Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 3 - March 2019
A cross sectional study of neutrophil to lymphocyte ratio (NLR) in patients with benign paroxysmal positional vertigo
Venkata Kasyapi V1, ThirunavukarasuPalanisamy2, Priya Kanagamuthu3*, Rajasekaran S4, Paventhan K5, Prabakaran S5, Namasivaya Navin RB6, Balaji D7, Ramyashree C7
1,7Junior Resident, 2Professor, 3Associate Professor, 4Professor and HOD, 5Assistant Professor, 6Senior Resident, Department of Otorhinolaryngology, Chettinad Hospital and Research Institute, Rajiv Gandhi Salai, Kelambakkam, Kanchipuram, Tamil Nadu – 603103, INDIA. Email: catchpriya.29@gmail.com
Abstract Benign Paroxysmal Positional Vertigo (BPPV) is a specific subtype of peripheral vertigo with recurrences and significant impact on quality of life. Neutrophil – Lymphocyte Ratio (NLR) is an easily measured, reproducible marker increasingly recognized worldwide in various inflammatory conditions. We aimed to evaluate NLR in patients with BPPV and to ascertain the sociodemographic parameters associated with altered NLR. In the study conducted at department of Otorhinolaryngology, Chettinad Hospital and Research Institute, a total of 60 patients (20 males and 40 females) with BPPV were recruited. NLR was calculated from all subjects. The mean absolute neutrophil and lymphocyte counts were 4742.08 ± 1853.7, 1767.06 ± 821.4 respectively and the median (Inter Quartile Range) of NLR was 2.3 (1.5,4.2). A positive correlation was seen for NLR with age (spearman’s Rho .353, p<0.001). In conclusion, this was the first study to evaluate NLR in BPPV where we found a higher NLR in patients with BPPV. We thus hypothesize the role of inflammation in BPPV in our population. Key Word: BPPV, inflammation, lymphocyte, neutrophil, NLR.
INTRODUCTION Vertigo is the sensation of perceived movement of either self or of the surrounding objects. It can be central or peripheral in origin. Common peripheral causes include: Meniere’s disease, BPPV, Labyrinthitis and Vestibular neuritis1. Positional vertigo is described as a sensation of spinning which is produced by changes in head position with respect to gravity. Benign Paroxysmal Positional Vertigo (BPPV) is a type of positional vertigo. Approximately 85-95% of BPPV is due to posterior semicircular canal involvement followed by horizontal semicircular canal2. History and clinical examination form the cornerstone of diagnosis. Overall, the prevalence of BPPV has been reported to range from 10.7 to 64 per 100,000 population with a lifetime prevalence of 2.4 percent3. Added to the heterogeneity of risk factors causing BPPV, the problem is compounded by the remissions and recurrences of the disease condition. With a recurrence rate of 15%4. This condition has a significant impact on the quality and productivity of life as well. Vertigo and stress are co-existent with production of increased levels of stress hormones during attacks of vertigo. The level of anxiety following an attack of vertigo also might be increased. The resultant anxiety provokes various symptoms, probably through disorders of the autonomic nervous system, influenced by the increased levels of stress-related hormones and inflammatory markers5. Most commonly used markers of inflammation are white blood cell (WBC) count, ESR, C-reactive protein (CRP). Neutrophil-to-Lymphocyte ratio (NLR) is a simple parameter to assess easily the inflammatory status of subject. NLR has been proposed as a reliable indicator of host inflammatory status and potential marker of inflammation in cardiac and non-cardiac disorders6.NLR is an easily measured, reproducible marker of inflammation. In patients with breast carcinoma, NLR was shown to have the potential to predict poor prognosis7. NLR along with Monocyte-to-Lymphocyte ratio (MLR) has also been shown to have a clinical significance in diagnosing SLE thus paving way for importance of NLR in autoimmune diseases8 This study was performed to evaluate the Neutrophil Lymphocyte Ratio (NLR) in patients with BPPV and to ascertain the sociodemographic parameters associated with altered NLR, if any. NLR as an inflammatory marker could identify role of anti-inflammatory drugs in management of BPPV.
