|
Table of Content - Volume 1 Issue 2 - February 2016
Doppler echocardiographic assessment of left ventricular diastolic dysfunction in hypertensive cardiomyopathies
Somnath Magdum1*, Vijay Nagaonkar2, Rajendra Bhagwat3, Sachin Patankar4
1,4Associate Professor, 3Professor and HOD, Department of Medicine, Government Medical College, Miraj, Maharashtra, INDIA. 2Assistant Professor, Department of Medicien, Dr D Y Patil Medical College, Kolhapur, Maharashtra, INDIA. Email: somnathmagdum@ymail.com
Abstract Background: Left ventricular hypertrophy confers an increased mortality independent of other cardiovascular risk factors. Echocardiography offers clinicians a quick assessment of changes in LV function resulting from hypertension. The M-mode and two-dimensional (2D) echocardiographic findings of LV mass are more sensitive and specific. In present study, an attempt has been made to assess left ventricular diastolic dysfunction in hypertensive cardiomyopathies with various echocardiographic parameters. Material and Methods: A total of 50 consecutive hypertensive patients with blood pressure (BP) more than 140/90 mm of Hg (JNC VII Stage I and II) at two or more recordings after an initial screening were included in this cross sectional study. Echocardiographic evaluation was done by 2D, M mode and Doppler echocardiographyon GE (Logiq 3) expert model no. AY-15 CUI. Results: Advancing age proved to be an important risk factor for the development of left ventricular diastolic dysfunction in patients of hypertension. The findings on echocardiography correlated well with the clinical condition of patients. Discussion: Echocardiography allows for rapid, noninvasive assessment of LV function in hypertensive patients. It can evaluate morphological and hemodynamic changes acutely and over time. Parameters obtained with echocardiography mayhelp in management and care for patients. Keywords: Left ventricular diastolic dysfunction, hypertensive cardiomyopathies, M-mode, 2D, Dopplerechocardiography.
INTRODUCTION Cardiovascular diseases are associated with considerable morbidity and mortality worldwide, and hypertension is a major risk factor for cardiovascular diseases. The hallmark of hypertensive disease is a gradual increase in left ventricular (LV) mass, resulting in concentric hypertrophy and eventual diastolic dysfunction of the left ventricle secondary to LV stiffness and impaired relaxation. Late stages may be characterized by severe LV systolic dysfunction and dilatation. Left ventricular hypertrophy confers an increased mortality independent of other cardiovascular risk factors1. Recent studies have focused attention on the association of left ventricular hypertrophy with left ventricular diastolic dysfunction as the earliest evidence of impaired left ventricular function in hypertension. Doppler echocardiography has been well established as a simple and reliable noninvasive technique to measure intracardiac blood flow. Recently much attention has been focused on utilizing Doppler echocardiography for assessment of diastolic function in patients with various cardiac disorders2-4. It offers clinicians a quick assessment of changes in LV function resulting from hypertension. The M-mode and two-dimensional (2D) echocardiographic findings of LV mass have been shown to be more sensitive and specific when compared to electrocardiographs (ECG) or chest X-ray in diagnosing LV hypertrophy and concentric remodeling. In present study, an attempt has been made to assess left ventricular diastolic dysfunction in hypertensive cardiomyopathies with various echocardiographic parameters.
MATERIAL AND METHODS A total of 50 consecutive hypertensive patients with blood pressure (BP) more than 140/90 mm of Hg (JNC VII Stage I and II) at two or more recordings after an initial screening were includedin this cross sectional study.The study protocol was approved by the local Ethical Review Committee, and a written informed consent was obtained from all those that participated in the study. The BP were measured with the mercury sphygmomanometer in the consulting room in sitting position after about 5–10 minutes of rest according to standard guidelines5. Patients of hypertension with renal failure, valvular heart disease, co-existent ischemic heart disease, gross congestive cardiac failure, atrial fibrillation, hypertrophic obstructive cardiomyopathy, severe anemia, diabetes mellitus and on treatment with antihypertensive drugs were excluded from the study. Complete history and physical examination along with routine hematological and biochemical investigations were done. Chest X-ray P-A view and ECG was done in all patients. Patients satisfying all the inclusion criteria were subjected to echocardiography. Echocardiography was done by a doctor trained and accredited by Indian Academy of Echocardiography on GE (Logiq 3) expert model no. AY-15 CUI.M-mode echocardiography was used to measure Left ventricular interior diameter at end systole –LVIDes, Left ventricular interior diameter at end diastole- LVIDed, Interventricular Septal Dimension end systole –IVSes, Interventricular Septal Dimension end diastole- IVSed, Left ventricular Posterior wall dimension end systole LVPWDes, Left ventricular Posterior wall dimension end diastole LVPWDed, End diastolic volume – EDV and End systolic volume-ESV. Left ventricular mass was calculated according to CUBED formula (i.e. TECHHOLZ formula) as, Left ventricular Mass = (IVS + LVIDed+ LVPWD)³ - (LVID)³× 1.05gm/cm³ (Where 1.05gm/cm³ is specific gravity of muscle). Left ventricular Hypertrophy was reported if Left ventricular mass was >150gm/cm³ for men and>120gm/cm³ for women. The ejection fraction (EF) in percentage was calculated using the formulae – E.F.= (LVIDd³ – LVIDs³) / LVIDd³ and E.F. (%)= EDV- ESV / EDV ×100. Evaluation of diastolic dysfunction was carried out by E/A ratio, Deceleration time and LA size. Ventricular diastolic function was measured by pulsed wave and continuous wave Doppler echocardiography. The mitral inflow velocities at the leaflet tips was used to assess LV diastolic dysfunction as this is the point at which mitral flow velocities are equal.
