|
Table of Content Volume 15 Issue 1 - July 2020
A study of atrial volume and it’s determinants as prognostic factor in patients with dilated cardiomyopathy
Satyendra Kumar A1, Y. Vivekananda2*
1Assistant Professor, Department of Cardiology, GSL Medical College, Rajahmundry, Andhra Pradesh, INDIA. 2Assistant Professor, Department of Cardiology, Katuri Medical College And Hospital, Guntur, Andhra Pradesh, INDIA. Email: dr.nandavivek@gmail.com
Abstract Background: Cardiomyopathy is a complex disease process that can affect the heart of a person of any age. Cardiomyopathy is an important cause of morbidity and mortality among the world's aging population. The utility of LA volume and function for monitoring cardiovascular risk and for guiding therapy is an evolving science and may prove to have a very important public health impact. Aim and objective: To study the atrial volume and it’s determinants as prognostic factor in patients with dilated cardiomyopathy Methodology: Present study was prospective study carried out on 50 Patients with diagnosis of Congestive Heart failure. Study period May 2018 to April 2019. The left atrial functions of the patients were evaluated by performing transthoracic echocardiography. The LV ejection fraction, LV volumes, and LV mass were determined for a total number of three times; first at the time of the visit to the hospital, and then at end of first and sixth months of follow up. Data was analysed with appropriate statistical tests. Results: Patients with DCM showed a larger LA VOLUME (75.57 ± 27.60 ml,) compared with normal control subjects (58.57 ± 21.37 p < 0.016). Differences in the E-wave velocity (0.92 ± 0.25 vs. 1.07 ± 0.20; p <0.029), A-wave velocity (0.68 ± 0.32 vs. 0.82 ± 0.16 p < 0.066), E/A ratio (1.71 ± 0.90 vs. 1.30 ± 0.25 p < 0.05), or DT (165 ± 40.11 vs.197.25± 24.33 p <0.002) were observed between patients and control subjects. Key Word: atrial volume, prognostic factor.
INTRODUCTION Cardiomyopathies are conditions in which the normal muscular function of the myocardium has been altered by specific or multiple etiologies, with varying degrees of physiologic compensation for that malfunction. Cardiomyopathies have multiple etiologies.1-3 The degree and time course of malfunction are variable and do not always coincide with a linear expression of symptoms. Persons with cardiomyopathy may have asymptomatic left ventricular systolic dysfunction, left ventricular diastolic dysfunction, or both.4,5 In adults, the prevalence is one in 2500 individuals, with an incidence of seven per 1,00,000 per year. In adults, dilated cardiomyopathy arises more commonly in men than in women. In children, the yearly incidence is 0.57 cases per 1,00,000 per year. Two thirds of children are thought to have idiopathic disease.6,7 The classification of cardiomyopathy has varied over the past century. Cardiomyopathies may be simply divided into dilated or nondilated categories.1,2 Within each of these groups, the myocardium may be hypertrophic or nonhypertrophic, and it may be accompanied by a restrictive (diastolic ventricular dysfunction) and/or congestive (systolic ventricular dysfunction) physiology. Dilated cardiomyopathy is characterised mainly by left ventricular systolic dys function (abnormality of contraction), with an associated increase in mass and volume. Dilated cardiomyopathy (DCM) manifests hemodynamically as decreased cardiac output and increased pulmonary venous pressure5. In large population-based studies, it has been demonstrated that LA size is an important predictor of cardiovascular outcome.8-11 Tsang et al... recently demonstrated that a larger indexed LA volume predicted a higher risk of cardiovascular events after adjustment for age, gender and other covariates. Patients with a severely increased left atrium (≥40 ml/m2) had the highest risk for the development of cardiovascular events (hazard ratio 6.6).12 The incremental value of LA size over conventional risk factors has been demonstrated in several studies.12-14 In the Framingham Heart study 15 it was demonstrated that LA enlargement was a significant predictor of death in both men and women. The relative risk of death per 10 mm increment in LA size was 1.3 for men (95% CI 1.0 to 1.5) and 1.4 for women (95% CI 1.1 to 1.7). For assessment of LA size various echocardiographic techniques are available, including transthoracic, transoesophageal and intracardiac echocardiography. Transthoracic echocardiography is most commonly used in daily clinical practice to assess LA size. Present study was conducted to study the atrial volume and it’s determinants as prognostic factor in patients with dilated cardiomyopathy.
