|
Table of Content Volume 15 Issue 1 - July 2020
Metabolic syndrome among elderly in a tertiary care center
Nagaraj S K1, Shashanka K S2*, Shashidhar G3, Vigneshwar M4
1, 2Postgraduate, 3Professor, 4Assistant Professor, Department Of General Medicine, MVJ Medical College And Research Hospital, Bangalore, Karnataka, India. Email: shashankksrinivas@gmail.com
Abstract Background: Metabolic syndrome (MS) is a premorbid condition with an inter-related cluster of metabolic abnormalities that involves glucose and lipid dysregulation, abdominal obesity and elevated blood pressure. It is estimated that 25 p.c of the world’s population has MS. The geriatric population (aged ≥60 years) is increasing rapidly in India, during the year 1991 it accounted for 6.7 p.c of the total population, rising to 7.4 p.c by the turn of the new millennium and is expected to increase to around 10.7 p.c by 2021 due to demographic transition. Aim and Objectives: To study the prevalence of metabolic syndrome and its risk factors among geriatric population. Material and Methods: A hospital-based, analytical cross-sectional study was conducted in the Department of General Medicine, MVJ Medical College and Research Hospital, Bangalore, Karnataka All the patients attending the General Medicine OPD aged 60 years and above who were willing to participate voluntarily were included. The study was conducted for a period of 6 months from 1st October 2019 to 31st March 2020. IEC approval and written consent were obtained. A detailed history was taken and examination done. A predesigned, pretested, semi-structured questionnaire was used to collect information regarding individuals’ characteristics, personal habits, physical activity and harmful habits. Biochemical profile and anthropometric measurements were obtained. Data was analyzed in SPSS version-22 trial. Results: Prevalence of metabolic syndrome among the geriatric population was reported to be 44.7 p.c. Conclusion: Rapid changes in lifestyle, sociodemographic factors and disease transition in India, the metabolic syndrome prevalence found to be in an increasing trend. Keywords: Elderly, Geriatric, Metabolic syndrome.
INTRODUCTION Metabolic syndrome (MS) is a premorbid condition with an inter-related cluster of metabolic abnormalities that involves glucose and lipid dysregulation, abdominal obesity and elevated blood pressure.1 This premorbid condition develops due to insulin resistance and factors such as physical inactivity, obesity, poor diet and genetics.2 It may increase the risk of development various conditions such as type-2 diabetes mellitus, coronary artery disease (CAD) and other cardiovascular diseases.3 Individuals with metabolic syndrome are at greater risk of cardiovascular mortality and morbidities.4 The geriatric population (aged ≥60 years) is increasing rapidly in India, during the year 1991 it accounted for 6.7 p.c of the total population, rising to 7.4 p.c by the turn of the new millennium and is expected to increase to around 10.7 p.c by 2021 due to demographic transition.5 During the past decades, the prevalence of MS has markedly increased worldwide.6 It is estimated that 25 p.c of the world’s population has MS.7 This estimate varies widely due to the age, ethnicity and gender of the population studied.8 About one third of the urban population in India has metabolic syndrome.9 As per International Diabetes Federation (IDF) - 2005 criteria the definition of metabolic syndrome was the presence of central obesity (waist circumference ≥90 cm in men and ≥80 cm in women), plus ≥2 of the following criteria: blood pressure ≥130/85 mmHg or taking drug treatment for hypertension; serum triglyceride ≥150 mg/dL or taking specific treatment for this lipid abnormality; serum HDL cholesterol (HDLc) <40 mg/dL in men and <50 mg/dL in women, or taking specific treatment for this lipid abnormality; fasting blood glucose ≥100 mg/dL, or previously diagnosed type 2 diabetes and taking specific drug treatment.10
MATERIAL AND METHODS A hospital-based, analytical cross-sectional study was conducted in the Department of General Medicine, MVJ Medical College and Research Hospital, Bangalore, Karnataka. All the patients attending the General Medicine OPD aged 60 years and above who were willing to participate voluntarily were included. Patients who were severely ill, with cognitive difficulties and those who were not willing to fast over-night were excluded. The study was conducted for a period of 6 months from 1st October 2019 to 31st March 2020. IEC approval and written consent were obtained in prior. A detailed history was taken and examination done. A predesigned, pretested, semi-structured questionnaire was used to collect information regarding individuals’ characteristics, personal habits and harmful habits. Physical activity or performance status of the individuals was assessed by a modified ECOG11 (Eastern Cooperative Oncology Group) scale. Individuals’ pattern of physical exercise was assessed by the total time spent every day walking and/or exercising, that may include pranayama or yoga or any other forms of exercise (for at least 30 minutes per day for a minimum of 5 days per week). Anthropometric measurements were obtained for every individual (height, weight, waist circumference) and BMI was calculated. Blood pressure was recorded for all the individuals who participated in the study. About 10 mL of blood was obtained from each individual after overnight fasting to estimate fasting blood glucose, serum triglyceride and high density lipo-protein (HDL) cholesterol. The data obtained was entered in Microsoft Excel and analyzed in SPSS version-22 trial. Appropriate statistical tests were used.