RESULTS All the patients selected for this study underwent echocardiographic evaluation by 2D, M mode and Doppler echocardiography. The age of the participants in the study ranged from 35 years to 70 years with a range of 35 years. The average age of a study subject was 53.48 years. The age of patients with left ventricular diastolic dysfunction ranged from 45 years to 70 years with a range of 25 years. The average age of a patient with left ventricular diastolic dysfunction was 59.66 years. The age of patients without left ventricular diastolic dysfunction ranged from 35 years to 72 years with a range of 37 years. The average age of a patient with hypertension and without left ventricular diastolic dysfunction was 47.69 years. The duration of hypertension in the study population, ranged from ½ year to 10 years. 7 patients were newly detected hypertensive. The mean duration of hypertension in the study population was 3.06 years. In patients with left ventricular diastolic dysfunction, the duration of hypertension ranged from 1 year to 10 years. Only 1 patient with left ventricular diastolic dysfunction was newly detected hypertensive. The mean duration of hypertension in hypertensive patients with left ventricular diastolic dysfunction was 4.5 years.
Table 1: Left ventricular indices derived from M-mode echocardiography in study population
The LVIDed was obtained on M mode echocardiography with the transducer positioned in the standard left parasternal position and directed through the interventricular septum and left ventricular posterior wall at the level of the Chordae tendinae. The mean LVIDed in patients with and without left ventricular diastolic dysfunction was 4.68 cms and 4.62 cms respectively. The LVIDes was obtained for all the patients in the study on M mode echocardiography. The mean LVIDes in patients with Left ventricular diastolic dysfunction was 3.15 cms. The mean LVIDes in patients without left ventricular diastolic dysfunction was 2.87 cms. The mean IVSed in patients with left ventricular diastolic dysfunction was 0.94 cms. The mean IVSed in patients without left ventricular diastolic dysfunction was 0.85 cms. The presence of left ventricular hypertrophy was assessed on M mode echocardiogtraphy using Teichholz (Cubed) formula as - LV Mass = (IVS +LVIDed +PW)³ - (LVIDed)³ × 1.05g/cm³ LV Mass > 150g/cm³ is reported as LVH for men and > 120g/cm³ is reported as LVH for women. Out of the 50 patients studied, 35 patients (70%) had evidence of left ventricular hypertrophy on M mode echocardiography. Thus, the prevalence of left ventricular hypertrophy in the study group was 46%.Out of the 35 patients with left ventricular hypertrophy on M mode echocardiography, 23 patients had left ventricular diastolic dysfunction on Doppler echocardiotgraphy. Thus, the prevalence of left ventricular diastolic dysfunction in patients with left ventricular hypertrophy was 65.71% Out of the 27 patients, with left ventricular diastolic dysfunction on Doppler echocardiography, 23 patients had left ventricular hypertrophy on M mode echocardiography. Thus, the prevalence of left ventricular hypertrophy in patients of hypertension with left ventricular diastolic dysfunction was 85.18%. Patients were evaluated for the presence of regional wall motion abnormalities on 2D echocardiography. No patient included in the study showed regional wall motion abnormalities (RWMA). Volume in ml of the left ventricle at the end of diastole when maximally distended was recorded with help of M mode measurements. The EDV ranged from 48.83 ml to 196.12 ml. Mean End Diastolic Volume (EDV) in patients with left ventricular diastolic dysfunction was 107.63ml.Mean End Diastolic Volume (EDV) in patients without left ventricular diastolic dysfunction was 99.98 ml. The volume in ml of the left ventricle at the end of systole when maximally contracted was recorded M Mode measurements. The ESV ranged from 10.40 ml to 77.30 ml. The mean End Systolic Volume (ESV) in patients with left ventricular diastolic dysfunction was 40.33 ml. The mean End Systolic Volume (ESV) in patients without left ventricular diastolic dysfunction was 28.81 ml. In the present study, the Ejection Fraction (EF) of patients ranged from 50% to 78.70%.The mean Ejection Fraction (EF) in patients with left ventricular diastolic dysfunction was 63.19%.The mean ejection fraction (EF) in patients without left ventricular diastolic dysfunction was 69.47%.
