|
Table of Content Volume 17 Issue 2 - February 2021
Clinical and haematological profile of sickle cell disease in rural area of western ghats of India
Rajeev Wadekar
Assistant Professor, Department of Internal Medicine, Vedanta Institute of Medical Sciences, Sasvand, Dahanu, Palghar, Maharashtra, INDIA.
Abstract Background: Sickle cell disease or sickle cell anemia is a hereditary genetic disease that is characterized by the presence of abnormal crescent-shaped red blood cells. Haematological profile of SCD patient is helpful for treatment and prognosis. Aim and objective: To study the clinical and hematlogical profile of sickle cell disease in rural area Methodology: Present study was prospective study conducted on patients diagnosed with sickle cell disease at a tertiary health care centre in Western Ghats of India. Data collected was sociodemographic data, clinical history and clinical examination. Hematological indices nHB%, HCT, PLATELET, MCV, MCH, MCHC were measured by complete blood count on auto analyser. Data was analysed with appropriate statistical tests. Results: Majority of the patients were in the age group of 21-30 years (35.71%) followed by 31-40 years (32.86%). Male to female ratio was 2.18: 1. Most commonly observed symptom was pain 43(61.43%) followed by Fever 25 (35.71%). Total hemoglobin is low (8.2±1.8g/dl). Mean MCV in males was 85.13±7.2 fl, while it was 81.4±10.2 fl in females. Mean MCH in all patients was 26.3±4.1 pg. Mean MCHC in males and females were 31.75±3.9g/dl and 31.5±3.86 g/dl respectively. Mean HbF in patients was 18.3±5.3%. Mean HbA2 values in males was 2.3±0.21 % and in females it was 2.7±0.8 %.
INTRODUCTION Sickle cell disease is an autosomal recessive genetic blood disease. It is one of the significant public health problem in India. Highly prevalent areas in India are Western, Central, and Eastern regions and in pockets of the South in the states of Maharashtra, Madhya Pradesh, Orissa, Andhra Pradesh, Gujarat, Chattisgarh, Tamil Nadu, and Kerala. 1-5 SCD is characterized by the presence of HbS, caused by a single point mutation involving GAG GTG transversion at codon 6 of the β-globin gene. 6,7 This results in an amino acid substitution at position 6 in the β-globin chain from glutamic acid to valine on the surface of the hemoglobin molecule. This change leads to formation of less soluble HbS than HbA.6 Polymerization of HbS results in the formation of elongated rigid fibers that damage the cytoskeleton of the red blood cell, causing the shape of the cell to change from the smooth, doughnut-shape to the sickle-shape. 8,9 Clinical features of the sickle cell disease starts in early life and their incidence increases as the age increases due to decline of HbF. Patients of sickle cell disease presents with vaso-occlusive pain crises, risk for pneumococcal infections, acute chest syndrome, stroke and organ failure. It is associated with significant morbidity and premature mortality. 3 Haematological profile of the patients with sickle cell disease shows changes in RBC morphology and count. Hematological profile of SCD is extremely variable. Various studies shown different results so present study was conducted to study the clinical and haematological profile of patients with sickle cell disease. Aim and objective: To study the clinical and hematlogical profile of sickle cell disease in rural area MATERIAL AND METHODS Present study was conducted in Department of Medicine at a tertiary health care centre in Western Ghats of India. Study population was patients diagnosed with sickle cell disease and attending Out patient Department or admitted in department of Medicine. Inclusion criteria:
Exclusion criteria:
Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. Data was collected with pre tested questionnaire. Data included sociodemographic data like age, sex etc. Detailed clinical history was noted. through clinical examination was done. 5 ml venous blood was collected in ethylene diamine tetraacetic acid (EDTA) bulb from all patients. Hematological indices HB%, HCT, PLATELET, MCV, MCH, RDW, MPV were measured by complete blood count on auto analyser. Quantitative assessment of HbS and HbF was done by high performance liquid chromatography (HPLC) technique. Data was entered in Excel sheet. Data was analysed with SPSS version 20.
