|
Table of Content Volume 13 Issue 3 - March 2020
Neurological manifestations in snake bite poisoning
Mirza Hammad Ali Baig1*, Mohd Asif Hussain2
1Assistant Professor, 2Senior Resident, Department of General Medicine, ESIC Medical College, Gulbarga, Sedam Road 585106, INDIA. Email: drhammadbbaig@gmail.com
Abstract Background: Snake bite is a life-threatening injury. Snake bite requires intensive care unit admission. Different snakes are observed in India. Snake bite manifest as neurological manifestation, haematological manifestation and local manifestations depending on type of snake. Aim and objective: To study the neurological manifestations in snake bite poisoning Material and methods: Present study was a prospective study carried out in Al Ameen Medical College Hospital, Bijapur on patients with snake bite. Data collected was sociodemographic data, type of snake, bite details, physical examination, progress of snake bite and outcome. Data analysed with appropriate statistical tests. Results and discussion: The incidence rate of Neurological manifestations in this study is 38.88% In our study we observed most common neurological manifestation was ptosis (85.7%) followed by Ophthalmoplegia (42.8%) respiratory failure (38.8%), facial palsy{19%}, hemiplegia/paraplegia (9.5%) and coma (9.5%). Key Word: snake bite.
INTRODUCTION The very existence of man depends to tally on the inter-relationships of other living beings and the maintenance of that complex and delicate balance, so it is our own interest to explore this parallel world -' a world where fact often reads like fantasy'. There are many single species of reptiles alone which far outnumber man in their worldwide distribution. Snakes are the most researched reptiles. The essence of the fascination and the fear of snakes have lain in their venom. In the past, the consequences of bite by venomous snakes were often attributed to forces' beyond nature, sometimes to revengeful deities thought to be embodied in the serpents. The venomous and poisonous animals are widely distributed throughout the animal kingdom. Of the 2,500-3,000 species of snakes, approximately 375 are considered to be venomous. The poisonous varieties belong to five families:
In the Indian sub-continent most of the deaths are attributed to, bites from snakes of the Elapidae family (Cobra and Krait) though bites from snakes of the Viperidae family are also common1. Snake-bite is common among the working group. It is estimated that about 70% of total cases of snake-bite are recorded in the 11-50 years age group. Males are affected three times more often than females2. The highest incidence of snake-bite occurs at the beginning of the rainy season when the reptiles are forced to come out of their pits and hideouts due to floods. Snake-bite is frequent in those engaged in outdoor activities. Bites seldom occur in the night when people sleep. Snakes bite only as a defence phenomenon. Two-third of bites are found on the legs and the feet and one-third on the fingers and hands, these areas come into contact with snakes during locomotion or during work. In India Joseph Fayrer was one of the pioneer workers to elaborate on the action of snake venom on the neurological system. Research work with cobra and krait venoms in dogs and cats has confirmed that the respiratory centre is active when respiration ceases and curarisation of the diaphragm is complete. 3-5 It was also proved that life could be prolonged by artificial respiration and maintenance of vital functions in a curarised and in an envenomated animal. Although no definite statistics are available, it is surmised that only a quarter of all bites are by poisonous snakes in our country and the rest of the bites are probably by the non-poisonous variety. This conclusion has been drawn on the basis of the symptoms in hospitalized patients. Banarjee and Siddique state that cobra-bites are more common than viper-bites in India. The studies conducted by different workers (Misra et al. 1982) state that the conventional treatment with antivenom resulted in mortality as high as 50-57% among all those who developed the symptoms of envenomation. This high mortality despite the available methods of treatment was responsible for the mortal fear of snake-bite that exists in the minds of the people2. Antivenins differ greatly in their potency . when the species of the snake is known a specific monovalent, high titer antivenom is the best treatment. Otherwise a polyvalent antivenin may be used, sometimes a heterologous monovalent antivenin can be of value 6 . Antivenin can be of proven potency have been shown in clinical trials to be of value in preventing and reversing some of the serious effects of snake bite 7,8 Not Many studies have been conducted on the neurological manifestations of Snake envenomation in Karnataka. This study takes into account the manifold action of snake venoms on the human being, special importance being given to the neurological manifestations.
