|
Table of Content - Volume 16 Issue 3 - December 2020
A study of clinical profile and outcome of children admitted with respiratory distress in a tertiary care centre
Rohit Bhandar1, Sharanagouda Patil2, Sunil Kumar3*
1Associate Professor, 2Peofessor And HOD,3Postgraduate, Department Of Paediatrics, M R Medical, Kalaburagi, Karnataka, INDIA.
Abstract Background: Respiratory distress is a common cause for admission in the PICU. Is the main symptom for various and different diseases, not including only the respiratory tract. Respiratory diseases are the most common cause for respiratory distress. Bronchiolitis and pneumonia are the most common cause of respiratory distress in children. Respiratory distress is a well-recognized cause of respiratory failure in children and is associated with a high mortality rate. Objectives: 1.To study the clinical profile of children admitted with respiratory distress2.To study the outcome of the children with respiratory distress Methods: 204 children between age group between 1month to 18year with signs of respiratory distress caused by various conditions admitted to PICU, fulfilling the inclusion criteria were included in the study. . Respiratory distress signs, vital parameters, systemic examination findings where documented in data collection form. Patients were stabilized first by maintain airway, breathing and circulation at admission, later relevant patients thoroughly examined, later relevant investigations are done to identify the cause. Patients are followed up till discharged. Results: Most common age group presenting with respiratory distress was 1m -1year, 110(53.9%). Male to female ratio was 2.04:1. Hurried breathing(87.7%),cough(79.9%) and fever(77.4%) were the most common presenting complains. Tachypnoea(96.57%), nasal flaring(82.35%) and subcostal retractions(81.86%) were the most common respiratory distress signs. Most common chest x ray findings were, infiltrations(45.09%), hyperinflated lung fields(20.58%), consolidation(14.70%). Most common system causing respiratory distress was respiratory system(81.37%),followed by endocrine disorders(4.9%), CNS(2.45%), GIT and hepatobiliary system(2.45%), CVS(1.96%), metabolic disorders(1.47%), renal system(1.47%) ,haematologic system(0.98%) and others(2.45%).Most common diseases causing respiratory distress in our study were bronchopneumonia(39.7%) ,bronchiolitis(8.82%). Conclusion: Respiratory diseases are the most common causes of respiratory distress in children. Non respiratory diseases causing respiratory distress is 18.62%. Most common diseases causing respiratory distress are bronchopneumonia, bronchiolitis and lobar pneumonia. Most common nonpreparatory disease causing respiratory distress is diabetic ketoacidosis. Most common respiratory distress signs were tachypneoa, nasal flaring and subcostal retractions. Mortality rate in patient with respiratory distress is 6.87%.Most common causes of mortality in patients with respiratory distress are bronchopneumonia and lobar pneumonia. Key Words: Respiratory distress, clinical profile, respiratory disease, bronchopneumonia
INTRODUCTION Respiratory distress refers to any kind of subjective difficulty in breathing. Objectively, it manifests as one or more of the following: altered breathing pattern (fast, slow, feeble or absent), forced breathing efforts or obstructed breathing, and chest indrawing. Respiratory distress is defined as a clinical state characterized by increased respiratory rate (tachypnea) and respiratory efforts (increased work of breathing).1 Respiratory distress is a common cause for admission in the PICU. Is the main symptom for various and different diseases, not including only the respiratory tract. Respiratory diseases are the most common cause for respiratory distress. Bronchiolitis and pneumonia are the most common cause of respiratory distress in children2.More than 1/3rd of deaths observed in children presented with severe respiratory distress and respiratory failure. Almost 2/3 rdof deaths were due to pneumonia with or without pleural involvement and made a major contribution to childhood mortality in PICU.3 Respiratory distress maybe due either to pulmonary or cardiac disease, generalized sepsis, abdominal pathology, or metabolic derangements. Respiratory distress produces detectable alterations in the pattern of breathing4. Respiratory distress is a well-recognized cause of respiratory failure in children and is associated with a high mortality rate5. Respiratory distress in children, particularly neonates and infants, must be promptly recognized and aggressively treated because they may decompensate quickly. Factors that contribute to rapid respiratory compromise in children include smaller airways, increased metabolic demands, decreased respiratory reserves, and inadequate compensatory mechanisms as compared with adults. Respiratory arrest is the most common cause of cardiac arrest in children, and outcomes are poor for patients who develop cardiopulmonary arrest because of respiratory deterioration.6 The study was conducted to determine clinical profile and outcome of children who were admitted due to respiratory distress.
