|
Table of Content - Volume 13 Issue 3 - March 2020
Prognostic significance of liver function tests and platelet indices in predicting maternal and fetal outcomes in pregnancy induced hypertension cases
Nidya K1*, Vidya Ramdas Tirankar2
1,2Department of Obstetrics and Gynecology, Dr.Vaishampayan Memorial Government Medical College and Shri Chatrapati Shivaji Maharaj Sarvopchar, Rugnalay, Solapur, Maharashtra, INDIA.
Abstract Background: Hypertensive disorders of pregnancy remain the most common medical complication leading to adverse maternal and fetal outcome. Many women with severe pre-eclampsia may have laboratory abnormalities such as isolated thrombocytopenia or elevated liver enzymes. Aim: To evaluate the platelets and liver function tests in preeclampsia cases and their correlation as prognostic indicators with feto-maternal outcome. Material and Methods: A total of 400 patients in labor room and ANC ward with pregnancy induced hypertension were investigated for platelet count and liver function tests. The cases were followed up for maternal and perinatal outcome. Results: 39 patients with inadequate platelets had abruptio placentae, 38 patients had eclampsia, 48 had oligohydramnios, 30 patients had postpartum hemorrhage and 14 patients had HELLP syndrome. 36 out of 45 patients with deranged liver enzymes had abruption, 34 out of 54 patients with deranged liver enzymes had oligohydramnios. 31 of 35 eclampsia patients had deranged liver enzymes. 20 of 26 postpartum hemorrhage patients had deranged liver enzymes. 14 of 14 HELLP syndrome patients had deranged liver enzymes. 25.38% patients with inadequate platelets had babies with fetal distress, 29.23% with inadequate platelets had babies which were admitted to the neonatal ICU. 18.75% patients with deranged liver enzymes had babies with fetal distress. 32.14% patients with deranged liver enzymes had babies admitted to NICU. Conclusion: Thrombocytopenia is reported frequently in severe preeclampsia. There is progressive fall of mean platelet count with the increasing severity of disease. Detection of increased LFTs in cases of severe preeclampsia is a risk category, associated with increased rate of feto-maternal complications. Key Words: pregnancy induced hypertension, thrombocytopenia, liver function tests, maternal outcome, fetal outcome
INTRODUCTION Hypertensive disorders of pregnancy remain the most common medical complication leading to a majority of adverse perinatal and maternal outcome.1 Many women with severe pre-eclampsia may have laboratory abnormalities such as isolated thrombocytopenia or elevated liver enzymes without complete HELLP syndrome. Abnormal liver function tests occur in 20-30% of pregnancies complicated by pre-eclampsia and are associated with poor maternal and fetal outcome. Maternal mortality associated with HELLP syndrome ranges from 1.1%-24.2%.2 Prevention of any disease process requires the availability of methods for prediction of those at high risk for the disorder. Although numerous clinical and biochemical tests have been proposed for prediction for early detection of pre-eclampsia, most remain unrealistic for general use in most developing countries. At present, there is not a single reliable and cost effective screening test for pre-eclampsia which can be recommended for use in most developing countries. Timely intervention along with knowledge and detection of the various complicating factors would go a long way in improving feto-maternal outcome in these disorders. Hence, this clinical study was conducted to evaluate the platelets and liver function tests in preeclampsia cases and their correlation as prognostic indicators with feto-maternal outcome.
MATERIAL AND METHODS This prospective observational study was conducted in the Department of Obstetrics and Gynaecology with assistance from Department of Biochemistry and Pathology of Tertiary Care Hospital. All patients in labor room and ANC ward with pregnancy induced hypertension were investigated from a period of two years. Written approval from ethical committee, at the institute level was obtained. This clinical study was conducted in defined cases of PIH admitted at our institute (tertiary care center), in Department of Obstetrics and Gynecology, above 28 weeks of gestation (third trimester). Definition of case Antenatal cases in third trimester clinically diagnosed to have PIH with BP> 140/90mm Hg on two separate occasions more than 6 hours apart with/without bilateral pedal edema and proteinuria. Inclusion criteria
Exclusion Criteria
Methodology Detailed history taking and general, systemic and obstetrical examination was carried out. All enrolled patients were classified into mild and severe pre-eclampsia, gestational hypertension based on ACOG guidelines. Specific investigations were performed, fundus examination was also done. Hemoglobin and Platelet counts was done by using of automated haematology analyser. Liver function tests were done with automated analyzer available in our hospital. All patients in the study were monitored in the ward using intensive non-invasive methods. Blood pressure, urine albumin, fetal movement count were recorded daily till the period of delivery. Weekly monitoring of abdominal circumference, symphysio-fundal height, complete blood count, liver function tests and renal function tests, fundoscopy and ultrasonography were performed as a routine for all patients. Statistical analysis The collected data was analyzed with IBM.SPSS statistics software 23.0 Version. To describe about the data descriptive statistics frequency analysis, percentage analysis were used for categorical variables and the mean and S.D were used for continuous variables. P value <0.05 was considered significant, P ≤ .01 was considered highly significant.