MATERIALS AND METHODS This study was a hospital-based cross-sectional study and was conducted in the Department of Otorhinolaryngology at Chettinad Hospital and Research Institute, Kelambakkam, Chennai. Sample size was calculated using the following formula: -; prevalence of BPPV was taken as 23.9% (Moreira M D et al., 2014)9. The final calculated sample size was 59.87 and a total of 60 BPPV subjectswere recruited by convenient sampling. The data collection was done between December 2018 to January 2019 for a period of three months. Patients diagnosed with BPPV satisfying the following criteria were included: A) Recurrent attacks of positional vertigo provoked by lying down or turning over in supine position, B) Duration of attacks less than 1 minute, C) Positional nystagmus elicited after a latency of few seconds by Dix-Hallpike maneuver. D) Does not attribute to any other disorder. Patients with other causes of peripheral and central vertigo were excluded. Patients with systemic diseases (DM, HT, etc) known to affect NLR were also excluded. After obtaining informed written consent, all the relevant parameters were documented in a structured study proforma. Blood samples were drawn by venipuncture from the antecubital vein and assessed for hemogram and calculation of the Neutrophil- Lymphocyte Ratio. Statistical analysis was performed using SPSS version 22. Normality of the continuous data was checked using K.S test. The continuous variables were described as mean ± standard deviation. The categorical variables were presented in terms of their frequencies and proportions. For comparison of means between the groups, independent t-test was used. For comparison of ratios, Mann-Whitney U test was used.
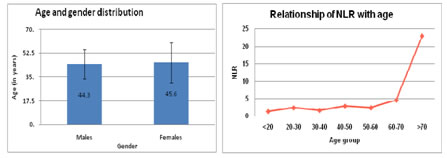
OBSERVATION AND RESULTS A total of 60 patients diagnosed with BPPV were included in the study. Study subjects included 40 females (66.7%) and 20 males (33.3%) (M: F = 1:2). The mean age was 45.1 ± 13.7 years with youngest being 17 years and oldest 76 years old. The age groups wise distribution of subjects is shown in Table 1. The mean age was similar among males (44.3 years) and females (45.6 years) and there was no significant difference between the two. (Figure 1) The mean absolute neutrophil and lymphocyte counts were 4742.08 ± 1853.7, 1767.06 ± 821.4 respectively and the median (Inter Quartile Range) of NLR was 2.3 (1.5, 4. 2). There was no significant difference in NLR between males and females as shown in table 2. There was a positive correlation obtained for NLR with age, Spearman's rho of .353 and p-value <.001 and the distribution of NLR within different age categories is shown in figure 2. Table 1: Age categorization of BPPV patients
Table 2: Distribution of inflammatory parameters between the genders
Independent t-test used; a- denotes Mann Whitney U test used and median with inter-quartile range is described; p-value <0.05 is significant;
Figure 1 Figure 2 DISCUSSION BPPV has a worldwide prevalence of 10.7 to 64.0 cases per lakh persons10. Studies have shown that BPPV has a higher potential to affect women and older adults and peaks around fifth and sixth decades10,11. In addition, the female to male ratio would be 2:1 which simulated the results of our study. In a Turkish study12 the average age of the enrolled participants were 39.1± 12.4 years and our study subjects were slightly elder with the mean age of 45.1 ± 13.7 years. It has been reported that the median duration of an episode of BPPV is around 2 weeks as per the study by Von Brevern M et al10. They also found these patients to have significant positive association with hypertension, dyslipidemia and stroke. Our study excluded patients with coexisting metabolic illness such as Diabetes, hypertension and dyslipidemia. This study was the first to investigate NLR exclusively in BPPV patients. Role of NLR as a biomarker in inflammatory conditions such as autoimmune diseases, Diabetes and malignancies has been evaluated before. However, underlying inflammation during an acute attack of BPPV has not been previously evaluated. According to Sahin C et al.13 the NLR in patients of peripheral vertigo was elevated during admissions and it declined at the time of discharge. The mean NLR baseline in healthy adults in China was 1.5 ± 0.0514 and a study from Chennai, India reported NLR of 1.5 ± 0.41 among healthy non diabetic individuals15. The median absolute neutrophil and absolute lymphocyte counts were 4742.08 ± 1853.7, 1767.06 ± 821.4 respectively, and the median (Inter Quartile Range) of NLR was 2.3 (1.5,4.2). Thus, this could possibly explain an underlying inflammation in patients with BPPV in our study population. Intense research is very much needed with comparison to control groups in order to derive evidences for the exact link of BPPV with elevated NLR. Large scale studies disclosing the role of ESR, Mean Platelet Volume, Platelet-Lymphocyte Ratio, Monocyte-HDL Ratio or CRP and comparing with NLR in BPPV has to be carried out as these economical parameters could be used at resource limited settings in order to provide a better quality of care for the patients.
CONCLUSION NLR is an economical, widely available, and quick investigation. Its role in various inflammatory and non-inflammatory diseases is being increasingly recognized worldwide. Our study was the first to assess the NLR in patients with BPPV as a specific subtype of peripheral vertigo. We found a positive correlation with age and the median NLR was raised in patients with BPPV. Further detailed follow up studies where NLR in BPPV is calculated before and after an attack is warranted. Also, studies evaluating the role of anti-inflammatory medications as a possible adjuvant treatment option for BPPV needs to be considered.
ACKNOWLEDGMENT The authors do not declare any funding or conflicts of interest.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home