|
Table of Content Volume 14 Issue 3 - June 2020
A study of systemic involvement in snake bites
Mirza Hammad Ali Baig1*, Mohd Asif Hussain2
1Assistant Professor, 2Senior Resident, Department of General Medicine, ESIC Medical College, Gulbarga, Sedam Road 585106, INDIA. Email: drhammadbbaig@gmail.com
Abstract Background: Nervous system complications and systemic involvement in snake bite leads to high rate of morbidity and mortality, thus prompt recognition of neurotoxic features and appropriate treatment can reduce the morbidity and mortality in snake bite cases. Aim and objective: To study the systemic involvement in snake bite patients Methodology: This clinical, prospective study was conducted on all the patients coming with a history of snake bite attending “Al Ameen Medical College Hospital, Bijapur and District Hospital Bijapur” during the period from January 2013 to December 2013. Any patient brought to the Al Ameen medical college hospital and district hospital, Bijapur with a history of snake bite was observed for signs of envenomation. They were carefully observed till it was definite that there was no reaction or features of systemic poisoning. Results and discussion: 18(33.3%) patients had local manifestations only, 21(38.9%) patients had neuroparalytic features and 14(25.8%) patients had haemotoxic features and 1(1.8%) had both neuroparalytic and haemotoxic features. Overall mortality was 6(11.1%) out of 54 patients. Cause of death in 3 patients was respiratory failure and in 3 patients AKI. Key Word: snake bites.
INTRODUCTION Snakes are intrinsically fascinating and form an important component of the biota. It is natural that their curious mode of propulsions, their venom and their constricting mechanisms have made them the most important group of predators; this maintains the natural balance in the forests and deserts and in the plains and hills of India. The civilisation of man appears to have increased their importance as these reptiles prey on frogs, birds, rats and mice and other household pests. Human beings have the propensity to come into contact with a variety of venomous snake which elaborate venom for defense or predation. The world mortality from snake bite has been as high as 30,000 - 40,000 per year (Wallace – 1971). In the Indian subcontinent most of the deaths are attributed to, bites from snakes of the Elapidae family (Cobra and Krait) though bites from snakes of the Viperidae family are also common1. In India, there are 216 species of snakes of which 52 are poisonous and belong to three major families2. The incidence of snake-bite is found to be higher in the Southern part of India in Tamil Nadu and Kerala. In 1969, the total numbers of patients admitted following snake-bite to the Government Hospitals in India were around 24000 of which 1,100 (4.6%) died3. Poisonous snakes are those which possess venom glands and specialized venom conducting fangs which enable them to inflict serious injury to the victim. The venomous snakes belong to the family Elapidae, Viperidae, Hydrophidae. The symptoms following snake bite vary according to the size and the species of the snake involved. Headache, vomiting, loss of consciousness, abdominal pain , pain in the regional lymph nodes, faintness, sweating , pallor , the passage of blood stained urine, proteinuria, diarrhea, spitting of the blood , the coughing of blood , the vomiting of the blood , loss of vision and less often convulsions occur. These latter symptoms may arise within minutes of the bite 4.the symptoms arising within ½ an hour after the snake bite are not necessarily due to fear as is suggested by some 5,6. In viperine Snake bites local lesions along with different systemic effects like hemorrhage, shock and hemolysis are important while in the Elapid bites, the most common Cause of death is neuromuscular paralysis and brain stem lesions. These effects so much mimic the myasthenia features that authors were prompted to use neostigmine in such cases. A dramatic effect has been observed especially in a case study conducted in the Darbhanga Medical College Hospital from February 1975 to March, 1979. Effects of cobra-bite have been well reviewed by Ahuja and Singh in 1956. The symptoms were pain at the site of the bite affecting the surrounding area to some extent, swelling extending up to the affected limb, numbness, lassitude, drowsiness and intoxication associated with difficulty in breathing.7 The initial symptoms may