Material and methods The present study was carried out in the Department of Pediatrics, Mahadevappa Rampure Medical College, Kalaburagi. Patient’s attenders were informed about the purpose of the study and written consent was before start of the study. Ethical clearance was obtained by the ethical clearance committee of the institution. The study included clinical profile and outcome of children admitted due to respiratory distress in PICU during the period from October 2018 to April 2020. Inclusion Criteria: Age group >1month to <18years of either sex admitted to picu with any of the following signs of respiratory distress,
Exclusion Criteria
METHOD OF COLLECTION OF DATA: 204 children between age group between 1month to 18year with signs of respiratory distress caused by various conditions admitted to PICU were studied. Respiratory distress signs, vital parameters, systemic examination findings where documented in data collection form. Patients were stabilized first by maintain airway, breathing and circulation at admission, later relevant patients thoroughly examined, later relevant investigations done to identify the cause of respiratory distress. Patients were followed up till they discharged. STATISTICAL ANALYSIS Descriptive and inferential statistical analysis has been carried out in the present study. The results were analysed by using SPSS version 20.0 (IBM Corporation, SPSS Inc., Chicago, IL, USA). Results on continuous measurements were presented on Mean±SD (Min-Max) and results on categorical measurements were presented in Frequency (Percentage).
RESULTS 204 children with respiratory distress were taken up for the study. In our study, most common age group presenting with respiratory distress was 1m -1yr ,representing 110(53.9%). In our study 137(67.2%) were males and 67(32.8%) were females, with male to female ratio was 2.04 : 1. Distribution of cases according to age, sex were tabulated in table no.1.
TABLE 1: DISTRIBUTION OF CASES ACCORDING TO AGE,SEX
Among 204 cases recruited in our study, common presenting complaints were hurried breathing in subjects of 179(87.74%),cough in subjects of 163(79.90%),fever in subjects of 158(77.45%),vomiting and loose stools in subjects of 33(16.17%),noisy breathing in subjects of 17(8.33%),pain abdomen and abdominal distension in subjects of 17(8.33%),convulsions and altered sensorium in subjects of 12(5.88%), gereralised edema in subjects of 6(2.94%),lethargy and irritability in subjects of 5(2.45%) and other complaints in subjects of 18(8.82%).The presenting complaints were tabulated in table no.2. TABLE 2: PRESENTING COMPLAINTS IN PATIENTS WITH RESPIRATORY DISTRESS
In our study, fully immunized subjects were 172(84.3%), partially immunized subjects were 26(12.7%) and 6(2.9%) unimmunized.6(2.9%) subjects had cyanosis at admission.147(77%) subjects had oxygen saturation <94% at admission.53(25.9%) subjects were PEM, among them 28(52.83%) , 13(24.52%), 09(16.98%) and 03(5.66%) were grade1,grade 2,grade 3 and grade4 PEM respectively. 138(67.64%) subjects were having anaemia as a associated finding. In our study, tachypnoea was seen in subjects of 197(96.57%),nasal flaring in subjects of 168(82.35%) and subcostal retractions in subjects of 167(81.86%),intercostals retractions in subjects of 111(54.4%),suprasternal retractions in subjects of 26(12.75%),wheezing in subjects of 26(12.75%),stridor in subjects of 10(4.9%),grunt in subjects of 9(4.4%) ,gasping in subjects of 2(0.98%) and bradypnoea in subjects of 1(0.49%). Table no.3 shows the respiratory distress signs.
TABLE 3: RESPIRATORY DISTRESS SIGNS
TABLE 4: CHEST X RAY FINDINGS IN RESPIRATORY DISTRESS PATIENTS
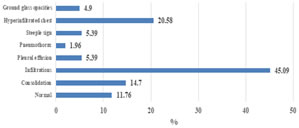
Table no.4 shows the chest x ray findings in patient with respiratory distress. Among 204 subjects, among them 24(11.76%) subjects had normal chest x ray, 92(45.09%) subjects had Infiltrations, 42(20.58%) subjects had Hyperinflated lung fields, 30(14.70%) subjects had consolidation, 11(5.39%) had pleural effusion, 11(5.39%) subjects had steeple sign,10(4.90%) subjects had ground glass opacities and 4(1.96%) subjects had pneumothorax.
GRAPH 1: CHEST X RAY FINDINGS IN RESPIRATORY DISTRESS PATIENT Among 204 subjects recruited in our study, ABG done in subjects of 53,among them 30(56.60%) subjects had metabolic acidosis with respiratory alkalosis, 7(13.20%)subjects had metabolic acidosis with respiratory acidosis with hypoxia,7(13.20%) subjects had respiratory acidosis with metabolic alkalosis , 5(9.43%) subjects had metabolic acidosis with respiratory alkalosis with hypoxia and 4(7.54%) subjects had metabolic acidosis with respiratory acidosis.
