parotid region whereas adenoid cystic carcinoma was observed in submandibular (100%) and sublingual gland (85.71%). Majority of patients presented in early stage.Subhashraj(22) reported adenoid cystic carcinoma (25%) and mucoepidermoid carcinoma (18%). Sardar et al(23) in his study on 75 cases of salivary gland tumour reported Mucoepidermoid carcinoma as most commonly occurring malignant tumor in parotid gland.All cases were managed with surgical resection with selective neck dissection with postoperative radiotherapy. 2 cases with advanced locoregional parotid mucoepidermoid cancers were managed with palliative chemo-radiotherapy (table 6).Complete surgical resection is currently the mainstay treatment for SGCs. Postoperative radiotherapy (PORT) can be used as an adjuvant therapy in patients with high-risk factors like
Elective treatment of the N0 neck remains a controversial topic. For patients with clinically positive cervical lymph node, therapeutic neck dissection (TND) is still strongly recommended at the time of primary surgery followed by adjuvant RT, regardless of histology or site. However, elective treatment of the clinical N0 neck remains a controversial topic. Treatment of the clinically negative neck included observation, elective ND, and prophylactic radiation 27,28.Primary RT may be applicable in inoperable tumours where palliation can be achieved. Occult primary with neck secondaries: 23 patients present to ENT OPD with swelling over lateral aspect of neck involving various level of neck nodes.Age range – 46- 78 years with maximum patients in age group of 50 – 60 years. Male to female ratio – 3.14: 1. Epithelial deposits of SCC were reported in FNAC of all cases. All patients were subjected to panendoscopies and radiological investigation like CT neck + thorax.11 Patients with N1 and N2 a disease were managed with neck dissection followed by postoperative radiotherapy. 12 patients with advanced stage disease were managed with concurrent chemo-radiotherapy. Metastatic carcinoma in the lymph nodes of the neck from an unknown primary is relatively rare, accounting for about 3% of all head and neck cancers.The proposed treatment options for neck metastases include neck dissection alone, radiotherapy alone or neck dissection with postoperative radiotherapy. A review of the literature suggests that the most promising results have been achieved with neck dissection followed by comprehensive irradiation whenever feasible29,30. Ear cancer: A 63 year female patient with swelling over left pinna, diagnosed as basal cell carcinoma was included in present study. Managed with wide local excision with skin grafting with postoperative radiotherapy (figure 2).
Table 1: Clinical profile of head neck cancer patients
Table 2: Stage of presentation
Table 3: Management of Lip cancers
Table 4: Treatment in oral cavity cancers
Table 5: Nose Paranasal sinuses and Nasopharyngeal tumour
Table 6: Salivary gland tumour
Figure 1: (A) SCC of left alveolobuccal complex. (B) WLE with segmental mandibulectomy done (C) free fibula graft harvested for reconstruction. Figure 2: (A) basal cell carcinoma of left pinna. (B) WLE done (C) Postoperative 3rd week after skin grafting.
CONCLUSION Head neck cancers are major public health burden. There are wide variations in risk factors, sites of involvement, geographical, and demographic characteristics. Widely spread educational campaigns against determinant factors should be introduced in order to reduce incidence rates. Health educational camps should be organized to aware people about signs of cancers, importance of early detection and treatment. Referring medical or paramedical personals should be trained to detect cancers at early stage. Early detection and proper selection of treatment modality are keys for successful outcome.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home