|
Table of Content - Volume 16 Issue 1 - October2020
Brain abscess in TOF - The storm we dealt with
Islam MT1*, Hussain MZ2, Karim T3, Alam MS4, Barua Chaity5, Bhuiyan Md Mustafizur6, Munira Shirajum7
1,3Associate Professor, 2Professor, 4,5Assistant Professor, 6Medical Officer, 7Resident, Department of Paediatric Cardiology, BSMMU, Shahbag, Dhaka, BANGLADESH. Email: tariqul125@yahoo.com
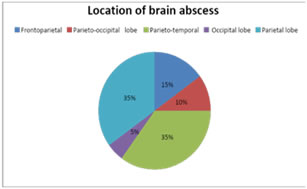
Abstract We reviewed twenty cases of brain abscess with Tetralogy of Fallot`s (TOF). A sharp peak in the age distribution was seen at 6 to 10 years of age. 85% of the cases were presented with fever, 70% had headache, neurological deficit at presentation were seen in 50% cases where as decreased consciousness level found in 10%. The majority of these abscesses were supratentorial and 70% of abscesses were found in the temporal, and parietal lobes. Multiple abscesses were present in 25% of cases and increasing percentage of sterile cultures seems to be the result of broad-spectrum antibiotic therapy. Cases lived with neurological deficit were 60% whereas the overall mortality rate was 10%. One patient died after surgical excision secondary to aspiration. Since the introduction of computerized tomography, aspiration without total excision has produced good results, and therefore it is believed that the number of cases which are cured with aspiration therapy alone will gradually increase in the future. With advancement of management dealing with the storm like brain abscess with TOF become feasible with some neurological deficit. Key words: Brain abscess, TOF, Brain edema, Ventriculomegaly
INTRODUCTION Central nervous system lesions in association with congenital cyanotic heart disease has long been recognized. The two most serious complications of central nervous system resulting from unoperated congenital heart disease are cerebral intravascular thrombosis and intracranial suppuration. Brain abscess is a severe infection of brain tissue that can be caused by bacteria, fungi, protozoa, and parasites.1-3 The mortality rate caused by brain abscess is about 10%.1 Cyanotic congenital heart disease (CHD) with right-to-left shunt is one of the most frequent predisposing factors to brain abscess in children.1,4 Of children with cyanotic CHD, 5-18% develop brain abscess complications.1 It is postulated due to increased viscosity of blood. This in turn includes intravascular thrombosis leading to small infarctions in the brain. During the phase of transient bacteremia the virulent organism in the shunted blood finds a rich media to grow. This may this follow local cerebritis. The poor host response in these patients enhances the process further. Lack of encapsulation in these abscesses make the situation more serious.5-11 Besides their cardiopulmonary risk, these patients have wide variety of coagulation defects. Often they do not tolerate systemic hypotension. These factors together increase the risk of anesthesia and surgery.7-12 According to Matson, la "a fatal cerebrovascular accident or cerebral abscess was once looked upon almost as welcome release from the miserable existence of a cardiac cripple." However, recent progress in neurosurgery and cardiac surgery has made it possible to extend the normal life of these patients. The introduction of computerized tomography (CT) has facilitated early detection and accurate characterization of these lesions. This study reviews the experience with 20 cases of brain abscess with TOF. METHODS This is a retrospective, longitudinal study conducted in Bangabandhu Sheikh Mujib medical university, Dhaka, Bangladesh, from 2012 until 2018. Data were collected from medical records. Inclusion criteria for the study group were age between 1 year - 18 years with diagnoses of brain abscess and TOF. The exclusion criteria were included incomplete medical records or cases of other cyanotic CHD and patients who had undergone corrective heart surgery. Nutritional status was determined with WHO growth chart (normal: weight for age and weight for height between 2SD and -2SD, undernourished: weight for age or weight for height <-2SD, severe malnutrition: weight for age or weight for height <-3SD, and stunted: height for age <-2SD). Developmental status was determined using Denver II developmental screening test and was assessed in 4 major milestones aspect of which were, personal social, fine motor, language and gross motor aspect (normal: no developmental delay, delayed: delay in no more than 1 aspect, global developmental delay: delay in 2 or more aspect); and immunization status was classified as completed or not based on National Immunization Programme of Bangladesh based on the age of subject. Data were collected and analyzed with SPSS 22. The study was approved by the institutional research board of BSMMU.
