Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 3 - March 2019
Sialendoscopy: Our experience
Hiren Soni1, Nimisha Nimkar2*
1Associate Professor, 2Assistant Professor, Department of ENT, GMERS Medical College, Gotri-Vadodara, Vadodara, Gujarat, INDIA. Email: soni.hiren@hotmail.com
Abstract Background: We encounter various disorders of salivary glands mainly they are either neoplastic or non-neoplastic. Among non-neoplastic they are divided in acute and chronic sialadenitis. Major Salivary glands secrete through their respective ducts, pathology involving these ducts are major etiological factor behind chronic non neoplastic sialadenitis. Sialendoscopy is a miniature endoscope which allows us to approach the salivary duct through its opening. Methods: This research was carried out on all patients visiting ENT OPD with chronic non neoplastic salivary lesion with symptoms more than 1 month who were subjected to sialendoscopy. All patient’s data including age, sex, complaints with duration, site and side of lesion, sialendoscopy findings with routine ENT examination were recorded. Data of last one year were analysed and concluded. Results: among 20 patients who underwent sialendoscopy we found diagnostic sensitivity of 90.9%. with sialendoscopy we found sialolithiasis in 65% cases while ductal stricture was found in only 5% cases. Male and female were equally affected with middle age group of 16-50years having maximum number of cases. Conclusions: Salivary gland lesion incidence are not so common but they cause significant discomfort to an individual. Among them chronic disorders were treated with gland removal in neoplastic as well as non-neoplastic conditions. Sialolithiasis found to be most common cause of chronic non neoplastic sialadenitis. With advent of sialendoscopy we can accurately diagnose non neoplastic disorder and as well as treat them with good result and in this way we can preserve the gland. So sialendoscopy is a good tool to manage non neoplastic chronic sialadenitis. Key Word: sialendoscopy, chronic non neoplastic sialadenitis, sialolithiasis,
INTRODUCTION We have salivary exocrine glands in our body, which opens in the oral cavity with primary function of lubrication for swallowing and as first level of defence against micro- organisms. We have two major salivary glands submandibular and parotid on each side with sublingual gland and minor salivary glands. Among this parotid gland opens into the oral cavity by stenson’s duct and submandibular gland opens via wharton’s duct. We encounter various disorders of salivary glands mainly they are either neoplastic or non-neoplastic. Neoplastic lesions are again classified into benign and malignant lesions. While non neoplastic causes are divided into acute and chronic. Most of the chronic non neoplastic disorders are due to ductal pathology. The most common chronic ductal pathology is salivary stones which account for 60% - 70% of salivary duct obstructions. Majority of stones are found in Wharton’s duct followed by Stensons duct. Sialendoscopy is a technique in which we can diagnose and treat ductal pathology of salivary gland with miniature endoscope with minimally invasion. We can visualise directly and in real time makes sialendoscopy a superior tool for diagnostic purpose over conventional modalities of imaging for obstructive pathologies. Paediatric sialadenitis accounts for 10% of the salivary gland diseases in children. Acute viral sialadenitis is the most common disorder of parotid gland which affects children. But recurrent sialadenitis due to juvenile recurrent parotitis is also common cause in paediatric age group. Apart from these children may be affected with ductal stricture, mucous plug, polyps and other ductal pathology causing obstructive sialadenitis.1 these pathologies were treated medically with antimicrobials, anti-inflammatory agents and sialagogues or surgically by gland excision or duct splitting. While medical management gives temporary solution in chronic cases; surgical management has risk of complications like injury to marginal mandibular, lingual and hypoglossal in submandibular gland or parotid fistula, Frey’s syndrome and facial palsy in parotid gland.2 With introduction of sialendoscopy there is paradigm shift in management of chronic salivary disorders. while we still need to excise the gland for neoplastic lesions. Use of sialendoscopy for diagnostic and therapeutic purpose leads to avoiding surgical gland removal to gland saving procedure. The first attempt to perform sialendoscopy was by Katz and Gundlach in 1990.3 since then with better optics and instrumentation we can use it in many indications now. Contemporary ways of investigation in case of salivary lesion ranged from X- Ray, ultrasound, CT –Scan, MRI, sialography (conventional and MRI) with their own indications and pitfalls. While diagnostic sialendoscopy gives direct vision with sensitivity of 96 to 98%.4,5 sialendoscopy can be performed as a day care procedure with minimal morbidity.6 It can be performed in any age group from paediatric to geriatric and also in patients who have other co-morbidities.7 But it has its own limitations like miniature fragile endoscope, long learning curve, cost of consumables and requires lots of skill and patience.
MATERIALS AND METHODS In this study we have included cases undergoing sialendoscopy at department of ENT and Head and Neck surgery in a tertiary hospital in last year. All patient having symptoms like recurrent pain and swelling of the cheek or below the jaw specially after meal or those who have dry mouth; for more than 1 month were subjected to sialendoscopy and are included in the study with exclusion of patient diagnosed with neoplastic lesion (benign or malignant). Detailed history and clinical examination was done in all cases. We divided all patient into six group depending upon sex and age. we considered below 15 years in paediatric group and above 51 as elderly patient group while 16 -50years were counted as middle age group. All patients went for routine blood investigations and CT-scan of affected gland prior to the procedure. All sialendoscopy were done in operation theatre under general anaesthesia. All patients were given sialagogues prior to the procedure. Punctum of duct was identified with microscope in submandibular gland and directly in parotid gland. Serial dilations were done. Then diagnostic sialendoscope used first to identify the pathology. With modular or all in one scope necessary procedure were done as a therapeutic measure.
