|
Table of Content - Volume 21 Issue 3 - March 2022
Efficacy of fractional radiofrequency in management of acne scars: A Retrospective study
Ajay Ovhal1, Deesha Ovhal2
1Professor & HOD, Department of Skin & VD, Government Medical College, Latur, Maharashtra, INDIA. 2Director, Marvel Skin, Hair and Laser Clinic, Latur, Maharashtra, INDIA. Email: drajayovhal@gmail.com
Abstract Background: There are various treatment modalitieslike chemical peeling, subcision, laser resurfacing with CO2 laser, ErYAG laser are available for treatment of acne scars. Ablative lasers are most effective but associated with drawback of hyperpigmentation in type IV and V i.e. Indian skin types. The fractional radiofrequency (FRF) system have reported to cause dermal regeneration with minimal epidermal changes.This study was designed to assess efficacy of FRF in treatment of acne scars. Aims: This study is to asess efficacy of FRF for treatment of acne scars. Methods and Material: Thirty-one patients with acne scars received three treatments with FRF at the interval of 4 weeks. Acne scar assessment was done with Goodman and Baron’s grading (GBG) and Echelle d’Evaluation Clinque des cicatrices (ECCA) system on pre and post treatment photographs taken at first visit and one month after the last treatment. Statistical analysis used: Wilcoxan signed rank test. Results: The results were assessed quantitatively by GBG showed improvement of 23 (63.8%) patients from grade 3 to grade 1 and 6 (75%) patients from grade 4 to grade 2. Thus 20 patients (64%) patients showed improvement by 2 grades. Median GB score improved from 18 to 8 and median EACC score improved from 45 to 20 after the treatment which are statistically significant on applying Wilcoxan signed rank test.No significant adverse effects like post inflammatory hyperpigmentation were seen. Conclusions: FRF is effective for treatment of moderate to severe acne scars. Key words: fractional radiofrequency, acne scars, lasers, non-ablative lasers.
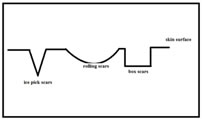
INTRODUCTION Acne is common in adolescents. Acne is present in various grades of severity of grade 1 to grade 4. The most unwarranted sequelae of acne are acne scarring.1 Acne may cause scarring even in mild grades of acne. The incidence rate of acne scars is 11-90% in men and women as reported in various studies.2 Acne scars lead to detrimental impacts on psychosocial life of adolescent patients. Aim of acne treatment is prevention of permanent acne scarring. Severe grades of acne or delay in treatment may lead to the development of acne scars. Acne scars are classified into atrophic and hypertrophic types of scars. AAtrophic acne scars are classified as ice pick, box and rolling type of acne scars.[Figure 1]Acne scar treatment armamentarium involves chemical peeling, subcision, laser resurfacing with CO2laser, ErYAG laser, etc.1 Even though ablative lasers are known to be effective for treating acne scars, they are associated with prolonged downtime and the drawback of hyperpigmentation in Indian skin i.e. types type IV and V.3 The fractional radiofrequency (FRF) system has reported to cause dermal regeneration with minimal epidermal changes.4 FRF principly works by generating heat by radiofrequency and heating dermis thereby stimulating the collagen tissue, promoting the regeneration of collagen and the reconstruction of soft tissues.6 Fractional radiofrequency energy can be delivered by two different modes such as needles or by an array of elecrodes.5 This study is to asess the efficacy of FRF delivered by elecrodes for treatment of acne scars.
SUBJECTS AND METHODS This is a retrospective, cohort study performed on study population of patients with acne scars treated with FRF between January 2016 to December 2017 at Government Medical College, Latur. Institutional Ethical Committee approval was taken. Healthy men and women above 16 yrs of age with acne scars were included in study. Pregnant females or those having active acne were excluded. Similarly patients with active electric or facial implant, history of surgical, chemical, light based treatment, isotretinoin treatment in past 3 months, keloidal tendiences were excluded from the study. Thirty one patients satisfied the criteria which included 18 female and 13 male patients having mean age of 22.48 yrs. The patients were given 3 treatment sessions of FRF at the interval of 4 weeks. The treatment parameters were decided based on scar severity. The procedure area was cleaned with cleanser, topical anesthetic cream was applied over the face for 30 min before procedure. The patients were given 2 passes with 30% overlapping. The photographs were taken before and one month after 3rd sitting of the treatment. The photographs were assessed and improvement was determined by Global acne severity classification of the Goodman and Baron (GB) (qualitative and quantitative)and Echelle d’Evaluation clinque des cicatrices (ECCA) for acne scarring.[Table1 to 5] After the procedure patients were advised moisturizers and sun protection for 1 week. If patient experienced pain he was advised to take a paracetamol tablet. Fractional radiofrequency instrument: This instrument delivers fractional radiofrequency energy via electrode pin arrays. Two types of sets of electrodes having 64 pins and 81 pins are provided and the tip size is 21mm X 21mm and 13.5mmX 13.5mm. .[Figure 2] The pins on tip are connected to bipolar radiofrequency electrodes which form positively and negatively charged electrodes and deliver energy upto 1.15 MHz at multiple points. The energy of 11-142 mj/pin and of 20 J by the assembly of pins is delivered to the skin surface in contact by sparing adajacent areas thus creating fractional effect. [Figure 3] The energy can be delivered by selecting modes provided in instrument from M1 to M4. M1 mode delivers energy at superficial level of dermis and M4 upto deep layers of dermis. More energy was deliverd to areas having moderate to severe scarring over cheek by selecting M3 and M4 modes and bony areas were given M1 and M2 modes of energy. [Figure 4]The study was performed using fractional radiofrequency device ‘Dermatrix’, manufactured by GSD.