RESULTS Out of the 400 patients, 56.25% of the patients were in 21-25 years age group, 20% patients were in 18-20 years age group, with 19% in 26-30 years age group and 4.75% in 31-35years age group. It was observed that as the age increased, the number of pre-eclamptic patients decreased. The mean age group of the patients was 23. Maximum of 49.25% being nulliparas, 23.25% patients were primiparas and 20.75% were belonging to second para, 6.75% being multipara. 47% patients belonged to mild pre-eclamptic group and 45.75% were severe pre-eclamptic. A very small group of 7.25% patients belonged to gestational hypertension group. In our study, 30.75% belonged to 37-38 weeks of gestation and 28.25% belonged to 35-37weeks of gestation.26.25% were referred after 38 weeks. 8.5% patients belonged to 32-34 weeks of gestation. 6.25% were in 28-31 weeks gestational age. 61.75% patients had vaginal delivery, out of which 48.2% were induced. Induction was done with Foley’s catheter no.24 or prostaglandin E2 gel depending on the Bishop’s score. 6 patients had instrumental delivery. Main indication of induction in 56% patients were abruption placentae followed by oligohydramnios in 40%. Main indication for cesarean section was fetal distress in 57% patients. In present study, 35% of patients had inadequate platelets with 80% count being the lower limit (80,000). 65% patients had normal platelet counts. 39% patients had with platelets in the range of 1,00,000-1,50,000. 24.25% patients had platelets counts in the range of 1,50,000-2,00,000.21.5% had platelets in the range of less than 1,00,000.15.25% had platelets more than 2,00,000. It was observed that 6.5% had deranged bilirubin. 19 of them landed in HELLP syndrome and DIC. 93.5% were having normal values. Among the 26 patients with deranged bilirubin 16 had higher direct bilirubin and 10 had higher indirect bilirubin. According to the normal values of SGOT/SGPT in the third trimester and comparison with contemporary studies cutoff was set as 70/70. 31% had deranged SGOT/SGPT.
Table 1: Maternal complications with platelet correlation
In present study, 39 patients with inadequate platelets had abruptio placentae, 38 patients had eclampsia, 48 had oligohydramnios, 30 patients had postpartum hemorrhage and 14 patients had HELLP syndrome.
Table 2: Maternal complications correlation with liver function tests
In our study, 36 out of 45 patients with deranged liver enzymes had abruption, 34 out of 54 patients with deranged liver enzymes had oligohydramnios. 31 of 35 eclampsia patients had deranged liver enzymes. 20 of 26 postpartum hemorrhage patients had deranged liver enzymes. 14 of 14 HELLP syndrome patients had deranged liver enzymes. 35.5% babies were of 2-2.5kg, 34.5% were more than 2.5kg. Low birth weight babies were 30%,6% being extremely low birth weight babies. 20.5% babies had fetal distress detected by CTG or Hand held Doppler. 21.5% Babies were admitted to NICU, out of which 54% were admitted due to low birth weight and extremely low birth weights. 12% cases where IUD in the study, out of which 67% were abruption cases. There were 3.75% stillbirths in the study. 41.5% babies were IUGR.
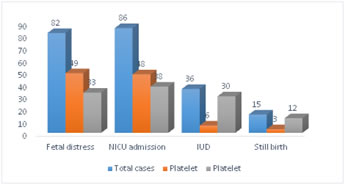 Figure 1: Fetal outcome with platelet counts correlation Thirty-three (25.38%) patients with inadequate platelets had babies with fetal distress, 18.15% with adequate platelets had babies with fetal distress. Comparison between Fetal distress and Platelet has no statistical significance (Chi-Square value= .007, p-value= 0.934) with P >.050. Thirty-eight (29.23%) with inadequate platelets had babies which were admitted to the neonatal ICU.17.78% with adequate platelets had babies admitted to NICU. Comparison between NICU admission and Platelet has no statistical significance (Chi-Square value= .964, p-value= 0.326) with P >.050. Thirty (23.08%) patients with an inadequate platelet count had intrauterine death.2.22% with adequate platelets had an IUD. Comparison between IUD and Platelet has high statistical significance (Chi-Square value= 52.513, p-value= 0.0005) with P ≤ .01. Twelve (9.23%) patients with inadequate platelets had a stillbirth and 1.11% patient with adequate platelets had a stillbirth. Comparison between Still birth and Platelet has high statistical significance (Chi-Square value= 18.129, p-value= 0.0005) with P ≤ .01.