be followed by a sense of receding consciousness. Eye sight becomes dim and there is marked drooping of the eyelids. The pulse is weak, the heart action is speeded and. speech becomes labored. There is dribbling of saliva and mucous as well as paralysis of the tongue and laryngeal muscles associated with difficulty in breathing. In later stages there may be paralysis of the limbs and loss of sphincter control. The interval between the occurrence of the bite and the onset of paralysis and other neurotoxic symptoms is seldom more than 2-3 hours and is frequently less. A similar picture was given by Purananda in 1956 from cases of cobra bite in Thailand. Chugh et al.8 in 1975, Dash et al. in 1976 and Sarangi et al. 9, 1977 reported on the neurological manifestations and are of opinion that respiratory paralysis is the prime cause of death in India and hence energetic and prompt measures instituted at the appropriate time go a long way in mitigating permanent neurological handicaps. Present study was conducted to see the systemic involvement after snake bite. Aim and objective: To study the systemic involvement in snake bite patients
MATERIAL AND METHODS This study was conducted on all the patients coming with a history of snake bite attending “Al Ameen Medical College Hospital, Bijapur and District Hospital Bijapur” during the period from January 2013 to December 2013. Any patient brought to the Al Ameen medical college hospital and district hospital, Bijapur with a history of snake bite was observed for signs of envenomation. They were carefully observed till it was definite that there was no reaction or features of systemic poisoning. Inclusion Criteria:
Exclusion Criteria: Patients with history of suspected snakebite where in
The patients who showed either features of local or systemic envenomation were admitted to the intensive care unit. A proforma was prepared to enter the case notes and the progress of the patients. A detailed physical examination was made at the time of admission to assess the type and severity of systemic involvement. Every effort was made to identify the snake if it was brought by the patient's attenders. From the clinical presentation, it was possible to identify the type of envenomation, whether neurotoxic or haematotoxic. The bite site is inspected. The number and type of fang marks are noted and the type of local reaction is described . The vital signs of the patient are assessed and investigations like bleeding time, clotting time, blood urea and urine output was done. A detailed assessment of the neurological system is made with observation for the presence of ptosis, diplopia, slurring of speech, dysphagia or respiratory insufficiency. The patient is examined for any hemorrhagic spots, spontaneous bleeds, retinal hemorrhages, hematuria, gastrointestinal bleeds etc. Based on the clinical picture at the time of admission, patients were categorised by allocating score points for each sign;
Ptosis 1 Mild cases : Score 1-5 Dysphagia 2 Moderate cases : Score 6-10 Dysarthria 3 Severe cases : 11 and above Aphonia 4 Hypotonia 5 Cyanosis 6 Labored respiration 7 Circulatory failure 8 Coma 9
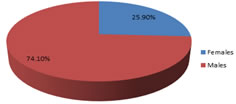
Besides the medical management in the form of antibiotics and analgesics, patients with respiratory paralysis were intubated and artificial ventilation and supportive care given to tide over the period of crisis. Patient with definite features of envenomation were given the polyvalent ASV and tetanus prophylaxis. Patients who developed cranial nerve palsies especially of the 9th and 10th cranial nerves were given pharyngeal and laryngeal toilette through a cuffed endotracheal tube and respiratory paralysis was anticipated. Patients with respiratory distress were kept on intermittent positive pressure ventilation till the ability to maintain spontaneous respiratory movements is gained. Supportive care of the skin to prevent bed sores, bladder and bowels to prevent infection, maintenance of electrolyte balance, calorie intake and adequate hydration follows till the complete recovery of the paralysed patient. Data was analysed with appropriate statistical tests. Study is Ethically approved by Institution. RESULTS A total of 66 patients of snakebite were studied. Out of them 12 bites were non poisonous and 54 were poisonous. Out of the 54 patients 21(38.9%) were in the age group of 31-40 years, 12(22.2%) were in the age group of 21-30 years. 