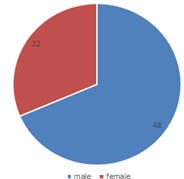
RESULTS After considering inclusion and exclusion criteria we studied 70 patients diagnosed with sickle cell disease. In our study age distribution of these patients is mentioned in table 1. Majority of the patients were in the age group of 21-30 years (35.71%) followed by 31-40 years (32.86%). Patients in age group of 12-20 years were 30%. Only one patient was seen in age group of 41-50 years. None of the patient was above 50 years. Fig 1 shows distribution of the patients according to sex. Out of 70 patients 48 (68.57%) were male and (31.43%) were females. Male to female ratio was 2.18: 1. Table 2 shows clinical profile of the sickle cell disease patients. Most commonly observed symptom was pain 43(61.43%). Among all the patients with pain, most commonly observed pain was musculoskeletal pain 18(41.86%). Abdominal pain was observed in 15(34.88%) patients. generalised body ache and chest pain was complained by 16.28% and 6.98% patients respectively. Fever was seen in 25 patients contributing to 35.71% of the patients. Other symptoms observed were vomiting and diarrhoea (21.43%) and cough (11.42%). Pallor was the most commonly 29(41.43%) observed sign followed by splenomegaly (25.71%). Icterus and hepatomegaly were observed in 12.86% and 10 % patients respectively. In our study most common cause for hospitalization was severe anaemia requiring blood transfusion 32(45.71%) followed by respiratory infections 24 (34.28%) and gastrointestional infections 19 (27.14%). Some patients also admitted for urinary tract infections and malaria. Table 3 shows haematological profile of sickle cell disease patients. Total hemoglobin is low (8.2±1.8g/dl), in male patients it was 8.3±2.1g/dl and in females it was 7.9±1.9 g/dl the difference was not statistically significant (p>0.05). In our study RBC count in males was 2.95±0.85 million/mm3, while in females it was 2.94±0.7 million/mm3 . Total Hct was 25.4±5.3, it was 25.3±5.7in males and 25.6±4.9 in females. Mean MCV in males was 85.13±7.2 fl, while it was 81.4±10.2 fl in females, difference in male and females was insignificant, (p>0.05). Mean MCH in all patients was 26.3±4.1 pg. Mean MCH was more in male patients (27.43±4.1pg) than females (25.65±4.3 pg) but the difference was statistically not significant. Mean MCHC in males and females were 31.75±3.9g/dl and 31.5±3.86 g/dl respectively. The difference between them was statistically not significant. Mean HbF in patients was 18.3±5.3%. In males it was 19.2±4.92 % and in females it was 17.81±5.9 %. Mean HbA2 values in males was 2.3±0.21 % and in females it was 2.7±0.8 %. The difference between mean HbF and HbA2 among male and female was statistically not significant (p>0.05).
Table1: distribution of sickle cell disease patients according to age group
Figure 1: Distribution of sickle cell patients according to sex
Table 2: Distribution of sickle cell disease according to clinical features
Table 3: Haematological profile of sickle cell disease patients
P value>0.05: statistically not significant
DISCUSSION In our study, Majority of the patients were in the age group of 21-30 years (35.71%) followed by 31-40 years (32.86%). Lesser patients were observed above the age of 40 years. Previous studies also reported majority patients in the younger age group. 10 In our study male outnumbered female patients. Male to female ratio was 2.18: 1. In a study by Chavda J.et al.11 male: female ratio was 2:1. Another study by Deore et al. found 27 males and 19 females out of total 46 patients. 12 similar results were seen in previous studies. 13,14 Gender bias and female child discrimination in our society may be the reason for male predominance in the study. In our study, Most commonly observed symptom was pain 43(61.43%). Among all the patients with pain, most commonly observed pain was musculoskeletal pain 18(41.86%). Abdominal pain was observed in 15(34.88%) patients. generalised body ache and chest pain was complained by 16.28% and 6.98% patients respectively. Our results are in accordance with Subhramanyam et al. where musculoskeletal pain was observed in 64%, abdominal pain and chest pain were observed in 35% and 7% of cases respectively. 15 Similar results were seen in a study by Kinjal G. Patel et al. where musculoskeletal pain in 40.54%, abdominal pain in 37.83%, generalized body ache in 18.91% and chest pain in 2.7% of cases was observed. 16 Fever was seen in 25 patients contributing to 35.71% of the patients. Other symptoms observed were vomiting and diarrhoea (21.43%) and cough (11.42%). Pallor was the most commonly 29(41.43%) observed sign followed by splenomegaly (25.71%). Icterus and hepatomegaly were observed in 12.86% and 10 % patients respectively. Similar results were observed in Mandot et al.13 and Kinjal G. Patel et al.16 where splenomegaly was observed more than hepatomegaly. Table 3 shows haematological profile of sickle cell disease patients. mean haemoglobin level is lower in the patients. In male patients it was 8.3±2.1g/dl and in females it was 7.9±1.9 g/dl the difference was not statistically significant (p>0.05). Increased hemolysis and recurrent infections was the cause for lowered haemoglobin level. Lowered Hb levels in females were due to menstruation in females. Similar results were seen in previous records. 17-20 In our study RBC count in males was 2.95±0.85 million/mm3, while in females it was 2.94±0.7 million/mm3. Total Hct was 25.4±5.3, it was 25.3±5.7in males and 25.6±4.9 in females. Lowered RBC count and Total Hematocrit level was observed in Roy B et al.21 and Tshilolo L et al.22 Mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH) and mean corpuscular haemoglobin concentration (MCHC) were low in present study. Above results were in accordance with previous studies. 11,21,22 Mean HbF in patients was 18.3±5.3%. In males it was 19.2±4.92 % and in females it was 17.81±5.9 %. Mean HbA2 values in males was 2.3±0.21 % and in females it was 2.7±0.8 %. These results were in accordance with Rao et al.19 and Jadhav et al.18
CONCLUSION Mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH) and mean corpuscular haemoglobin concentration (MCHC) were low in patients with SCD.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home