TABLE 5: ETIOLOGY OF RESPIRATORY DISTRESS
Table no.5 shows the etiology of respiratory distress. Among 204 subjects recruited in our study the etiology of respiratory distress includes, 1.Respiratory system 166(81.37%)-bronchopneumonia 81(39.70%),bronchiolitis 18(8.82%), lobar pneumonia 17(8.33%),bronchial asthma/HRAD 14(6.86%), croup 11(5.39%), WALRTI 8(3.92%), empyema thoracis 5(2.45%), pulmonary tuberculosis 4(1.96%), aspiration pneumonia 4(1.96%),ARDS 2(0.98%), pneumothorax 1(0.49%), foreign body aspiration 1(0.49%), 2.Cardiovascular system 4(1.96%) - myocarditis 2(0.98%), DCM 1(0.49%), RHD 1(0.49%), 3.GIT and hepatobiliary system 5(2.45%) - acute liver failure with hepatic encephalopathy 3(1.47%), intestinal obstruction 1(0.49%), acute gastroenteritis 1(0.49%), 4.Central nervous system 5(2.45%)- encephalitis 2(0.98%), intracranial bleed 1(0.49%), meningitis 1(0.49%), pontine glioma 1(0.49%), 5.Endocrine disorders 10(4.90%) – diabetic ketoacidosis 10(4.90%), 6.Metabolic disorders 3(1.47%)– inborn errors of metabolism 3(1.47%), 7.Haematologic disorders 2(0.98%)- anaemia 2(0.98%), 8.Renal system 3(1.47%)–nephrotic syndrome 1(0.49%), acute glomerulonephritis 1(0.49%), wilms tumor with shock 1(0.49%), 9.Others 5(2.45%)– dengue fever 3(1.47%), OP poisoning 1(0.49%),anaphylactic shock 1(0.49%). In our study oxygen required in 182(89.2%),NIV in 72(35.3%) and invasive ventilation in 30(14.7%), ICD inseration in 7(3.43%),bronchoscopic removal of FB in 1(0.49%),thoracotomy in 1(0.49%) and adrenaline injection in 1(0.49%) patient . Inotropic support was required in 18(8.82%) patients. Mean duration of oxygen, NIV and invasive ventilation requirement in our study was 2.16, 1.93 and 2.06 days respectively. The average duration of stay in PICU was 4.56days ,with minimum duration of stay was 4hr and maximum duration of stay was 16 days.
TABLE 6 :OUTCOME OF PATIENT ADMITTED WITH RESPIRATORY DISTRESS
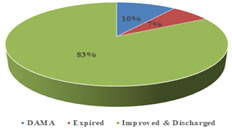
Table no.6 shows the outcome of patient admitted with respiratory distress. In our study ,the patients who improved and discharged were 169(82.84%),the patients who went against medical advice(DAMA) were 21(10.29%) and the patients who expired were 14(6.87%). GRAPH 2: OUTCOME OF PATIENT ADMITTED WITH RESPIRATORY DISTRESS
TABLE 7: CAUSES OF MORTALITY IN RESPIRATORY DISTRESS PATIENT
Table no.7 shows causes of mortality in patients admitted with respiratory distress. Among 204 subjects recruited in our study, causes of mortality were bronchopneumonia 4(28.57%),lobar pneumonia 2(14.28%),IEM 2(14.28%),aspiration pneumonia 1(7.14%),DKA 1(7.14%), viral encephalitis 1(7.14%), meningitis 1(7.14%), DHF 1(7.14%) and pontine glioma 1(7.14%) The mortality was more in age group of 1m-1yr and 1yr-5yr,accounting for 6 (42.85%) in each age group, followed by 2(14.28%) subjects in the age group of 5yr-10yr and 0(0%) in the age group of 10yr-18yr.The mortality was more in male patients 8(57.16%) comapred to female patients 6(42.85%). DISCUSSION In present study, 204 cases with respiratory distress studied. The mean age presenting with respiratory distress in our study was 3.07 ±3.75. The most common age group presenting with respiratory distress was 1m -1yr, representing 110(53.9%). In present study there is increased incidence of respiratory distress in male child compared to female. Male to female ratio was 2.04. The present study was comparable with Lekshminarayanan A et al.7, Kanwal Nayani et al..8 ,were 47% ,49.1% belonging to age group of 1m-1yr respectively. Infants most commonly present with respiratory distress compared to older children due to smaller airways, increased metabolic demands, decreased respiratory reserves, and inadequate compensatory mechanisms as compared with older children6. In present study male to female ratio was 2.04. Increased incidence of respiratory distress in male child compared to female in our study, which is comparable to Lekshminarayanan A et al..7 , Kanwal Nayani et al..8. This is due to increased incidence of infection in male as compared to females9-10. This could also be due to higher rates of care seeking for male children than for female children, given strong preferences for sons in south Asian regions11. In present study, most common presenting complaints were hurried breathing(87.74%), cough(79.90%) and fever(77.45%). K. Umamaheswara Rao et al.12 in their study breathlessness 97%, Cough 93% Fever 90% were common presenting complaints. In our study, out of 204 cases,175(77%) had oxygen saturation <94%.A similar study done by Lekshminarayanan A et al.7,were 19 (37.3%) Patients had oxygen saturation <90%.In our study ,out of 204 cases ,53(25.9%) had PEM. Among them 28(52.83%) ,13(24.52%), 09(16.98%) and03(5.66%) had grade 1,grade 2,grade 3 and grade 4 respectively. A study done by Lekshminarayanan A et al.7, were 12 (66.7%) ,6(33.3%) had grade 1 and grade 2 PEM respectively. In our study 138(67.64%) patients had anemia as associated finding. This was correlated with Lekshminarayanan A et al.7 were 34(66.7%) patients had anaemia as associated finding. In our study most common respiratory distress signs were tachypnoea(96.57%) followed by nasal falring(82.35%) and subcostal retractions(81.86%). Table no.8 shows comparison of most common respiratory distress signs with other studies.
