|
Table of Content - Volume 16 Issue 2 - November 2020
Anaemia among SAM children and its effect on outcome in nutritional rehabilitation centre at tertiary care centre of Gujarat
Seema Shah1, Nisha Prajapati2*
1Assistant Professor, 2Associate Professor, Department of Paediatrics, GMERS Medical College, Gandhinagar, Gujrat, INDIA. Email: nishuydarji@gmail.com
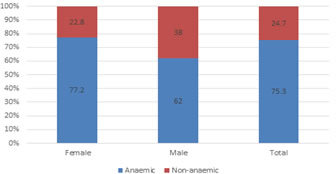
Abstract Background: Severe Acute Malnutrition is one of the most common cause which contributes towards the under 5 mortality in India. It results in the various pathophysiological changes in the body systems including significant changes in hematological parameters. Low red cell counts resulting in Anaemia has always been a constant feature of protein energy malnutrition and may be normochromic normocytic, microcytic hypochromic or macrocytic. Methodology: Retrospective observational study conducted by retrieving data of SAM children who were admitted in Nutritional Rehabilitation Centre during calendar year 2018. Primary outcome variables were mean rate of weight gain (gm/kg/day), proportion of children achieving target weight and recovery from SAM status. The mean rate of weight gain (g/kg/day) was calculated as weight gain over a defined time period divided by the number of days in anaemic and non-anaemic children. Result: In present study, 75.3% children with SAM were found to be anaemic, out of which 3.7% were severely anaemic and 96.3% were mild anaemic. This proportion is higher among female compare to male. There is no significant difference in weight gain and anaemia status. Conclusion: It was concluding that nearly all patients with severe acute malnutrition had anaemia as a common co-morbid condition. Most of them suffered from moderate to severe anaemia. This anaemia status don’t affect the outcome of treatment. Key Words: Anaemia, NRC, Sever Acute Malnutrition
INTRODUCTION Malnutrition is result of deficiency of one or more macronutrients to body tissues which leads to inadequate bodily functions,1 and numerous micronutrient deficiencies usually associated with this. Malnutrition is a broad concept that includes over nutrition and undernutrition. Undernutrition is a variety of clinical conditions such as kwashiorkor, marasmus, marasmic kwashiorkor, wasting or stunting, and micronutrient deficiencies. Severe malnutrition - often referred to as severe acute malnutrition (SAM) - is defined as a WHZ of more than three SDs below the mean, or a mid-upper arm circumference (MUAC) of less than 115 mm, or the presence of nutritional oedema. It results in the various pathophysiological changes in the body systems including significant changes in hematological parameters. Low red cell counts resulting in Anaemia has always been a constant feature of protein energy malnutrition and may be normochromic normocytic, microcytic hypochromic or macrocytic.2,3The Facility based care is being implemented through a network of CMTCs and NRCs. The admission criteria is W/H less than –3Z score or MUAC <115mm, or bilateral pedal oedema. The appetite test for all children is undertaken. The children are admitted for 14-21 days. They are given locally made F-75 and F-100. The children are discharged after regaining good appetite and body weight. After the discharge, registration of child to ICDS scheme is undertaken and follow up of Children is done through home visit As there were few studies conducted on the prevalence, pattern and outcome of anaemia in SAM children, present study has been designed to identify the prevalence of anaemia in SAM children admitted to NRC and to find out whether there is any correlation between the degree of anaemia and outcome in terms of weight gain.