9(16.7%) were in the age group of 41-50 years, 7(13%) were in the age group of 11-20 years and 2(3.7%) in the age group of 51-60 years. In the present study 40(74.1%) were males and 14(25.9%) females. In the present study 40(74.1%) patients were from rural population and 14(25.9%) from urban population. The ratio was 2.9:1. In the present study 41(75.9%) patients were admitted during the period May to October. The incidence was least between January and April. Only 7(13%) patients were admitted during this period. In 29(53.7%) patients bites were on the lower extremity. In 22(40.7%) patients bites were on the upper extremity. In 1(1.8%) case it was on the chest and in 1(1.8%) it was on the right armpit. In 1(1.8%) case bite mark on upper extremity. In our study in 22(40.7%) patients biting snake’s species could not be identified. In 7(13%) patients the biting species was Cobra, in 10(18.5%) it was Krait and in 15(27.8%) it was Viper. In the present study 50(92.6%) patients had pain at the site of the bite, 48(88.9%) had swelling at the site of the bite. 19(35.2%) patients had vomiting. Bleeding manifestations were seen in 11(20.4%) patients Abdominal pain was present in 5(9.2%) Oliguria and Anuria were present in 4(7.4%) patients. Inability to open eyes and or difficulty in swallowing difficulty in respiration and weakness of limbs were present in 21(38.9%) patients. We found 21(38.9%) patients had neuroparalytic features, 11(20.4%) patients had haematotoxic features, 1(1.8%) had both, and 18 (33.3%) patients had local manifestations only. Urine output was measured for all cases. 11 of the patients had urine output less than 400ml/day.3 out these 11 patients were referred for dialysis. Remaining 8 of the patients recovered spontaneously by the use of conservative measures. Urine output was abnormal in 20.7% cases. Many of the patients were dehydrated due to travel to the Al Ameen medical college hospital and District hospital, Bijapur or had recurrent episodes of vomiting or blood loss which contributed to a pre renal element. 11 out of 54 patients had blood urea more than 60mg%. A moderate rise of blood urea from 40-60mg% was not given much significance as these patients would have suffered from extracellular volume depletion. 8 of the 11 patients recovered spontaneously by conservative measures without hemodialysis. 3 of the 11 patients were referred for hemodialysis. 2 of which died while shifting to higher centre and 1 patient could not undergo dialysis because of financial reasons. Blood urea was abnormal in 20.7% cases. A serum level of Sodium 135-145mg/L was taken as normal. 50 of the patients had normal values. 4 of the patients had serum sodium more than 145mg/L. However Serum Sodium never rose more than 148mg/L. Serum sodium was abnormal in 7.4% cases. A serum Potassium level of 3.5-5.5mgL was taken as normal. 3 of the 54 patients had values less than 3.5mg/L. Serum Potassium was found abnormal in 5.6% cases. 10 out of 54 cases showed a prolongation of the clotting time more than 15 minutes. Bleeding time and clotting time was prolonged in 10 out of 54 cases. Bleeding and clotting time abnormality was seen in 18.5%. Microscopic hematuria was seen in 5 out of 54 cases that is 9.3% cases In the present study all 11 cases of acute kidney injury managed conservatively. Eight of them recovered. The other 3 were advised dialysis therapy and referred to higher centers. Two of them died while shifting to higher centre for dialysis and one could not the cost of the dialysis treatment. In our study 18(85.8%) out of 21 neurotoxic bites received both neostigmine and A.S.V. One (4.5%) patient was given only neostigmine and no A.S.V .3(13.6%) patients did not receive neostigmine because of non availability. One patient who did not receive neostigmine died of sudden respiratory failure. This patient could not be but on ventilator support. Three patients who received both neostigmine and A.S.V died. In present study 4(7.4%) patients died though they were admitted within 24 hours. In one ventilator support could not be instituted as he died while shifting to Al Ameen medical college hospital. One patient had AKI. He died while shifting to higher centre for dialysis therapy. Another patient developed respiratory failure but he could not afford the costs of mechanical ventilation treatment. Another patient died suddenly of respiratory failure. Two (3.6%) patients who died were admitted after a delay of 80 and 120 hours of bite.