Table 2: Left ventricular indices derived on Doppler echocardiography in study population
The Peak Early Filling Velocity (E) and Peak Atrial Filling velocity (A) were measured at the mitral leaflet tips by Doppler echocardiography. The E/A ratio was calculated to assess the presence of left ventricular diastolic dysfunction. An E/A ratio less than 1.0 was considered indicative of the presence of left ventricular diastolic dysfunction.27 out of the 50 patients studied had an E/A ratio less than 1.0 suggesting the presence of left ventricular diastolic dysfunction. The E/A ratio in the study population ranged from 0.5 to 1.85. E wave deceleration time (EDT) was more than 200ms in 20 patients out of 27 patients having diastolic dysfunction. LA size is more than 4 cm in 12 out of 27 patients having left ventricular diastolic dysfunction.
Table 3: Observations of number of patients with increased left ventricular mass by TEICHHOLZ FORMULA in study population
Table 4: Correlation between Left ventricular hypertrophy and left ventricular diastolic dysfunction
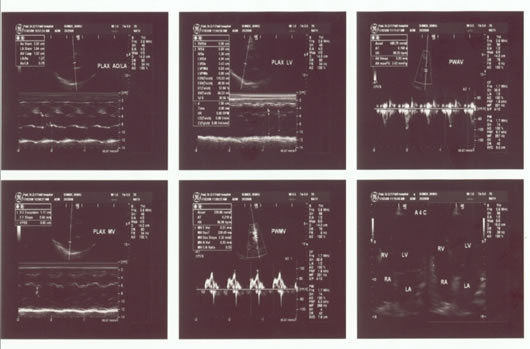
Patients were evaluated for the presence of regional wall motion abnormalities on 2D echocardiography. No patient included in the study showed regional wall motion abnormalities (RWMA). Volume in ml of the left ventricle at the end of diastole when maximally distended was recorded with help of M mode measurements. The EDV ranged from 48.83 ml to 196.12 ml. Mean End Diastolic Volume (EDV) in patients with left ventricular diastolic dysfunction was 107.63ml.Mean End Diastolic Volume (EDV) in patients without left ventricular diastolic dysfunction was 99.98 ml.The volume in ml of the left ventricle at the end of systole when maximally contracted was recorded M Mode measurements. The ESV ranged from 10.40 ml to 77.30 ml. The mean End Systolic Volume (ESV) in patients with left ventricular diastolic dysfunction was 40.33 ml. The mean End Systolic Volume (ESV) in patients without left ventricular diastolic dysfunction was 28.81 ml. A comparison of the volume of blood pumped out of the left ventricle in one cycle to the end diastolic volume (EDV), the greatest volume of the left ventricle, gives the proportion (fraction) of the total left ventricular volume which is pumped out in one cardiac cycle. In the present study, the Ejection Fraction (EF) of patients ranged from 50% to 78.70%.The mean Ejection Fraction (EF) in patients with left ventricular diastolic dysfunction was 63.19%.The mean ejection fraction (EF) in patients without left ventricular diastolic dysfunction was 69.47%. The Peak Early Filling Velocity (E) was measured at the mitral leaflet tips by Doppler echocardiography. The E values ranged from 0.43 m/sec to 1.9 m/sec in the study population. The mean E value in patients with left ventricular diastolic dysfunction was 0.68 m/sec. The mean E value in patient without left ventricular diastolic dysfunction was 0.88 m/sec. The Peak Atrial Filling velocity (A) was measured at the mitral leaflet tips by Doppler echocardiography. The A values in the study population ranged from 0.47 cm/sec to 1.14 m/sec. The mean A value in patients with left ventricular diastolic dysfunction was 0.97 m/sec. The mean A value in patients without left ventricular diastolic dysfunction was 0.67 m/sec. The E/A ratio was calculated to assess the presence of left ventricular diastolic dysfunction. An E/A ratio less than 1.0 was considered indicative of the presence of left ventricular diastolic dysfunction.27 out of the 50 patients studied had an E/A ratio less than 1.0 suggesting the presence of left ventricular diastolic dysfunction. The E/A ratio in the study population ranged from 0.5 to 1.85.The E/A ratio in patients with left ventricular diastolic dysfunction was 0.71The mean E/A ratio in patients without left ventricular diastolic dysfunction was 1.36.LA size is more than 4 cms in 12 out of 27 patients having left ventricular diastolic dysfunction. Figure 1: 2-D echocardiogram and color Doppler of 62 years old male patient who is known hypertensive for 7 years showing E/A ratio of 0.55, along with cardiomegaly on chest X ray and LVH on ECG.
