|
Table of Content Volume 16 Issue 3 - December 2020
A clinical study of alopecia areata and it’s dermatoscopic correlation in a tertiary care hospital
K Sumohita1*, M Madhavi Latha2, T Praveena3
1Post graduate, 2Professor, 3Associate Professor, Department of DVL, Santhiram Medical college and General Hospital, NH-40, Nandhyal, Andhra Pradesh, INDIA. Email: sumohita88@gmail.com Abstract Background: Alopecia Areata (AA) is a common, chronic autoimmune disease causing non- scarring hair loss of scalp and body hairs. The course of the disease is unpredictable that results in a severe psychological impact on the people. Aims and objectives: To study clinical patterns of Alopecia areata and it’s association with other diseases.To study the dermatoscopy findings of AA. Materials and methods: The study was conducted in 50 people of both sexes between ages (1-50yrs) with Alopecia Areata attending the department of DVL at Santhiram medical college and general hospital for 6 months. The patient's data was recorded in a prestructured proforma that includes clinical history, general and cutaneous examination, investigations and dermatoscopy. Results: Out of 50 people(29 males, 21 females). Common age group affected was 10-20yrs.Scalp involvement in 80% cases with (patchy alopecia 80%, ophiasis 15%, diffuse 5%).beard in 10%, eyebrows and eyelashes in 8%, body hair in 4%. Nail changes in AA were Pitting seen in 8% cases and longitudinal ridging in 6% cases. No nail changes in 86% cases. Alopecia areata was associated with atopy in 48%, hypothyroidism in 18%, vitiligo in 4%, AA was not associated with other diseases in 30%. Dermatoscopy findings were yellow dots in 45%, black dots in 32%, exclamatory mark 30%, white dots in 10% broken hairs in 15%, bent hair in 5% vellus hair in 2% Conclusion: Scalp was the most common site affected with the patchy type being a most common pattern. Alopecia areata was commonly associated with atopic dermatitis. The most common Dermatoscopy features were yellow dots(YD), black dots(BD), and exclamatory marks. Key words: Alopecia areata(AA), Black dots(BD), Yellow dots(YD)
INTRODUCTION Alopecia areata (AA) is a common, chronic inflammatory disease that causes non- scarring hair loss1 It affects 1% of the general population although the pathogenesis of alopecia areata is still not completely understood, genetic environmental and autoimmune factors are considered to play a role in it’s etiology.1 Alopecia areata is a T cell-mediated organ-specific autoimmune disease and is associated with various autoimmune disorders such as vitiligo, atopy, Hashimoto's thyroiditis, diabetes mellitus, psoriasis, celiac disease, and lupus erythematosus.1 The characteristic initial lesion of alopecia areata is a circumscribed, hairless, smooth patch.1 Short, easily extractable broken hairs, known as exclamation mark hairs, are often seen at the margins of the bald patches during active phases of the disease.1.The incidence of Alopecia areata is 0.1-0.2%.1 Shuster described the “coudability” sign to differentiate diffuse AA from other alopecias, in AA normal looking hair kinks when forced inwards2 Histopathology -The swarm of bees appearance due to dense peribulbar lymphocytic infiltrate characterizes the acute phase of A.A.2 On Dermatoscopy, active disease is characterized by yellow dots, black dots, "exclamation mark" or tapering hairs, and broken hairs. Vellus hair in lesions is another marker of AA and may indicate late or inactive disease3,4.
AIMS AND OBJECTIVE: Aims and objectives: To study clinical patterns of Alopecia areata and it’s association with other diseases. To study the dermatoscopy findings of AA.
PATIENTS AND METHODS The study group includes 50 patients of both sexes between ages 1-50 yrs with alopecia areata attending to the department of DVL OPD in Santhiram medical college and general hospital, Nandyal during the period from september 2019 to February 2020. All patients of ages 1-50yrs of both sexes with the clinical diagnosis of alopecia areata willing to give informed written consent were included in the study. Patients who are not willing to give informed consent and patients of alopecia areata already on treatment were excluded. Approval for the study was taken from the Institutional ethical committee. Written informed consent was taken from patients. A detailed history and clinical examination findings were recorded as per the pre-structured proforma. Clinical photographs and dermatoscopy images were taken The skin, hair, nails, and mucosa were examined in detail. Relevant investigations were done.
