|
Table of Content Volume 16 Issue 1 - October 2020
A study of complications and mortality in acute myocardial infarction among diabetic and non diabetic patients
Sham P Toshniwal1, Sanjay B Jagtap2*, Dhakne Anand3, Khan Aref Yousuf4
1Assistant Professor, 2Associate Professor, 3,4Junior Resident, Department of Medicine, Vilasrao Deshmukh Government Institute of Medical science, Latur, Maharashtra, INDIA. Email: arefkhan91@yahoo.in
Abstract Background: Cardiovascular disease including acute myocardial infarction are more common among diabetics than among non-diabetics. There are a lot of controversies regarding the clinical profile of acute myocardial infarction and the risk factors for AMI. Present study was conducted to compare complications and mortality in AMI patients with diabetes and without diabetes. Aim and objective: To compare the complications and mortality in acute myocardial infarction among diabetic and non diabetic patients Methodology: 60 diabetic AMI and 60 non-diabetic AMI were studied in the study for post AMI complication and mortality. Results: Post AMI complications are common in both group are sinus tachycardia and pump failure is more common in diabetic group. In hospital mortality among diabetic AMI was 30% and non-diabetic AMI was 13.33%. It was statistically significant (P<0.05). Pump failure was an important cause of mortality and was commonly seen with females who had a poor hospital course Key Word: Diabetes mellitus.
INTRODUCTION The disease burden related to diabetes is high and rising in every developing and developed country, it is fuelled by the global rise in the prevalence of obesity and unhealthy lifestyles. The latest estimates show a global prevalence of 382 million people with diabetes in 2013, expected to rise to 592 million by 2035. The aetiological classification of diabetes has now been widely accepted. Type 1 and type 2 diabetes are the two main types, with type 2 diabetes accounting for the majority (>85%) of total diabetes prevalence. Both forms of diabetes can lead to multisystem complications of microvascular endpoints, including retinopathy, nephropathy and neuropathy, and macrovascular endpoints including ischaemic heart disease, stroke and peripheral vascular disease. The premature morbidity, mortality, reduced life expectancy and financial and other costs of diabetes make it an important public health condition.1 Type-2 diabetes accounts for over 95% of all diabetics in India. Due to its insidious onset and lack of alarming symptoms, the disease often remains undiagnosed for many years. Type-2 diabetes mellitus has significant relationship with obesity and almost 90% type-2 diabetics are obese although only a minority of obese people are diabetic. Dyslipidemia is observed in practically all patients of type-2 diabetes mellitus and very high level of cholesterol in diabetics have 2-3 times higher AMI risk than non-diabetic individuals. 1 Cardiac involvement in diabetes commonly manifests as AMI and less commonly as dilated (diabetic) cardiomyopathy and autonomic cardiovascular neuropathy. 2 Although coronary artery disease (AMI) and diabetes mellitus have been recognized as distinct entities for many decades, but their correlation was established only in 1870 after the work of Seegen.J. Der. Who emphasized higher incidence and mortality of AMI among diabetics. 3 The Framinghan heart study assessed that patient with diabetes, particularly women exhibited an increased risk in coronary events including angina, stroke, claudication, heart failure, myocardial infarction, and sudden death. The prevalence of AMI in Indians is higher than in any other population in the world. In the recent past, the prevalence has risen from 1.5-6.5% to 8-12%. There is difference in the prevalence of AMI in urban and rural India (8-9.6% to 3.5%) more common in south than north India. The incidence of AMI in diabetic men is twice and four times more common in diabetic woman. The risk of AMI among diabetic patients is directly related to the levels of blood pressure, cigarette smoking and total cholesterol. 4,5 The Framingham study showed that the risk of cardiovascular death was increased 4-5 fold in women and 2 fold in men with predominantly type-2 diabetes mellitus. 75 to 80% of adult diabetic patients die from coronary artery disease, cerebrovascular accidents and or peripheral vascular disease. 6 Coronary artery disease mortality is higher amongst Indian Asians than in other ethnic groups. It was predicted that cardiovascular mortality will rise by 100% in India by the year 2015. 7 New risk factors for AMI among diabetics viz microalbuminuria, PAI – 1 And hyper-(pro)-Insulinaemia have appeared, which have to be kept in mind while treating AMI because PAI–1 may pose resistance to thrombolysis. Type-2 diabetes mellitus is the commonest type of diabetes in India. It gives rise to numerous complications, out of which coronary artery disease is important one, which is the leading cause of death in diabetes. As the trends keep on changing from time to time with respect to geographic region. Present study was undertaken to compare the complications and mortality in acute myocardial infarction among diabetic and non diabetic patients. Aim and objective: To compare the complications and mortality in acute myocardial infarction among diabetic and non diabetic patients
