|
Table of Content Volume 16 Issue 1 - October 2020
Primary sclerosing cholangitis with down syndrome
Mustafa Taskeen1*, Dileep Kadam2, Shilpa Sule3, Rajvardhan Shelke4, Dhairyasheel Patil5
1Junior Resident, Department Of Medicine, 2Professor, 3Associate Professor, 4Lecturer, 5Junior Resident, Department of Medicine, SKNMC & GH Pune, Maharashtra, INDIA. Email: drmustafataskeen@gmail.com
Abstract Background: Primary sclerosing cholangitis (PSC) is a chronic liver disease of unknown etiology characterized by the progressive inflammation, liver fibrosis, and multifocal biliary duct stenosis leads to progressive alternating biliary duct stricturing and dilatation and eventually cirrhosis requiring liver transplantation. Down syndrome is a common chromosomal anomaly associated with multiple congenital malformations and a commonly known genetic cause of intellectual disability humans. There have been many reports of the association of thyroid disease, coeliac disease, and type 1 diabetes mellitus with Down syndrome. Association with primary sclerosing cholangitis is very rare, till now only 3 cases have been reported so far. We report primary sclerosing cholangitis in a patient with Down syndrome. Key Word: down syndrome.
INTRODUCTION Primary sclerosing cholangitis (PSC) is a chronic liver disease of unknown etiology characterized by the progressive inflammation, liver fibrosis, and multifocal biliary duct stenosis leads to progressive alternating biliary duct stricturing and dilatation and eventually cirrhosis requiring liver transplantation.1Recent studies show that PSC has an overall incidence rate of 0.77 per 100,000 person-years.2 Primary sclerosing cholangitis patients are often going undiagnosed because approximately 40%-50% of patients with this disease are asymptomatic.3 Fatigue, fever, jaundice, pruritus, and vague upper abdominal discomfort are the most commonly described symptoms in primary sclerosing cholangitis patients at the time of diagnosis.4 Down syndrome is a common chromosomal anomaly associated with multiple congenital malformations and commonly known genetic cause of intellectual disability humans. The incidences in India are 1 per 850- 900 live births.5,6 Down syndrome has been associated with increased frequency of malignancies, autoimmune diseases and infections due to abnormal precocious aging.7 Evidence suggests that the immune system in Down syndrome is deficient from the very beginning, with immune dysregulation causing a tendency towards autoimmune diseases.8 We report primary sclerosing cholangitis in a patient with Down syndrome, which is rarely reported in literature.
CASE PRESENTATION A 48 years old female, k/c/o Downs Syndrome, was brought to the medicine OPD by her relatives. Chief complaints were yellowish discoloration of eyes for 2 months, constipation, loss of weight and appetite since the past 2 months, fever and cough with expectoration for 1 month. On examination patient was afebrile, pulse was 78/min, regular, equal on both sides, without radio-femoral delay. Patients’ blood pressure was 100 / 64 mm Hg, respiratory rate 16/min and respiration was abdominothoracic. Icterus (grade 2), clubbing (grade 2) and scratch marks were noted. Patient had no pallor, cyanosis, lymphadenopathy and edema feet. Her thyroid, JVP was normal. Features of Downs Syndrome (Brachycephaly, flat head, upslanting palpebral fissures, low set ears, flat nasal bridge, short neck, large tongue, short hands, single palmar crease, separation of first and second toes) were present. Patient was conscious and her higher functions could not be elicited (mentally challenged ). Abdomen was distended and umbilicus was transverse. No dilated veins , scars or sinuses. Ascites and splenomegaly ( grade 2) was present. No hepatomegaly. Primary differential diagnosis was auto immune hepatitis, Wilson’s disease, primary biliary cirrhosis, primary sclerosing cholangitis, drug induced hepatitis and cystic fibrosis. Investigations On admission hemoglobin levels were 9.8 gm/dl and platelets were 60,000. BT/CT was normal. PT was 18.32 and INR 1.3. Serum Ammonia 18 µ/dL (normal 15 to 45 µ/dL), Gamma-Glutamyl Transferase (GGT) 253 U/L (normal 9-48 U/L), IgG 1,190 mg/dL ( normal 700-1600 mg/dL) rest LFT/RFT were within normal limits. X-ray chest and ECG were normal. 2 D Echo was suggestive of normal LV size and systolic function, normal valves, mild aortic regurgitation, normal pulmonary arterial pressure and LVEF was 60 %. USG (A+P) findings were Altered echotexture of liver with intra hepatic biliary radical dilatation with Ascites. Liver span was 14 cm and spleen span was 14.5 cm. Sputum gram stain and culture suggestive of E Coli species and antibiotics were started as per sensitivity reports. Immunological and serological markers such as ANCA – MPO was positive, ANA was weakly positive. Anti SMA/ Anti LKM1/ AMA tests were negative. Liver biopsy findings were portal tracts show mild inflammatory infiltrate composed of neutrophils lymphocytes and eosinophils, cholestatic degeneration in the form of marked intra cytoplasmic cholestasis noted in perivenular and periportal areas. and diffuse macrovesicular steatosis. Findings suggestive of Primary Sclerosing Cholangitis.