RESULTS The patients in this study group presented with an ice pick, box and rolling types of acne scars. All types of scars showed improvement in form of decrease in depth, improvement in the texture of skin, and softening of contours. The rolling scars responded the best and box scars the least. There were total 31 patients, 18 females and 13males, between the age group of 16 to 40 years with mean age of 22.48 years. The physician’s quantitative assessment of GB quantitative scar grading system showed 23 patients with grade 3 and 8 patients with grade 4 acne scarring.[Table 6] Out of these 23 grade 3 patients, 14 (60.8%) improved to grade 1 and of those 8 grade 4 patients, 6 (75%) improved to grade 2 acne scarring. Thus, average 64% patients showed improvement by 2 grades and 35% patients ( 11 out of 31) showed improvement by 1 grade. [Table 6] [Photographs 1 to 6] GB quantitative assessment showed a moderate reduction in the 21(67.7%), good reduction in the 4 (12.9%), very good in 6 (19.3%) patients.[Table 7] The qualitative assessment showed improvement of median GB score from 18 before to 8 after treatment, whereas a median EAAC score improved from 45 before to 20 after the treatment. Wilcoxan signed rank test was applied to GB score before and after the treatment had ‘z’ value of 4.88 and ‘p’ value <0.001 which are statistically significant. Similarly, EAAC score median value before and after the treatment had ‘z’ value of 4.95 and ‘p’ value <0.001 which are significant. [Table 8 and 9] The treatment had erythema and burning pain for 1-2 hours after the session in almost all patients, which was managed with cold compressess and paracetamol tablets if required. The erythema subsided in 1-2 hours, followed by mild edema and crusting which persisted at the most for 7 days. No patient reported post inflammatory hyperpigmentation. One patient had persistent track marks for period of 3 weeks.
Figure 1 Figure 2
Figure 3 Figure 4
Table 1: Goodman-and-Barons-qualitative-scar-scale
Table 2: Goodman-and-Barons-quantitative-scar-scale
Table 3: Grades of acne
Table 4: Assessment of improvement
Table 5: Echelle d’Evaluation cliniaue des Cicatrices d’acne (ECCa)
Table 6: Distribution of patients according to GB grade before and after treatment.
Table 7: Improvement status by quantitative GB score
Table 8: Comparison of GB score before and after treatment.
Table 9: Comparison of EAAC score before and after treatment.
Test applied for table 8 and 9 is Wilcoxan signed rank test. Figure 1: Pre Post Figure 2
Figure 3 Figure 4 Figure 5 Figure 6
DISCUSSION Various modalities for treatment of acne scarring like peeling are too mild or too harsh like ablative lasers.6 Moreover, procedures for acne scarring have great concern regarding downtime and post inflammatory hyperpigmentation.2 FRF devices deliver heating directly to the dermis without significant epidermal damage. The RF devices do not target chromophores but heat the dermis by conduction of electrons through target tissue forming triangular zones of coagulation.1 All acne scar patients showed improvement. This study demonstrtes 64% of patients showing improvement by 2 grades, without significant adverse events even in type IV and V skin types. There is improvement in skin texture, hyperpigmentation just in a week. Similar studies performed by FRF devices in past have shown 50-90% improvement in acne scars.7 It has been observed in this study that mild to moderate scarring responds better than severe scars. Though there is decrease in acne scars by 2 grades in grade 4 acne scar patients, residual grade 2 scarring may not be acceptable by the patient. Severe acne scars may require a greater number of treatments for their better outcome. In the current treatment protocol only 3 treatments were given in the interval of 4 weeks as recommended by manufacturer of the instrument. The improvement in acne scars by individual scar types was not considered as counting them only by numbers may be misleading. The disposable tips used for FRF treatment are now available at affordable costs and may not pose an obstacle for using this technology. Considering these facts, it would be prudent to have a fractional radiofrequency as a first line therapy for treatment of mild to moderate acne scars in IV and V skin types. In severe acne scarring ablative lasers combined with FRF may deliver better outcomes.8 More number of FRF treatment sessions given over longer duration may give improved outcomes. This is a retrospective study and is its limitation. Further studies with randomised, blinded, split face, prospective studies with FRF and FRF in combination with ablative lasers for severe acne scars having large sample size should be planned for further research.
CONCLUSION The treatment with fractional radiofrequency is safe and effective for treatment of acne scarring with IV and V skin types. FRF treatment shows improvement in all types of acne scars. FRF provides the advantage of minimum downtime and no risk of post inflammatory hyperpigmentation.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home