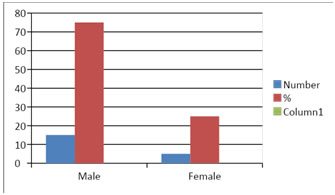
RESULTS A total of 20 cases of brain abscess in children with TOF were found in the 7-year study period. The demographic characteristics of subjects are described in Table 1. The mean age was 6 years, and most subjects were male (75%), whereas female were 25%. Of the cases 50% were found to be stunted. Developmental delay noticed in 7 cases (35%) and 12 cases (60%) were found to have normal development. 80% of the cases were immunized as per EPI schedule. Most of the patients were from lower socioeconomic background and residing in rural community. The outcomes of the case group are described in Table 2. During admission 85% cases presented with fever, 40% had seizure and 70% had headache. Abscess drainage was done only in 7 cases (35%). After drainage of brain abscess, fluid culture results in subjects with abscess drainage were Streptococcocus, Eschericia coli, and Staphylococcus warneri, while in 2 cases there were no growths. Antibiotics were given based on sensitivity and resistance results. 35% of the abscesses were found to be occupied in the paritotemporal and parietal lobe of the brain, demonstrated at CT scan reports. Neurological deficit noticed at 50% cases. Most cases had single abscess (75%). 2(10%) cases died; one in the post-operative days and other after admission. Table 1: Age distribution of cases(n=20)
Figure 1: Bar diagram showing male, female ratio.
Table 2: Other Demographic data(n=20)
Table 3: Outcome of Brain abscess(n=20)
DISCUSSION Hanna,13 Garfield J,14 and Molinari GF15 reported an incidence of brain abscess varying from 3.8% to 5.7% in fatal cases of congenital anomalies of the heart and great vessels. Maronde 1~ reported 11 cases of brain abscess associated with congenital heart disease (an incidence in their series of 10.4%); Clark,5 Matson and Salam16 have emphasized the rarity of an abscess occurring in children under the age of 2 years. In our study, a 7-year period, there were 20 subjects with brain abscess and TOF. A sharp peak was observed between 6 and 10 years old and the youngest subject was below 5 years of age. These data support the previous evidence which concluded that the brain abscess formation rarely happen on infants (<1 year old).17 The majority of these abscesses are supratentorial. In our series, 70% of abscesses were found in the temporal, and parietal lobes. This undoubtedly reflects the common metastatic hematogenous etiology? Multiple abscesses were present in 25% of our cases. Bacteria from the aspirated pus were generally Staphylococci and Streptococci found in our series. Sterile cultures have been reported in about 20% of brain abscesses of other etiologies18,19,20 In brain abscesses with congenital heart disease, sterile cultures were reported in 16% by Fisch- bein, et al.,21 and in 44% by Matson and Salam?16 The control of polycythemia, oxygen desaturation, and arteriovenous shunt should decrease the possibility for thrombus formation, infarction, and embolic disorders. However, predisposing conditions before heart surgery, such as minute encephalomalacia, will still play a major role.16,21,22,23 The evolutional mechanism of brain abscess in cyanotic heart disease has been the subject of much controversy. It is clear that there are several important factors influencing this evolution. The most important factor is polycythemia which induces intravascular thrombosis as a cause of infarct.15 The increased viscosity of blood resulting from compensatory polycythemia and the reduced rate of flow in the micro- circulation of the brain are predisposing factors. In addition, diminished oxygen tension or actual brain hypoxia may already be present so that the arrival of shunted blood containing virulent organisms may well be followed by focal cerebritis. Bacteremia episodes in infants are extremely rare. Also, dentation has been theorized as the most frequent source of intermittent bacteremia, so younger children with incomplete tooth growth may be less prone.24 The outcomes of our serial 20 brain abscess cases were as follows: 2/20 subjects died, 12/20 subjects lived with neurological sequelae and 6/20 subjects lived without neurological deficits. Similarly, a previous study in 2006 reported that 16% of subjects died, 53% lived with neurological sequelae, and 30% lived without neurological sequelae. A weakness of this study was the small sample size and retrospective design for which complete medical records are very important. The strength of this study was that it was the first of such studies in Bangladesh. Our initial findings reported here provide basic data on evaluation of risk factors and outcomes of brain abscess in children with TOF in Bangladesh.
CONCLUSION With advancement of investigations like CT scan and management with antibiotics and surgical approach we can deal well with the storm like brain abscess in TOF. Conflict of Interest: None declared.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home