MATERIAL AND METHODS Present study was a prospective study carried out in Al Ameen Medical College Hospital, Bijapur and District Hospital Bijapur during the period from January 2013 to December 2013. Study population was patients visiting casualty department with snake bite. Inclusion Criteria: All patients with history of snakebite and with at least one of the following criteria were included in the study 1.Patients or attenders have seen the offending snake. 2.Definite fang marks are noted. 3. Features of local or systemic envenomation. Exclusion Criteria: Patients with history of suspected snakebite where in 1. Patient or attenders have not seen the snake. 2. No fang marks and no features of envenomation. Patients with pre-existing neurological problems, renal problems and bleeding diathesis. Any patient brought to the Al Ameen medical college hospital and district hospital, Bijapur with a history of snake bite was observed for signs of envenomation. They were carefully observed till it was definite that there was no reaction or features of systemic poisoning. The patients who showed either features of local or systemic envenomation were admitted to the intensive care unit. A proforma was prepared to enter the case notes and the progress of the patients. A detailed physical examination was made at the time of admission to assess the type and severity of systemic involvement. Every effort was made to identify the snake if it was brought by the patient's attenders. From the clinical presentation, it was possible to identify the type of envenomation, whether neurotoxic or haematotoxic. The bite site is inspected. The number and type of fang marks are noted and the type of local reaction is described. The vital signs of the patient are assessed. A detailed assessment of the neurological system is made with observation for the presence of ptosis, diplopia, slurring of speech, dysphagia or respiratory insufficiency. All patients were treated with medical management in the form of antibiotics and analgesics. Patient with definite features of envenomation were given the polyvalent ASV and tetanus prophylaxis. Patients who developed cranial nerve palsies especially of the 9th and 10th cranial nerves were given pharyngeal and laryngeal toilette through a cuffed endotracheal tube and respiratory paralysis was anticipated. All other systemic manifestations were treated. Patients were followed till their discharge or death. Data was analysed with appropriate statistical tests.
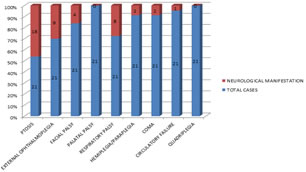
RESULTS A total of 70 cases of snakebite cases were studied out of which 4 were doubtful snakebite cases. These 4 cases were not included in the Study. 12 bites were non poisonous. 54 bites were poisonous. Following Observations are with reference to these 54 poisonous snake bite patients. In the present study in 22(40.7%) patients biting snake’s species could not be identified. In 7(13%) patients the biting species was Cobra, in 10(18.5%) it was Krait and in 15(27.8%) it was Viper. (table1) Out of the 54 patients 21(38.9%) were in the age group of 31-40 years, 12(22.2%) were in the age group of 21-30 years. 9(16.7%) were in the age group of 41-50 years, 7(13%) were in the age group of 11-20 years and 2(3.7%) in the age group of 51-60 years. There was 1(1.8%) patient each in the age group of 0-10, 61-70 and 71-80 years. (table 2) In our study male preponderance was seen with Male to female ratio of 2.9:1. In our study 31.5% were admitted after 24 hours and 68.5% before 24 hours. A number of patients seek treatment from traditional healers before getting admitted to hospitals. In the present study, 18(33.3%) patients sought treatment from traditional healers first and later got admitted to hospital. In the present study 50(92.6%) patients had pain at the site of the bite, 48(88.9%) had swelling at the site of the bite. 19(35.2%) patients had vomiting. Bleeding manifestations were seen in 11(20.4%) patients. Abdominal pain was present in 5(9.2%) Oliguria and Anuria were present in 4(7.4%) patients. Inability to open eyes and or difficulty in swallowing difficulty in respiration and weakness of limbs were present in 21(38.9%) patients. (table4) In the present study 21(38.9%) patients had neuroparalytic features, 11(20.4%) patients had haematotoxic features, 1(1.8%) had both. In our study 18 (33.3%) patients had local manifestations only. Incidence rate = (No. of new cases/No. of population at risk)×100 Incidence rate of neurological manifestations=( No. of cases with neurological manifestations/Total no. of snakebite cases)× 100 Total no. of cases = 54 No. of cases with neurological manifestations = 21 Incidence rate=(21/54)×100= 38.88% Hence the incidence rate of Neurological manifestations in this study is 38.88% In our study we observed most common neurological manifestation was ptosis (85.7%) followed by Ophthalmoplegia (42.8%) respiratory failure (38.8%), facial palsy{19%}, hemiplegia/paraplegia (9.5%) and coma (9.5%) . Whereas no convulsions, palatal palsy, quadriplegia was seen in any case in this study.(fig 1 ) In the present study 6(11.1%) patients died. Two were cobra bites 2 were viper bites. 1 was Krait bite and 1 unknown. The cause of death in three patients was AKI and in the other 3 respiratory failure. In the present study 18(85.8%) out of 21 neurotoxic bites received both neostigmine and A.S.V. One (4.5%) patient was given only neostigmine and no A.S.V .3(13.6%) patients did not receive neostigmine because of non availability. One patient who did not receive neostigmine died of sudden respiratory failure. This patient could not be but on ventilator support. Three patients who received both neostigmine and A.S.V died.