DISCUSSION Initially, the assessment of the diastolic function was carried out by invasive methods like ventriculography requiring exposure to radiocontrast dyes, irradiation, considerable pain to the patient, and skill on the part of the operator. This has now been replaced by non-invasive techniques like radionuclide ventriculography and echocardiography. Echocardiography is particularly attractive as a modality to evaluate ventricular diastolic function as it is painless, freely available, relatively inexpensive, non-invasive, reproducible, does not involve exposure to radiation or radio contrast agents and shows excellent co-relation with diastolic function indexes generated by the more invasive and technically demanding studies. To apply these Doppler indices in clinical practice, it is important to determine mitral inflow velocity in a large population group with a wide range of ages and both genders. Other factors, besides ventricular compliance, which may affect the measurements of left ventricular inflow velocity should be looked into for a better understanding. In present study, all the diastolic parameters were determinedbypulsed Doppler echocardiography inhypertensive patients with and without left ventricular hypertrophy. With advancing age, the prevalence of left, ventricular diastolic dysfunction increases. This is explained by the increased duration of arterial hypertension with advancing age and also the independent effects of aging on left ventricular relaxation. Li SY et al6 also detailed the effects of aging on left ventricular diastolic dysfunction and pointed out that the increased incidence of impaired relaxation and increased passive stiffness was due to increased interstitial collagen content and decreased number of functioning myocytes that occur as part of the normal ageing process. As the duration of the hypertensive state increased, prevalence of echocardiographic evidence of left ventricular diastolic dysfunction also increased. This is explained by the progressive nature of adaptive changes occurring in the left ventricular myocardium in face of the increased afterload characteristic of the hypertensive state7. Isovolumic relaxation time (IVRT), ratio of mitral inflow E (early diastolic filling wave) and A (late diastolic/atrial filling wave) velocities, deceleration time of E velocity, and duration of A wave can all be used to assess diastolic dysfunction8. The presence of left ventricular hypertrophy was assessed on M mode echocardiography. Out of the 50 patients studied, 35 patients (70%) had evidence of left ventricular hypertrophy with the prevalence of 70%. Out of these 35 patients, 23 patients had left ventricular diastolic dysfunction on Doppler echocardiography. Thus, the prevalence of left ventricular diastolic dysfunction in patients with left ventricular hypertrophy was 65.71%. Out of the 27 patients with left ventricular diastolic dysfunction on Doppler echocardiography, 23 patients had left ventricular hypertrophy on M mode echocardiography. Thus, the prevalence of left ventricular hypertrophy in patients of hypertension with left ventricular diastolic dysfunction was 85.88%. Dipette D J and Frohlich E9 reported diastolic dysfunction manifested by reduced ventricular dispensability of a hypertrophied left ventricle in patients of hypertension to be an early characteristic of the hypertensive heart disease. Pavulopoulos H et al7 reported that left ventricular diastolic dysfunction appears early in hypertensive disease, before the onset of abnormal remodeling or LV hypertrophy. With progression of the remodeling process and the advance of LVH, diastolic function progressively deteriorates. Rusconi C and coworkers10 reported that in a large group of hypertensive patients with normal left ventricular systolic function, prevalence of left ventricular diastolic dysfunction as assessed by Doppler echocardiography stood at 51%. This finding correlates well with the findings from the present study.A study done by Lele RD and coworkers11 from India found isolated diastolic dysfunction in 66% patients by myocardial perfusion imaging. This percentage is very close to the present study. A strong case may be made for the screening of all hypertensives with clinical cardiomegaly by echocardiography for the presence of left ventricular diastolic dysfunction.Echocardiography allows for rapid, noninvasive assessment of LV function in hypertensive patients. It can evaluate morphological and hemodynamic changes acutely and over time. Parameters obtained with echocardiography may help in management of patients.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home