|
Table of Content Volume 16 Issue 2 - November 2020
The accuracy of ultrasonography in confirming endotracheal tube placement in emergency department
B Gnanendra Prasad1, Deepali Rajpal2*, Manhar Shah3, Manu Mathew4, Mayank Chaurasiya5
1,5Resident, 2Professor, 3Professor & HOD, 4Assistant Professor, Department of Emergency Medicine, D.Y. Patil School of Medicine, Navi-Mumbai, Sector 5, Nerul, Navi Mumbai 400 706 Email: deepalioncall77@gmail.com
Abstract Background: Over the past few years, ultrasonography is increasingly being used to confirm the correct placement of endotracheal tube (ETT). In our study, we aimed to compare it with the traditional clinical methods and the gold standard quantitative waveform capnography. Two primary outcomes were measured in our study. First was the sensitivity and specificity of ultrasonography against the other two methods to confirm endotracheal intubation. The second primary outcome assessed was the time taken for each method to confirm tube placement in an emergency setting. Methods: This is a single ‑ centered, prospective cohort study conducted in an emergency department of a tertiary care hospital. We included 250 patients with indication of emergency intubation by convenient sampling. The intubation was performed as per standard hospital protocol. As part of the study protocol, ultrasonography was used to identify ETT placement simultaneously with the intubation procedure along with quantitative waveform capnography (end‑tidal carbon dioxide) and clinical methods. Result: Out of the 250 intubation attempts, the overall accuracy of ultrasonography was 98.80% .The sensitivity ,specificity, positive predictive value and negative predictive value of ultrasonography method for tracheal intubation confirmation were 98.72% 100%,100%,84.21% respectively. If ultrasonography is as specific and sensitive as wave form capnography It can be used instead if wave form capnography is not available. Conclusion: Ultrasonography confirmed tube placement with comparable sensitivity and specificity to quantitative waveform capnography and clinical methods. Key Word: Capnography, emergency, intubation, ultrasonography.
INTRODUCTION Airway management skills are indispensable for an emergency physician. Unrecognized airway accidents such as esophageal intubation is a source of morbidity and mortality, tend to occur more in emergency settings,1 where it is reported as 8%.2 Numerous studies have compared methods used for distinguishing between endotracheal and esophageal placement of the tube. Visual confirmation during laryngoscopy, expansion of the chest wall during ventilation, auscultatory method, capnography, and chest X‑ray are modalities currently used in practice. These techniques vary in their degree of accuracy.3‑6 The Advanced Cardiac Life Support (ACLS) 2015 guidelines recommend continuous waveform capnography in addition to clinical assessment as the most reliable method of confirming and monitoring correct placement of an endotracheal tube (ETT).7 In 1989, in a study, Vaghadia et al. came to a conclusion that end‑tidal carbon dioxide (ETCO2 ) is most accurate for identifying esophageal intubation.8 Capnography has also been found to be the best method for rapid assessment of tube position. Ultrasound, once the domain of the radiologist, has now found its place in pre- hospital applications (e.g, emergency responders), emergency wards, intensive care units, and operation theatres. Portable ultrasound is easy to carry. noninvasive, relatively economical, easily reproducible, and widely available, and it has a good safety record. It is noninvasive, occurs in real time and thus improves the confidence of the physician in determining tube placement. Tracheal ultrasonography images are not affected by very low pulmonary flow, contrary to capnography, and ultrasonographic detection of esophageal intubation can be performed prior to ventilation of the patient. Earlier detection of esophageal intubation could the stomach and its associated complications, namely prevent ventilation of the stomach and its associated complications, namely emesis and aspiration. In this study, we evaluate the sensitivity and specificity of transtracheal ultrasound as compare to traditional methods in confirming endotracheal tube placement in emergency department.
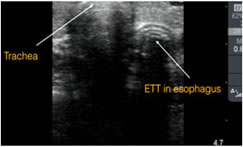
METHODS SOURCE OF STUDY: this study was conducted on adult patients who underwent emergency intubation because of impending respiratory failure, cardiac arrest, or severe trauma. two fifty patients presented to ED with an indication for endotracheal intubation were recruited into this study. Tracheal sonography was performed using a SonoSite M‑Turbo linear probe (13‑6 MHz). A Philips M‑20 monitor with a mainstream ETCO2 analyzer was used for capnography. In this study we excluded patients less than 18 years and patients with severe neck trauma and neck tumours. Method of confirmation of endotracheal tube placement Procedure: As per inclusion and exclusion criteria patients were recruited into the study (one for intubation and direct visualization and second for 5 point auscultation) senior resident or faculty of emergency medicine department (look for rise oxygen saturation by pulse oxymetry and condensation in the endotracheal tube)] were required for this study and everyone record their findings and time using a stopwatch. The operating time required for intubation and ultrasound confirmation was recorded. The intubation time was defined as the time from pre oxygenation with a bag-valve-mask to completion of endotracheal tube insertion. The ultrasound operating time was defined as the time from completion of endotracheal tube insertion to when the sonographer had interpreted the sonographic results. Simultaneously by pulse oxymetry (rise in oxygen saturation) and 5 point auscultation done and separate time and findings were recorded. Time for direct visualization defined as the time from stopping of bag-valve-mask pre oxygention to successful placement of endotracheal tube under direct visualization. Portable X-ray of the chest was done after repositioning of endotracheal tube whenever it was found in oesophagus by other confirmatory Method of ultrasonographic confirmation: Figure 1: Tracheal intubation if only one air-mucosal (A-M) interface with reverberation artifact and posterior shadowing was observed and Esophageal intubation if two A-M interfaces posterior shadowing were noted, which is called a double tract sign.