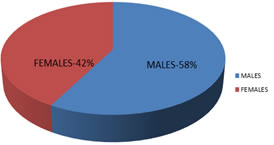
RESULTS The Study population includes 50 cases of Alopecia areata(AA) Out of 50 cases 58% were males, 42% were females. Male to female ratio was 1.38:1, AA according to age in age groups 1-10yrs was 32%,11-20yrs was 36%, 21-30yrs was 16%,31-40yrs was 12%,41-50yrs was 2% . AA was common in age groups(11-20yrs). The most common site of AA was Scalp 80%, Most common type in scalp AA was patchy alopecia ( 80%). Ophiasis was seen in 15%, and diffuse alopecia areata in5%. Other sites involved in Alopecia areata were beard in 10%, eyebrows, and eyelashes in 4% body hair in 2%. Alopecia totalis was 2%, alopecia Universalis was 2%. Nail changes in Alopecia areata were Pitting seen in 8% cases and longitudinal ridging in 6% cases, no nail changes in 86% cases. Alopecia areata was associated with atopy in 48%, Hypothyroidism in 18%, and vitiligo in 4%, AA was not associated with other diseases in 30%. Dermatoscopy findings were yellow dots in 46%, black dots in 32%, exclamatory mark in 30%, white dots in 10 broken hairs in 16%, bent hair in 3% vellus hair in 2%.
Graph 1: Male and female distribution
Table 1: Distribution of cases according to Age and sex
Table 2: Site of distribution of Alopecia areata
Table 3: Pattern of distribution of AA on scalp( out of 40)
Graph 2: Nail changes in AA
Table 4: Associated diseases with AA
Table 5: Dermatoscopy changes in AA
Clinical photographs Figure 1: Patchtype of alopecia areata Figure 2: Patch type of AA Figure 3: Ophiasis Figure 4: Alopecia areata involving occipital area Figure 5: Alopecia totalis
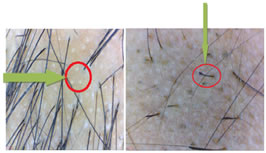
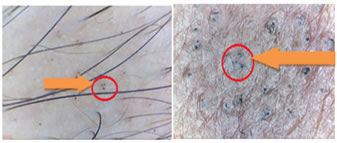
DERMATOSCOPY IMAGES Figure 6: White dots; Figure 7: Exclamatory mark sign Figure 8: Broke hair Figure 9: Hidden hair
DISCUSSION Alopecia areata is a common chronic inflammatory disease causing non- scarring form of hair loss. AA affects both sexes equally though in some studies there was a preponderance for males. Our study included 50 patients of alopecia areata of both sexes of which 58% were males and 42% were females. The male to female ratio was 1.38:1. This was similar to the study reported by Arun Achar et al.l, where males and females affected were(50.24% and 49.8%, respectively)5. In a study conducted by Sharma et al., there was a slightly higher incidence among males. The age of participants in our study ranged from 5-50yrs. The most common age group affected was 11-20yrs ( 36%) which was similar to a study done by Wasserman et al.;6 in which more cases of AA were seen before 20 years of age. The most common site of AA in our study was Scalp 84% (patchy alopecia 80%, ophiasis 15%, diffuse 5%), other sites involved in AA were beard 10%, eyebrows and eyelashes 4%,body hair 2%. Alopecia totalis was seen in 2%, Alopecia Universalis is 2%. The scalp was the most common site affected in AA (90%) which was similar to study conducted by Tan et al.., 2002,7. In Bapu et al..'s study,8 patchy (65.5%), ophiasis (4.31%) types were most commonly seen. Nail changes in our study were Pitting seen in 8% cases and longitudinal ridging seen in 6% cases, no nail changes in 86% cases. Gandhi et al. reported superficial pits as the commonest change 9. Nail changes were described in 7% to 66% of AA patients with nail pitting the common type.10 The association of Alopecia areata with atopic dermatitis was 48%, A study conducted by S Sukhjot et al.;11 has reported that 50%cases of AA had Atopy, similar to our study. Hypothyroidism was 18% in our study which was similar to Ola A Bakry et al. study 12 where hypothyroidism was seen in 16% of cases. AA with vitiligo was 4% in our study which was similar to a study conducted by Jesy Ragavan et al.,13 were vitiligo was noted in 5% subjects suggesting an association between AA and vitiligo. AA in 30% of cases was not associated with any disease. Dermatoscopy findings in our study include yellow dots in 46%, black dots in 32%, exclamatory mark in 30%, white dots in 10%, broken hairs in 16%, bent hair in 3% vellus hair in 2% of patients, in contrast, to study conducted by Balachandar et al.14 that showed yellow dots(50%), exclamation mark hairs(60%), broken hairs, (30%)black dots(20%), short vellus hairs in (10%).
CONCLUSION Alopecia areata is a chronic autoimmune T-cell disorder of the hair follicle. The peak incidence of AA in our study was 11-20yrs. The scalp was the commonest site affected. Patchy type was the commonest pattern. Pitting of nails was the most common nail change. Alopecia areata was commonly associated with atopic dermatitis. Most common dermatoscopic finding was yellow dots. Other common dermatoscopic findings were black dots, exclamatory marks and broken hair.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home