Table 1: Distribution of cases according to bite of species
Table 2: Distribution of snake bite poisonous cases according to age group
Table 3: Distribution of snake bite poisonous cases according to site of bite
Table 4: Showing frequency of various symptoms in the 54 cases
Figure 1: distribution of cases according to neurological manifestations in snake bite
DISCUSSION In our study maximum patients 21 (38.9%) were from the age group of 31-40 years followed by 21-30 years 12(22.2%). Similar findings were seen in Nigam et al9 and, Hatti et al10 In the present study 40(74.1%) were males and 14(25.9%) females. The male to female ratio was 2.9:1 This is similar with the findings of Nigam et al9 and Bhat et al.11, However the ratio was 1.2:1 according to Hati et al.10 In the present study in 22(40.7%) patients biting snake’s species could not be identified. In 7(13%) patients the biting species was Cobra, in 10(18.5%) it was Krait and in 15(27.8%) it was Viper. Similar findings were observed in Sarangi et al. 12 where Viper bites were observed in 85.2 % patients. Nigam et al9 found that 63.3% patients were of Viper bite while 36% were of Cobra bite. In our study, 31.5% were admitted after 24 hours and 68.5% before 24 hours. These findings are consistent with the study of Bhat 11who reported that 72% of patients were admitted within 24 hours and 28 and after 24% Waleska et al. 13 in their study reported 100% admissions in the first 12 hours. In the present study, 18(33.3%) patients sought treatment from traditional healers first and later got admitted to hospital. In the study conducted by Hatti et al10 65.5% of patients sought treatment from traditional healers only. 8.5% after consulting the traditional healers got admitted in the hospitals. In the study conducted by Nhachi-C-F-B in rural Zimbabwe 15.6% received treatment from traditional healers only 14. In the present study 50(92.6%) patients had pain at the site of the bite, 48(88.9%) had swelling at the site of the bite. 19(35.2%) patients had vomiting. Bleeding manifestations were seen in 11(20.4%) patients. Nigam et al. 9. also reported higher incidence of bleeding manifestations and lower incidence of ptosis. This is because the study had more viper bites than elapid bites. The incidence rate of Neurological manifestations in this study is 38.88%. In our study we observed most common neurological manifestation was ptosis (85.7%) followed by Ophthalmoplegia (42.8%). These finding are consistent with that of Sarangi et al 12 and Kulkarni et al. 15 where neurological manifestations were 11.7% and 12.5% respectively.
Table 5: showing comparison of neurotoxic bites only
The frequency of ptosis in the present study is similar to that observed in the study conducted by Sarangi et al In the present study paraplegia occurred in only one case. Whereas the incidence is very high in the study conducted by Nigam et al Respiratory failure occurred in only 38.09% of the patients in the present study whereas Sarangi et al reported 60% of respiratory failure patients and Nigam et al reported 75% of respiratory failure patients. In the studies conducted by Sarangi et al and Nigam et al all those who developed respiratory failure died. In the present study, 8(38.09%) patients developed respiratory failure. Five of them were put on ventilator and all of them survived. In 3(14.3%) ventilator support could not be instituted for various reasons and all three of them died.
CONCLUSION The incidence rate of Neurological manifestations in the study was 38.88% and most common neurological manifestation was ptosis (85.7%) followed by Ophthalmoplegia (42.8%).
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home