Figure 2: Baby weight with platelet correlation In our study, 32 (24.06%) patients of thrombocytopenia had baby weight in the range of 1-1.5kg, 21.80% had baby weight in the range of 2-2.5kg, 21.05% patients had baby weight in the range of 1.5-2kg. 18.81% had baby weight more than 2.5kg. 14.28% patients had baby weight less than 1kg.
Figure 3: Fetal outcome with liver function tests correlation
Twenty-one (18.75%) patients with deranged liver enzymes had babies with fetal distress.17.71% patients with normal liver enzymes had fetal distress babies. Comparison between Fetal distress and SGOT/SGPT has no statistical significance (Chi-Square value= .084, p-value= 0.772) with P >.050. Thirty-six (32.14%) patients with deranged liver enzymes had babies admitted to NICU.17.36% of the patients with normal liver enzymes had their babies admitted to NICU. Comparison between NICU admission and SGOT/SGPT has no statistical significance (Chi-Square value= .212, p-value= 0.145) with P >.050. Twenty-two (19.64%) patients with deranged liver enzymes had an IUD. 4.86% patients with normal liver enzymes had an IUD. Comparison between IUD and SGOT/SGPT has high statistical significance (Chi-Square value= 25.903, p-value= 0.0005) with P ≤ .01. Ten (8.93%) patients with deranged liver enzymes had a still birth.1.74% with normal liver enzymes had a still birth. Comparison between Still birth and SGOT/SGPT has high statistical significance (Chi-Square value= 13.639, p-value= 0.0005) with P ≤ .01.
Figure 4: Baby weight correlation with liver function tests In our study, 32.37% patients of Deranged LFTs had baby weight in the range of 1.5-2kg, 21.58% had baby weight in the range of 1-1.5kg, 19,42% patients had baby weight in the range of 2-2.5kg. 18% had baby weight more than 2.5kg. 8.63% patients had baby weight less than 1kg.DISCUSSION The patients in this study were a well-defined group with diagnosed hypertensive disorder of pregnancy. All patients had been accurately randomized using the inclusion and exclusion criteria. Complete haemogram including platelet count had been done and documented. The cases had been followed up for maternal and perinatal outcome. Out of 400 cases of hypertensive disorders of pregnancy, 130 cases had documented thrombocytopenia which accounts for 33.51% and 115 cases had deranged LFTs which accounts for 29.64%. There had been no statistically significant association between the severities of pregnancy induced hypertension and thrombocytopenia. But a higher incidence of cesarean section was observed with increasing gestational age, probably because of better fetal outcome and fetal survivability. There was a high statistically significant association between maternal outcome and thrombocytopenia but in cases with severe thrombocytopenia, there was an increase incidence of maternal morbidity due to abruption placenta, DIC, renal failure, eclampsia and pulmonary oedema. There were 19 cases of maternal mortality due to uncontrolled post-partum haemorrhage, eclampsia and abruption placenta leading to DIC, Acute renal failure. The perinatal outcome mainly depended upon the gestational age at the time of delivery. Better fetal outcomes were reported with increasing gestational age.3-5 Comparison between Mode of delivery with Thrombocytopenia and LFT’s deranged shows high statistical significance (Chi-Square value= 27.62, p-value= 0.0005) with P≤.01 Comparison between severity of Hypertension with Thrombocytopenia and LFT’s deranged shows no statistical significance (Chi-Square value= 29582, p- value= 0.228) with P>.05. TICU admission and Platelet counts had high statistical significance (Chi-Square value= 64.127, p-value= 0.0005) with P≤.01. Between Blood and Blood product transfusion and Platelet had high statistical significance (Chi-Square value= 60.674, p-value= 0.0005) with P≤.01. Comparison between maternal Death and Platelet has high statistical significance (Chi- Square value= 20.989, p-value= 0.0005) with P≤.0120.3% had oligohydramnios in the thrombocytopenia group and the next most common being abruption, eclampsia. The mean platelet count values in our study were: control 2.38±0.39 lakh/mm3, Mild Pre-eclampsia-2.3±0.43 lakh/mm3, Severe pre-eclampsia-1.6±0.42 lakh/mm3. The mean platelet count of cases as a whole was 