Figure 2:
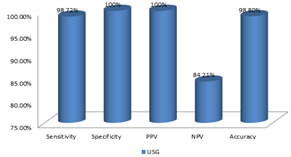
Table 1: Sensitivity, Specificity, Positive predictive value, Negative predictive value and Accuracy of Ultrasound for tracheal intubation confirmation
Sensitivity, Specificity, Positive predictive value, Negative predictive value and Accuracy of Ultrasound for tracheal intubation confirmation
Figure 3:
The overall accuracy of ultrasonography method was 98.80% (95% confidence interval (CI) 96.53% to 99.75%). The Sensitivity, Specificity, Positive predictive value and Negative predictive value of ultrasonography method for tracheal intubation confirmation were 98.72% (95% CI 96.30% to 99.73%), 100% (95% CI 79.41% to 100%), 100 % and 84.21% (95%CI 63.41% to 94.26%) respectively. The likelyhood ratio of a positive test was Infinite and the likelyhood ratio of a negative test was 0.01(95% CI 0.00 to 0.04)
DISCUSSION This prospective study aimed to assess accuracy and timeliness of tracheal ultrasound for determining endotracheal tube placement during emergency intubation. In this study, tracheal ultrasound achieved high sensitivity and specificity for confirming endotracheal tube placement. Therefore, ultrasound can serve as a good diagnostic tool for confirming tracheal intubation during resuscitation. However, each confirmation technique has its own limitations. Capnography is the currently accepted criterion standard for tracheal intubation confirmation. According to the new ACLS guidelines, quantitative waveform capnography is recommended as the most reliable method for confirming endotracheal tube placement. Nevertheless, quantitative capnography is neither widely available nor consistently applied in some of EDs. In a survey of the National Emergency Airway Registry Series, a total of 77% of physicians reported that colorimetric end-tidal CO2 detectors were available in their hospitals, but only 25% of respondents used continuous quantitative capnography. 94) Base on these results, the EDs and ICUS should be appropriately equipped with capnography. Besides that, another confirmation technique with high accuracy is desirable if capnography is not available. Ultrasound is a common and useful diagnostic tool in many EDs and critical care areas. The use of ultrasound to confirm endotracheal tube placement is attractive due to the following reasons. First, ultrasound is portable, repeatable, and widely available in many EDs, critical care areas, and even outside of the hospital. If ultrasound is as sensitive and specific as the waveform capnography, it can be used instead if waveform capnography is not available. Second, ultrasonographic images are not affected by low pulmonary flow, as compared to capnography. Third, tracheal ultrasound can detect esophageal intubation even before ventilating the patient, which prevents unnecessary forced ventilation to the stomach and its associated complications. Several previous studies have provided promising results of tracheal ultrasound for endotracheal tube placement confirmation. Ma et al... used the transcricothyroid ultrasound to confirm tracheal intubation in the cadaveric model, and demonstrated high sensitivity and specificity. 95) Two prospective studies showed up to. 100% of sensitivity and specificity of tracheal ultrasound in live humans under a well-controlled operating room setting. 96.97) In a recent study performed on 30 ED patients, high sensitivity and specificity values were reported using combined ultrasonographic methods.081 In this study we compared different methods of endotracheal tube confirmation. Each method have their disadvantages. In Direct visualization method 24 patients (10%). had difficulty in visualization of vocal cord. Out of 44 patients of trauma there were 26 patients with severe faciomaxillary injury. Out of these 26, 18 patients had difficulty in visualization of vocal cord due to distorded anatomy. Another 6 patients had difficulty in
CONCLUSION Ultrasonography detected the tube placement faster and accurately than the other methods. The time difference is statistically significant, and, considering that the scenario is time critical, it has significant clinical importance. Present study demonstrated that transtracheal sonography has an acceptable degree of sensitivity and specificity for the confirmation of endotracheal intubation. Ultrasonography is a valuable adjunct and should be considered when capnography is unavailable or unreliable. As a result, the 2015 advanced cardiac life support guidelines suggested that ultrasonography may be a useful alternative to quantitative waveform capnography, which is further supported by this study. Moreover, most confirmatory methods require multiple ventilations, which may increase the risk of gastric distention and aspiration if the endotracheal tube is incorrectly placed. Ultrasonography offers the advantages of being rapid, easily available, and non invasive, and does not require ventilations to confirm placement. REFERENCE
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||
 Home
Home