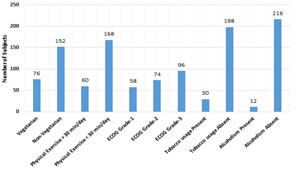
RESULTS About 228 individuals who participated in the present study about 44.7 p.c (102) prevalence of metabolic syndrome was reported. Table-1 reports the sociodemographic factors of the study, majority 38 p.c (86) subjects were between 70-79 years; majority 53.5 p.c (122) were males and 46.5 p.c (106) were females; majority 36.4 p.c (83) of the subjects were Hindu by religion; majority 66.7 p.c were literates and 33.3 p.c (76) were illiterates. Figure-1 reports that majority 66.7 p.c (152) were non-vegetarians and 33.3 p.c (76) were vegetarians; majority 73.7 p.c (168) of the subjects exercised less than 30 minutes a day and 26.3 p.c (60) of the subjects exercised >30 minutes a day; majority 42.1 p.c (96) subjects reported physical activity ECOG grade-2; about 86.8 p.c (198) subjects did not have a harmful habit of smoking; about 94.7 p.c (216) subjects did not have a harmful habit of alcoholism. Body mass index (BMI) of the subjects was reported be less than 23kg/m2 in majority of the individuals 51.7 p.c (118) and >23kg/m2 among 48.3 p.c (110) subjects respectively. Table-2 reports that the mean SBP among the subjects with metabolic syndrome was 145 + 7.3mm of Hg and among the subjects without MS was 129 + 10.7mm of Hg; the mean DBP among the subjects with metabolic syndrome was 97.2 + 2.8mm of Hg and among the subjects without MS was 87 + 4.8mm of Hg; the mean waist circumference among the subjects with metabolic syndrome was 92.6 + 1.8cms and among the subjects without MS was 77.3 + 6.7cms; the mean BMI among the subjects with metabolic syndrome was 26.2 + 1.8 kg/m2 and among the subjects without MS was 21 + 2.8 kg/m2; the mean serum TG level among the subjects with metabolic syndrome was 156.4 + 11.2mg/dL and among the subjects without MS was 122.4 + 8.7mg/dL; the mean serum HDL among the subjects with metabolic syndrome was 39.4 + 2.2mg/dL and among the subjects without MS was 45.4 + 4.6mg/dL; the mean FBG among the subjects with metabolic syndrome was 115.6 + 9.9mg/dL and among the subjects without MS was 73.6 + 4.4mg/dL respectively. Table-3 reports MS among the individuals as per International Diabetes Federation (IDF) – 2005 criteria, the presence of central obesity (waist circumference ≥90 cm in men and ≥80 cm in women) among 91.1 p.c individuals; the presence of blood pressure ≥130/85 mmHg or taking drug treatment for hypertension among 86.2 p.c individuals; the presence of serum triglyceride ≥150 mg/dL or taking specific treatment among 37.2 p.c individuals; the presence of serum HDL cholesterol (HDLc) <40 mg/dL in men and <50 mg/dL in women, or taking specific treatment among 38.2 p.c individuals; the presence of fasting blood glucose ≥100 mg/dL, or previously diagnosed type 2 diabetes and taking specific drug treatment among 76.4 p.c individuals.
Table 1: Sociodemographic Factors
Figure 1: PERSONAL and HARMFUL FACTORS
Table 2: MEAN AND STANDARD DEVIATIONS OF VARIOUS PARAMETERS IN RELATION TO METABOLIC SYNDROME
Table 3: Components of metabolic syndrome
DISCUSSION Among the elderly population of the present study, the overall prevalence of metabolic syndrome was reported to be 44.7 p.c, with a higher prevalence among women (55.4%) than men (36.8%). Pemminati S et al.12 in their study reported that the prevalence of metabolic syndrome was about 57 p.c with a higher prevalence of metabolic syndrome among females than males. Wasir JS et al.13 in their study reported that prevalence of metabolic syndrome was 40.2 p.c among the urban residents of Northern India. A study conducted in China reported that the prevalence of metabolic syndrome was 46.3 p.c among the elderly population.14 A high prevalence of metabolic syndrome among elderly women in the present study was probably due to the hormonal effects after menopause. Other Indian studies have reported a prevalence of metabolic syndrome ranging from 9.3 to 31.4 p.c respectively.15, 16
CONCLUSION Due to rapid changes in lifestyle, sociodemographic factors and disease transition in India, the metabolic syndrome prevalence found to be in an increasing trend. This high prevalence is a major concern to the country. There is need for an urgent attention of the health-care providers, policy makers and stake holders to take necessary actions.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home