1.87±0.59 lakh/mm3. It was seen that the platelet count in severe preeclampsia and cases with eclampsia were very significantly lower than the healthy pregnant women, whereas the platelet count in mild preeclampsia was not significantly lower than the healthy pregnant women. Jambhulkar et al6 also found normal platelet count in mild preeclampsia when compared with normal pregnant control group but in severe pre-eclampsia (1.70±0.57 lakh/mm3) and eclampsia (1.51±0.56 lakh/mm3) decrease in platelet count was highly significant.7In present study, we observed that as the severity of PIH increases from mild preeclampsia to severe preeclampsia and eclampsia a decreasing trend of platelet count is seen and the association is statistically significant. Similar association was shown by Poulri et al.8,9 Thrombocytopenia was present in 5 out of the 100 PIH cases and in which 4 were eclampsia patients and only one was that of severe pre-eclampsia. Therefore, thrombocytopenia was mostly a feature of eclampsia. In preeclampsia case the lowest platelet count was 90,000 cells/mm3 and in eclampsia the lowest platelet counts recorded was 51,000 cells/mm3. In present study, the rate of maternal complications and fetal complications during pregnancy increased as the severity of PIH increased. The complication rate was seen to be higher in the cases of severe preeclampsia. We observed that cases with low platelet counts had increased risk of maternal and fetal complications. Most of the PIH cases who developed Preterm labour, impending eclampsia and placental abruption had platelet count in the range of 1 to 1.5 lakh/mm3. Out of 130 PIH cases who presented with thrombocytopenia, 6 women had pulmonary odema, 16 had placental abruption, 1 had DIC and 14 maternal deaths occurred. Most of the fetal complications were also seen in cases with platelet count in the range of 1-1.5 lakh/mm3. In all of the 5 women who developed less than 1 lakh thrombocytopenia intrauterine fetal demise was seen. Among patients who had deranged liver enzymes 41.08% of patients in the age group of 26-30years age group. 25.89% belonged to 21-25 years age group. 41.96% patients were second para,30.36% were nulliparous. Comparison between Gestational age with SGOT/SGPT showed high statistical significance (Chi-Square value= 85.991, p-value= 0.0005) with P ≤ .01. Comparison between Diastolic blood pressure with SGOT/SGPT and Serum bilirubin shows no statistical significance (Chi-Square value=4.25, p- value=0.119 with P>.05. TICU admission and SGOT/SGPT had high statistical significance. Blood and Blood product transfusion and SGOT/SGPT has high statistical significance. Maternal Death and SGOT/SGPT has high statistical significance (Chi-Square value= 11.261, p-value= 0.001) with P≤.01. Severity of hypertension and SGOT/SGPT has high statistical significance. Maternal complications with deranged LFTs-23% patients had oigohydramnios and 16% had abruptio placentae. Fetal distress and NICU admissions with thrombocytopenia and deranged LFTs had no statistical significance. 26.32% patients of thrombocytopenia had baby weight in the range of 1.5-2kg, 24.06% had baby weight in the range of 1-1.5kg, 21.80% patients had baby weight in the range of 2-2.5kg. 18.8% had baby weight more than 2.5kg. 9.02% patients had baby weight less than 1kg. 32.37% patients of Deranged LFTs had baby weight in the range of 1.5-2kg, 21.58% had baby weight in the range of 1-1.5kg, 19,42% patients had baby weight in the range of 2-2.5kg. 18% had baby weight more than 2.5kg. 8.63% patients had baby weight less than 1kg. High statistical significance was observed in still births and intrauterine deaths with thrombocytopenia and deranged LFTs.CONCLUSION Thrombocytopenia is reported frequently in severe preeclampsia. There is progressive fall of mean platelet count with the increasing severity of disease. Detection of increased LFTs in cases of severe preeclampsia is a risk category, associated with increased rate of feto-maternal complications, compared to severe pre-eclampsia with normal LFTs. Such cases need special attention with early detection and referral to higher centre with better facilities of NICU set up to reduce the complications and mortality.REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home