MATERIAL AND METHODS Present study was a cross sectional study carried out at a tertiary health care centre during January 2018 to September 2019. Study population was adult patients admitted with Acute myocardial Infarction. Inclusion criteria: 1. Patients with age more than 12 years. 2. Patients with diabetes as cases and non diabetic patients as control group 3. Patients willing to participate in the study Exclusion criteria: 1. Patients with age above 12 years 2. Patients having impaired Fasting Glucose [FPG < 126mg/dl. But > 110 mg/dl, PP-PG 140 –200mg/dl] Study was approved by ethical committee of the institute. A valid written consent was taken after explaining study to them. 120 cases of AMI were studied, out of which 60 cases are diabetic AMI (Group 1) and 60 cases are nondiabetic AMI (group 2). Sample is drawn by simple random technique. Previously known diabetic or first time detected diabetic by American diabetic association (ADA) criteria, 2018, presenting with AMI were included in group 1 and Cases presenting with myocardial infarction who are not known diabetics or not fulfilling ADA were included in group 2. Data was collected with pre tested questionnaire. After fulfilling the inclusion and exclusion criteria patients were recruited. Detailed clinical history was noted. History included duration and control of diabetes, presence of risk factors like smoking, hypertension, and family history of IHD. If any complications of hypertension or diabetes in past it was noted. A through clinical examination was done. Vital signs like pulse (rhythm disturbance) BP (look for hypertension/ hypotension) were noted. Routine investigations like Routine blood and urine RBS, FBS and PPBS And Glycosylated Hb was done. Lipid profile, renal function tests, fundus examination was done. Patients were stabilised by medical management. Complications observed were Pump failure (LVF ± Cardiogenic shock), Rhythm disturbances (Ventricular / atrial) and Co-morbid complication (e.g. Stroke). Outcome in both the group was compared in terms of complications and mortality. Data was entered in excel sheet. Data was analysed with SPSS version 22.
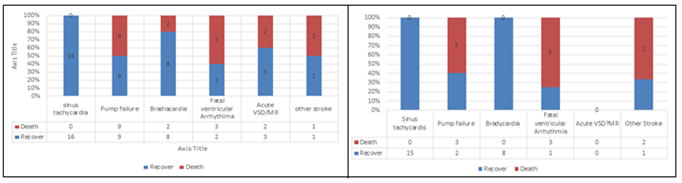
RESULTS The study consists of two groups i.e., Diabetic AMI (group-1) and Non-diabetic AMI (group2). Group-1 consists of 60 cases (42 males and 18 females) and group-2 consists of 60 cases (44 males and 16 females). From table 1 we can say that most of the patients in both group diabetic and nondiabetic belongs to age group 45 – 54 so Age difference between two groups and within groups among sex wise, t-test shows insignificant p >0.05. Male to female ratio in group-1 was 2.3:1 and in group-2 it was 2.75:1. Females were commonly affected in the diabetic group than non-diabetic group (p<0.01). Only 4 premenopausal women had AMI among diabetic group whereas none were in premenopausal group among non-diabetics. (table 1) Among the established diabetics, mean duration of diabetes was 5.01±3.8 years (1 SD). For males mean duration of diabetes was 4.91±3.9 years (1 SD) and for female it was 5.11±3.2 years (1 SD). The association between Males and Females in relation to duration of diabetis among established diabetic is insignificant (P > 0.05) Among diabetics, 61.11% of females were hypertensive and 40.40% of males were hypertensive by history. Among non-diabetics 15.9% of males were hypertensive and 43.75% of females were hypertensive. Among diabetic 28 (46.67%) were hypertensive and among non-diabetic 14 (23.34%) were hypertensive. In our study, central obesity was present in 38 (90.48%) of males and 16 (88.88%) of females in diabetic group and 40 (90.9%) of males and 14 (87.5%) of females in non diabetic group. Most common presentation is chest pain in both groups ( D 70 % and ND 85 % ). Most of the patients in diabetic group presented with chest pain with sweating and with symptoms of sympathetic stimulation (vomiting/ apprehension 70%). A small fraction of diabetic patients presented with breathlessness – 20%, syncope (3.33%) and palpitation (8.3%). Maximum number of cases of Stable angina belonged to Non-Diabetic group (66.66%) and Unstable angina and MI belonged to Diabetic group (28.34% and16.66%) respectively. There was a significant association between types of AMI among the diabetic and the non-diabetic groups (P<0.001). (table 3) Diabetics are more vulnerable to mortality than non-diabetics (p<0.05). Totally, 17 cases in diabetic group (28.33%) and 8 (13.33%) patients in non-diabetic group have expired. In diabetic group the main cause of mortality was pump failure 9 (50%) and in non-diabetic group pump failure and fatal ventricular arrhythmia was the main cause for mortality 6 (75%). Table 4 shows complications in diabetic and non diabetic patients. Among the diabetic patients total 54 (90%) patients had complications. In the non diabetic patients complications were observed in 35 (58.33%) . Pump failure 18 (30%) was most common complication followed by sinus tachycardia (26.67%)in diabetic patients. among the non diabetic patients, sinus tachycardia (25%) was most commonly observed followed by bradycardia (13.33%). There was a significant association between diabeties and complications (p<0.05)
Table 1: Distribution of diabetic and non diabetic patients according to age and sex