TABLE 8: COMPARISION OF MOST COMMON RESPIRATORY DISTRESS SIGNS WITH OTHER STUDIES
TABLE 9: COMPARISION OF CHEST X RAY WITH OTHER STUDIES
In our study, most common chest x ray findings were, infiltrations(45.09%), hyperinflated lung fields(20.58%), consolidation(14.70%).Table no.9 shows comparison of chest x ray findings with other studies. In our study out of 204 cases, respiratory diseases are the most common cause for respiratory distress accounting for 166(81.37%). Other systems accounting for respiratory distress includes, Endocrine system 10(4.9%),CNS 5(2.45%),GIT and hepatobiliary system 5(2.45%),CVS 4(1.96%),Metabolic disorders 3(1.47%),renal system 3(1.47%),haemologic cause 2(0.98%) and other causes 5(2.45%). Most common causes in our study was bronchopneumonia 81(39.7%) and bronchiolitis 18(8.82%). The most common causes of respiratory distress in study done by D. Tzira et al.2 was bronchiolitis 33% and pneumonia 16% . The most common causes of respiratory distress in study done by Lekshminarayanan A et al.7 was pneumonia and WALRI 47.2%. The most common causes of respiratory distress in study done by Supriya A Patil et al.16 was bronchopneumonia(54.2%) and bronchiolitis(40%). Among 204 patients in our study, nebulisation was required in 163(79.9%), oxygen in 182(89.2%), NIV in 72(35.3%) and invasive ventilation in 30(14.7%). Mean duration of oxygen, NIV and invasive ventilation requirement in our study was 2.16, 1.93 and 2.06 days respectively. Some patients required ICD inseration in 7(3.43%), bronchoscopic removal of FB in 1,thoracotomy in 1 and adrenaline injection in 1 patient .Inotropic support was required in 18(8.82%) patients. A study done by D. Tzira et al.2, were the oxygen required in 82(45%), NIV in 12(6.5%), invasive ventilation in 87(47.8%),ICD inseration in 30(15%),tracheostomy in 6(3%). A study done by Lekshminarayanan A et al.7, were nebulisation was required in 26(51%) and inotropic support was required in 13(25.5%) Out of 204 patients in our study, the average duration of stay in PICU was 4.56days, with minimum duration of stay was 4hr and maximum duration of stay was 16 days. A study done by Lekshminarayanan A et al.7 were the average duration of stay in PICU was 5 days. Out of 204 patients in our study , the patients who improved and discharged were 169(82.84%),the patients who went against medical advice were 21(10.29%) and the patients who expired were 14(6.87%).The mortality was more in age group of 1m-1yr and 1yr-5yr,accounting for 6 (42.85%) in each age group. The mortality was more in male patients 8(57.16%) compared to female patients 6(42.85%).The most common causes for mortality were bronchopneumonia 4(28.57%) and lobar pneumonia 2(14.28%).A study done by Supriya A Patil16 were 82% cases completely recovered ,8.8% cases went against medical advice and 9.2% cases expired. A study done by M. Suhasini et al.3 were ,18 (8.45%) died among 213 patient presented with respiratory distress.
CONCLUSION Respiratory diseases are the most common causes of respiratory distress in children. Non respiratory diseases causing respiratory distress is 18.62%. Most common diseases causing respiratory distress are bronchopneumonia, bronchiolitis and lobar pneumonia. Most common non-respiratory disease causing respiratory distress is diabetic ketoacidosis. Common presenting complaints in patient with respiratory distress are hurried breathing, cough and fever. Most common respiratory distress signs were tachypneoa, nasal flaring and subcostal retractions. Mortality rate in patient with respiratory distress is 6.87%. Mortality is more in males than females. Mortality is more common in age group of 1m-1yr and 1yr-5yr.Most common causes of mortality in patients with respiratory distress are bronchopneumonia and lobar pneumonia.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home