MATERIAL AND METHODS For the purpose of this analysis, we retrieved the data of all children with SAM admitted from 1 January, 2018 to 31 December, 2018 to NRC. The detection of children with SAM was ensured in the villages by the community workers of the Integrated Child Development Services (ICDS) program either as part of monthly growth monitoring and promotion sessions at the ICDS center (passive case finding) or in the context of community drives for the identification of children with SAM (active case finding). At the NRC, a physician conducted a clinical examination in children to detect the presence/absence of medical complications (altered alertness, respiratory tract infections, diarrhoea/severe dehydration, high fever/ malaria, tuberculosis, and/or severe Anaemia) using the criteria for the Integrated Management of Neonatal and Childhood Illnesses (IMNCI).[4] Children with medical complications, and/or bilateral pitting edema, and/or with poor appetite were fed a locally-prepared therapeutic formula meant as a substitute for F-75 (herewith referred to as F75-proxy) to provide 100 kcal/kg/day. Classification of anaemia based on haemoglobin levels Mild anaemia: 10-10.9 g/dL, Moderate anaemia: 7-9.9 g/dL and Severe anaemia: <7 g/dL5 Primary outcome variables were mean rate of weight gain (gm/kg/day), proportion of children achieving target weight and recovery from SAM status. The mean rate of weight gain (g/kg/day) was calculated as weight gain over a defined time period divided by the number of days in anaemic and non-anaemic children.
OBSERVATIONS AND RESULTS A total of 162 children, aged 6 - 59 months were referred to the NRC. Around fourty seven percentage of children were in age group 6 – 12 months. Proportion of anaemic children is mostly same in each age group (Table I). Around 75% of SAM children were anaemic and this proportion is comparative high in female compare to male children (Figure 1). Table 2 depicts that in present study, 75.3% children with SAM were found to be anaemic, 2.7% were severely anaemic and 72.6% were moderately anaemic. Anaemia is more prevelant and severe among female SAM children compare to male. There was no statistical difference in admission weight among anaemic and non-anaemic children. Anaemic children had statistically lower haemoglobin level compare to non anaemic children so these children were comparable to see the effect of Anaemia. (Table 3) There is no statistical difference in weight gain and mean weight gain percentage difference in anaemic and non anaemic children (Table 4)
Table 1: Age wise distribution of SAM children
Figure 1: Proportion of Anaemia by sex in SAM children
Table 2: Anaemia status in SAM child
Table 3: Basic parameter difference in anaemic and non-anaemic group
Table 4: Outcome difference in anaemic and non-anaemic group
DISCUSSION Anaemia associated with severe malnutrition is the consequence of multiple factors and represents an interaction between adaptation to inadequate food intake and the impact of other stresses associated with infection or dietary imbalance.[6] Lower mean values were observed for haemoglobin and haematocrit in children with SAM as compared to controls, a finding similar to previous studies.7-9 In present study, 75.3% children with SAM were found to be anaemic, out of which 3.7% were severely anaemic and 96.3% were mild anaemic. This finding was similar to a study done by Thakur et al., where they reported 81.1% severely malnourished. children to be anaemic, out of which 67.3% as severely anaemic and 13.8% as moderately anaemic.[14] In another study by R kumar et al. 88.5% children had Anaemia, 24% had severe Anaemia and 55.7% had moderate Anaemia.11 These red cell changes may be attributed to adaptation to lower metabolic oxygen requirements and decrease in lean body mass seen in PEM. Micronutrient deficiencies such as iron, zinc and copper have also been implicated as a contributory factor.12 There was no statistical difference in admission weight among anaemic and non-anaemic children. Anaemic children had statistically lower haemoglobin level compare to non anaemic children so these children were comparable to see the effect of Anaemia. On comparison of malnutrition outcome in anaemic and non-anaemic children show that Anaemia does not had effect on outcome. This may be due to iron therapy in malnourished children after first week of treatment. Thought Anaemia doesn’t have effect on weight gain, timely identification and treatment of co-morbidities like Anaemia, diarrhoea, acute respiratory tract infection and micronutrient deficiencies is vital in malnourished children, so as to break undernutrition-disease cycle, and to decrease mortality and to improve outcome.
CONCLUSION It was concluding that nearly all patients with severe acute malnutrition had anaemia as a common co-morbid condition. Most of them suffered from moderate to severe anaemia. This anaemia status don’t affect the outcome of treatment.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home