Table 2: Random blood sugar levels according to diabetic status and sex
Table 3: Distribution of patients according to type of CAD
Figure 1: Post MI complications in diabetic patients Figure 2: Post MI Complications In non Diabetic Patients Table 4: Post MI complications and death in diabetic and non diabetic patients
DISCUSSION Age difference between two groups and within groups among sex wise and list shows insignificance (P>0.05). Singer de 3 noted that, diabetic were older, Malmberg et al. 8 noted the same results and noted that females are commonly involved, which is also seen in our study. When age wise cut-off is seen, maximum events occurred in 50-59 years in both diabetics and non- diabetics. Hence, age is an important risk factor for CHD in non-diabetic and diabetic population. In the GUSTO-1 trial 9, when diabetics were considered, it was seen that, diabetic MI patients were older compared to non diabetic MI‘s. But such results were not obtained in our study. GUSTO-1 trial says that females are commonly involved in diabetic group, which was consistent with our results. Chest pain was commonly found among Non-diabetic (85 %) and diabetics (70 %) and , 5% of patients in diabetic group had pain in abdomen, 2/3rd of which never had associated chest Pain and 5% had only breathlessness and 6.66% had only sweating. In the acute myocardial infarction framingham study 10, noted that Half of patients had atypical symptoms and half of them were not having any symptoms at all (actually / truly silent). Soler et al. found that 33% of diabetics had atypical features and presented with heart failure, hyperglycemia, vomiting, collapse, confusion or CVA. 11 In our study maximum number of cases of stable angina belonged to non-diabetic group (66.66%) and unstable angina and mi belonged to diabetic group (28.34% and16.66%) respectively. Hong et al.. 12 reported similar results that is acute coronary syndrome that is unstable angina and myocardial infarction is more common in diabetic than non- diabetics. In our study, among diabetic group 33 (55%) of the people were current smokers/toabcco chewers, 27 (45%) were non-smokers. Among non diabetics such figures were 35 (58.3%) and 25 (41.7%) respectively. In GUSTO-1 trial 9, 45% were current smokers, 26% were former smoker and 29% were never smoker among non diabetics. Among diabetics, the same percentage was 31, 31 and 38 respectively. Hence, smoking is less commonly seen with diabetics. In the UKPDS, who participated in the trial, the same proportion was 32%, 46%, 22% in men and 29%, 27% and 44% among women. 13 In our study, Mean BMI for diabetics was higher than non diabetics 24.61 ± 3.1 and 22.31 ± 2.51 and the association is statistically significant (p<0.001). In the Rancho Bernardo study 14, though BMI was high among diabetics, males commonly had higher BMI than females unlike our study. When we consider the difference between the mean systolic and diastolic BP among 2 groups, we see that, systolic BP was higher among diabetics (p<0.01) and diastolic BP was also higher DM group (p<0.05). Same findings were seen among males and females. In the GUSTO-1 trial 9 who have shown that systolic BP was higher among diabetics (p<0.001) and diastolic BP was equal (p=0.07) in two groups. From our study we can conclude that there is a significant association between diabeties and complications. Most common complication in DM is pump failure and in NDM patients sinus tachycardia is most common. The FAST-MI (French registry of Acute ST elevation or non-ST-elevation Myocardial Infarction) registry showed that 37.5% of AMI patients had HF; these patients, compared with MI patients without HF, had a significantly increased risk of death during index hospitalization (12.2% vs. 3.0%). 15 In our study we noted 17 (28.33%) mortality among diabetics compared to 8 (13.33%) among non diabetics. The association was found to be statistically significant (p<0.05).Pump failure is an important cause of death and is commonly seen in males. Studies both in pre-thrombolytic and thrombolytic era, have proved that, pump failure is an important cause of mortality and is especially higher in women. Such pump failure is even commonly seen with smaller infarcts and similar as in non diabetics thus underlines the importance of diabetic cardiomyopathy reducing the myocardial reserve and causing LVF. In the Multiple Risk Factor Intervention Trial (MRFIT), men with diabetes had a threefold higher absolute risk of cardiovascular death than non‐diabetic men (160 vs 53 cardiovascular deaths per 10 000 person‐years) even after controlling for age, race, income, cholesterol levels, blood pressure and smoking. 16 The Framingham Study 20‐year follow‐up similarly demonstrated that patients with diabetes not only had a higher mortality with their index event, they also had a higher incidence of re infarction and heart failure in the acute and post infarction periods.17 The FINMONICA Study, which looked at out‐of‐hospital deaths as well as deaths from index admission, showed that while diabetic women have a higher in‐hospital and 1‐year mortality, diabetic men have a higher overall mortality due to out‐of‐hospital death. 18
CONCLUSION Post MI complications and Mortality is significantly more among diabetics compared to among non diabetics.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home