MATERIAL AND METHODS Present study was prospective study carried out at GSL MEDICAL COLLEGE, Rajahmundry. Study population was 50 Patients admitted in the Intensive Coronary care unit with a diagnosis of Congestive Heart failure and matched controls for age and sex. Inclusion Criteria: Patients admitted in the Intensive Coronary care unit of the with a diagnosis of 1) Congestive Heart failure (New York Heart Association class II to IV) for ≥3 months while receiving medical treatment; 2) Consecutive patients who had a complete echocardiographic Doppler examination with a LV ejection fraction of ≤40% on the basis of echocardiographic evaluation using a modified Simpson’s method will form the study population. Exclusion Criteria: patients with 1) Significant organic mitral or aortic valve disease 2) The presence of clinical or echocardiographic features of amyloidosis or constrictive pericarditis 3) A recent myocardial infarction <6months.4) Children less than 14 years of Age Study was approved by ethical committee of the institute. A valid written consent was taken from patients or guardians of the patients after explaining study to them. According to the study protocol, the left atrial functions of the patients will be evaluated by performing transthoracic echocardiography. Echocardiographic images were acquired in the standard parasternal and apical views. The LV ejection fraction, LV volumes, and LV mass were determined for a total number of three times; first at the time of the visit to the hospital, and then at end of first and sixth months of follow up. Left atrial maximal volume (LAmax) is measured at LV end systole, and LA minimal volume (LAmin) at LV end diastole from the apical four-chamber view (area–length method). Left ventricular end-diastolic and end-systolic volumes (area–length method) and EF is measured off-line from the apical four-chamber view. Mitral E-wave (E) and A-wave (A) velocities, E/A ratio, and E-wave deceleration time (DTE) is also measured off-line. The last variable is measured as the interval (in milliseconds) from peak early mitral filling to an extrapolation of the deceleration to 0 m/s. All measurements were obtained from the mean of 3 beats for patients in sinus rhythm and 5 beats for those with AF. A restrictive mitral inflow pattern was defined as an E/A > 2 or between 1 and 2 and DTE < 140 ms in patients in sinus rhythm or a DTE<140 ms in patients with AF. Mitral regurgitation was assessed by color flow Doppler echocardiography. Data was analysed with appropriate statistical tests.
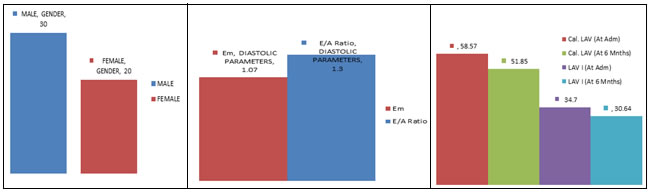
RESULTS 50 Patients with a diagnosis of DCMP who had a complete echocardiographic Doppler examination within one month of clinical evaluation and who were followed for 3 months formed the study population. The duration of the disease was taken to be the number of years of awareness of cardiac impairment. Twenty subjects in sinus rhythm, with no history of cardiac disease and with entirely normal echocardiographic findings were enrolled as a control group. A total of 50 patients (30 men and 20 women; age 36.08 ±16.13 years) formed the study population. The etiology of cardiomyopathy was idiopathic in 76%, viral myocarditis in 12%, peripartum cardiomyopathy in 8% and drug induced in 4%. Mean duration of symptoms was 1.8 years. Patients with DCM showed a larger LA VOLUME (75.57 ± 27.60 ml,) compared with normal control subjects (58.57 ± 21.37 p < 0.016). Differences in the E-wave velocity (0.92 ± 0.25 vs. 1.07 ± 0.20; p <0.029), A-wave velocity (0.68 ± 0.32 vs. 0.82 ± 0.16 p < 0.066), E/A ratio (1.71 ± 0.90 vs. 1.30 ± 0.25 p < 0.05), or DT (165 ± 40.11 vs.197.25± 24.33 p <0.002) were observed between patients and control subjects. The determinants of LA volume were defined by means of linear regression analysis TABLE 2. There was negative correlation between the LA volume, LA volume index and LV ejection fraction.TABLE.3
Table 1: Group Statistics
Table 2: Determinants of LA Volume
Table 3: Correlation of LAV between duration and degree of MR severity
Figure 1: distribution of patients Figure 2: Doppler parameters Figure 3: LA parameters at admission and according to sex attend of 6 months