TABLE 1: Distribution of poisonous snake bites according to months
Figure 1: Distribution of poisonous snake bite patients according to sex
Table 2: Distribution of snake bite patients according to symptoms
Table 3: Clinical profile of poisonous snake bite patients
Table 4: Investigation results in poisonous snake bite patients
DISCUSSION There was 1(1.8%) patient each in the age group of 0-10 61-70 and 71-80 years. Thus 40 patient each in the age group of 0-10 61-70 and 71-80 years. Thus 40 patient each in the age group of 11-40 years. These findings are consistent with the findings of Nigam et al.10 , Hatti et al.11 and Bhat et al. 12 The male to female ration was 2.9:1 This is similar with the findings of Nigam et al.10 and Bhat et al. 12, However the ratio was 1.2:1 according to Hati et al.11 In the present study 40(74.1%) patients were from rural population and 14(25.9%) from urban population. The ratio was 2.9:1. The findings are consistent with other Indian reports of Bhat et al. 12and Kulkarni et al. 13 However, Waleska et al. from Brazil reported that 58.6% of patients were from urban areas and 41.4% from rural areas 14 In the present study 41(75.9%) patients were admitted during the period May to October. These findings are consistent with those of Bhat et al. 12 and Nigam et al. 10 Snakes come out of their habitats during rainy seasons. This is probably the cause for increased incidence in rainy season. Also there is difficulty in seeing the snakes during rainy season amidst the surrounding greenery in the fields. Bhat et al. 12 reported 91% of admissions from May to September. Nigam et al.10 reported 71.4% of admissions from May to August. Hati et al.11 reported 56% of admissions from May to August. In 29(53.7%) patients bites were on the lower extremity. These on the lower extremity outnumber those of Sawai and Honama et al. 15, Hati et al.11 and Bhat et al.12 In our study 31.5% were admitted after 24 hours and 68.5% before 24 hours. These findings are consistent with the study of Bhat et al.12 who reported that 72% of patients were admitted within 24 hours and 28 and after 24% Waleska et al.14 in their study reported 100% admissions in the first 12 hours. In the present study 50(92.6%) patients had pain at the site of the bite, 48(88.9%) had swelling at the site of the bite. 19(35.2%) patients had vomiting. Bleeding manifestations were seen in 11(20.4%) patients Abdominal pain was present in 5(9.2%) Oliguria and Anuria were present in 4(7.4%) patients. Inability to open eyes and or difficulty in swallowing difficulty in respiration and weakness of limbs were present in 21(38.9%) patients. Sarangi et al.9 reported higher incidence of Bleeding manifestations than respiratory failure. Nigam et al.10 also reported higher incidence of bleeding manifestations and lower incidence of ptosis. This is because their studies had more viper bites than elapid bites. In the present study neurotoxic profile is seen more often than haemotoxic profile. This is because there were more elapid bites than viper bites in the present study. There were 14 cases with haemotoxic bites, out of them 3(21.4%) died. The mortality was1.96% according to Bhat et al.12, 28.5% according to Nigam et al.10and 10.3% according to Sarangi et al.9 K.p Chandrashekar and Mathew Thomas 16 reported in 1989 that 17.3% of their cases had neurological manifestations(28/162), 75% had ptosis and Ophthalmoplegia,75% had altered consciousness, 39% had respiratory paralysis, 14.3% had dysphagia and 10.8% patients were in coma. Banerjee et al. 17 and Sarangi et al.9 reported 43% and 6% incidence of neurological manifestations respectively. Among cases with systemic poisoning Bhat et al. reported 8.2% incidence of neurological manifestations. H sahoo and J.P Das 18 report mental confusion in 33.2% cases, Coma in 10.6% cases, convulsions in 5.5.% cases, Hemiplegia in 5.5% cases, ptosis in 80% cases, dysphagia and medullary palsy in 80% cases. In the present study all 11 cases of acute kidney injury managed conservatively. Eight of them recovered. The other 3 were advised dialysis therapy and referred to higher centers. Two of them died while shifting to higher centre for dialysis and one could not the cost of the dialysis treatment. In the study conducted by K.S. Chugh et al.8 5 patients out of 8 who developed acute kidney injury were given dialysis treatment and they all survived. In one case recovery occurred without dialysis treatment.
CONCLUSION Snake bite manifests as acute kidney injury and respiratory paralysis which is major cause of death.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home