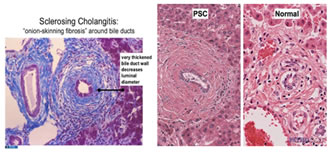
Figure 1: Liver biopsy histology slides of patient Figure 2: Typical histological findings in PSC patients
Final diagnosis small duct sclerosing cholangitis in Down syndrome. On day 11, hemoglobin levels were 7 gm/dl and platelets were 65,000. BT/CT was normal. PT was 28.5 and INR 1.9. Serum Ammonia 88 µ/dL (normal 15 to 45 µ/dL). Patient had hepatic encephalopathy and treated for same. Patient was started on Steroids but didn’t respond to treatment. Patient had massive hematemesis 1 week later. She was resuscitated but could not be revived.
Primary sclerosing cholangitis (PSC) is a rare idiopathic chronic progressive liver disease causes fibro-obliterative inflammation of the hepatic bile ducts and ultimately cirrhosis and liver failure.8 The best diagnostic approach in suspected patients with PSC are on endoscopic retrograde or magnetic resonance cholangiopancreatography (ERCP and MRCP respectively).9 Liver biopsy is not mandatory investigation but is useful in staging and excluding other causes of chronic cholestasis or autoimmune hepatitis, primary biliary cirrhosis.10 The fibro-obliterative lesion is the histological hallmark of PSC. It begins as concentric rings of fibrosis, known as onion-skinning, around bile ducts. With time, this concentric fibrosis squeezes off and obliterates the bile duct lumen, leaving behind a fibrous plug or scar. There is often a mild lymphocytic infiltrate that accompanies the fibrosis. Small duct PSC, also known as “pericholangitis”, presents typical clinical and laboratory tests for the disease but with normal cholangiography and accounts for 5 to 20% of patients with PSC.11 Table 1: Histological findings in various stages of primary sclerosing cholangitis
PSC - primary sclerosing cholangitis Since there is no curative treatment for PSC except for liver transplantation, one should focus on treating and preventing the complications of the disease. There have been many reports of the association of thyroid disease, coeliac disease, and type 1 diabetes mellitus with Down syndrome.12 Association with primary sclerosing cholangitis is very rare, till now only 3 cases have been reported so far. Devendra Mehta reported a 21 years old patient with Down syndrome, multiple autoimmune disorders and PSC.13 Vajro P reported a Down syndrome patient with hepatobiliary disease due to sclerosing cholangitis predating the overt clinical appearance of Crohn’ s disease.14 Marina Guitton Rodrigues, et al., reported a case of overlapping PSC and autoimmune hepatitis in a 44 years old patient with Down syndrome, underwent liver transplantation.15 Though due to antenatal screening in high risk mothers, incidence of Down syndrome is reducing but life expectancy in Down syndrome is increasing due to availability of better medical care. With increased survival rates, the spectrum of diseases reported in these patients has been growing, particularly autoimmune diseases.12 Treating physician should always kept in mind various autoimmune diseases while treating in patients with Down syndrome.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home