DISCUSSION The present study showed that LA remodeling is frequent, in patients with DCM. Left atrial volume is mainly determined by the degree of LV dilation, diastolic dysfunction, and the extent of MR. In patients with chronic heart failure due to DCM, diastolic dysfunction is an important hallmark of the severity of the disease. The degree of diastolic impairment correlates with symptoms and prognosis more closely than does EF107. 16,17 However, the predictive power of diastolic markers has been frequently but not uniformly confirmed. 18 This is probably due to the strong load dependency of mitral parameters, which can dramatically change after blood volume depletion. 19 It has been shown that the predictive power of mitral inflow can be enhanced when analyzed in relation to loading modification. 20 The role of LA size as a diastolic marker is well known, 21 and, accordingly, we found a relation between atrial volume and diastolic markers though statistically non significant. Interestingly, the predictive value of atrial volume is stronger and independent of echocardiographic Doppler diastolic parameters. This might be related to a lower load dependency due to increased fibrosis and reduced elastic recoil in a chronically enlarged atrium. Functional MR is a major confounding factor in the hemodynamic of patients with LV systolic dysfunction. 22 Mitral regurgitant volume is a key determinant of atrial volume,18 which may reflect the severity, duration, and prognosis of MR. 23 In this study, the predictive role of LA volume proved to be more powerful than MR, independent of the degree of MR, and it was confirmed in both the group of patients with and the group without MR. LA enlargement represents a strong predictive marker, because the atrial chamber is a window allowing comprehensive evaluation of several factors associated with a bad prognosis, which are often difficult to document separately. Atrial size might also reflect marked hemodynamic atrial overload in specific phases during the course of chronic heart disease, such as during exercise, giving evidence of temporal hemodynamic impairment (MR or diastolic dysfunction) which otherwise would remain silent. 24 An appealing suggestion is that LA volume stores information on the history of the disease, highlighting its duration. Accordingly, in this study, LA volume correlated weakly but significantly with the duration of the disease. LA enlargement represents a strong predictive marker, because the atrial chamber is a window allowing comprehensive evaluation of several factors associated with a bad prognosis, which are often difficult to document separately. Atrial size might also reflect marked hemodynamic atrial overload in specific phases during the course of chronic heart disease, such as during exercise, giving evidence of temporal hemodynamic impairment (MR or diastolic dysfunction) which otherwise would remain silent. 25 It is possible that in patients with DCM, atrial enlargement could also be due to concomitant atrial myopathic disease caused by a more widespread primary pathologic process. 26 Others studies have included LA size in the survival analysis. In one study 27 showed that LA size predicted the outcome independent of the restrictive mitral pattern, New York Heart Association functional class and EF, but they confirmed that the restrictive pattern had a higher predictive power than did atrial size. A possible explanation might be the difference between their patient cohorts and ours. Both studies analyzed populations of patients with very severe diastolic dysfunction, with a prevalence of a restrictive pattern of 42% and 46%, respectively. The narrow range of these pathophysiologic variables raises the question as to whether those cohorts can adequately represent the whole spectrum of the disease. In contrast, our population was characterized by a wider range of systolic dysfunction, and a 58% prevalence rate of a restrictive pattern, indicating a severe disease state.
CONCLUSION Left atrial enlargement carries important clinical and prognostic implications. Left atrial volume is superior to LA diameter as a measure of LA size, and should be incorporated into routine clinical evaluation.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home