RESULTS We had twenty patients in this study after excluding patient diagnosed with acute or neoplastic disorder. Out of this 20 patient with clinical features suggesting chronic salivary lesion of non-neoplastic type; two patient had bilateral lesion so total 22 glands were subjected to sialendoscopy. Among all these 22 procedures we could identify pathology in twenty glands which were treated accordingly while two patients with normal salivary ductal system were treated conservatively and discharged. With this data we can say diagnostic sensitivity was 90.9% with sialendoscopy. (Table 1) We found equal number of male and female (11) in our study. While we have two paediatric patient with incidence rate of 9.1% having youngest patient of three years. From above 51 age group we had 5 patients with incidence rate of 22.72% and from the adult age group we had 15 patients with incidence rate of 68.18%. (Table 2) Among all patients with pathology highest number of cases were seen with parotid glad 55% followed by submandibular gland 40% and only 5% in sublingual gland. Most number of patients were diagnosed having sialolithiasis 65% followed by other pathology like foreign body, ductal perforation and xerostomia having combined incidence of 25%, while ductal stenosis and mucous plug having 5% incidence rate each. (Table 3) Table 1: diagnostic sensitivity of sialendoscopy
Table 2: age and sex wise distribution of patient subjected to sialendoscopy
Table 3: gland wise distribution of chronic non neoplastic salivary disease
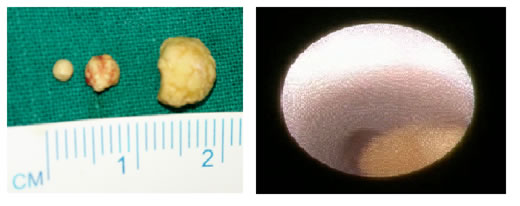
Figure 1: Sialolithiasis from parotid gland, Figure 2: Foreign body seen on sialendoscopy DISCUSSION Chronic salivary non neoplastic lesions were conventionally diagnosed by range of radiological technique like x-ray, sonography and sialography. These methods give indirect evidence of the pathology. According to marshal et al. stones smaller than 3 mm may not produce any acoustic shadow and may be missed on sonography8. In the study of Deenadayal et al. they found that USG had a good sensitivity of 95.6% for detecting calculi but a poor sensitivity of 17.8% for detecting non-calculus cause of obstruction like strictures and mucus plugs. In the same study they found diagnostic sensitivity of 93% with sialendoscopy.9 while in our study we found out diagnostic sensitivity of 90.9% with sialendoscopy which is almost similar to study by Deenadayal et al. In our study we found out that there is equal distribution between male and female so there is no sex predominance in case of chronic non neoplastic salivary lesions. And we also noticed that most of the cases in our study were from middle age group 68.18% followed by elderly group with 22.72%. least incidence was found in paediatric age group 9.1%. Nahlieli and Baruchin found 73% pathology in submandibular gland and 27% pathology in parotid gland and only one case of sublingual gland.1 In contrast to their observation we found maximum cases with parotid gland(55%) followed by submandibular gland (40%) and only one case of sublingual gland (5%) involvement.In all our cases with chronic ductal pathology we found maximum patient were suffering from sialolithiasis (65%), ductal stenosis (5%), mucous plug (5%). And one fourth of the cases were of miscellaneous group with xerostomia, ductal fistula, foreign body. While in ngu et al. they had incidence rate of sialolithiasis (73.2%), ductal stenosis (22.6%) and mucous plug (4.2%).10 In comparison with our study we found incidence of sialolithiasis and mucous plug same as their study while incidence of ductal stenosis was considerably lower in our study. Sialendoscopy for chronic non neoplastic lesion were performed in all patients with good outcome and thus we could avoid any surgical gland excision procedure in all our 20 patients. In conventional treatment protocol before sialendoscopy all these patients would have been subjected to gland removal so we can say with advent of sialendoscopy we could save the respective gland in all cases of our study. In study of Deenadayal et al. they had gland preservation rate of 93%9 while 95-98% gland preservation rate was seen in study of Iro, H. et al..11
CONCLUSION In comparison of conventional diagnostic methods for chronic non neoplastic salivary lesions sialendoscopy offers better diagnostic outcome specially far superior in case of non-calculus ductal pathologies. Sialendoscopy also allows us to manage the pathology at the same time of diagnostic procedure. Most of the cases of ductal pathologies are sialolithiasis for which sialendoscopy offers diagnostic as well as therapeutic management at the same time. We can avoid conventional gland excision and save the gland as well as prevent potential complication of gland excision with sialendoscopy with good outcome in ductal pathologies.
REFERENCES
|
|
 Home
Home