|
Table of Content - Volume 16 Issue 3 - December 2020
Clinical assessment of fetal malnutrition in Andhra Pradesh population
Gajanan Venkatrao Surewad1*, Khyati Ambatipudi2, Rajashree Sayanna Totawad3
1,2Assistant Professor, Department of Paediatrics, 3Senior Resident, Department of Radiology, Nimra Institute Medical Sciences, Jupudi (V) Vijayawada, Krishna (Dist) Andhra Pradesh – 521456, India. Email: gvsurewad@gmail.com
Abstract Background: Fetal Malnutrition (FM) at birth indicates soft tissue wasting with Clinical Assessment of Nutritional Status (CAN) score and comparison with other methods of determining intrauterine growth. Method: 300 normal full terms (38 to 42week of gestation) neonates were selected. The CAN score, weight, length, Mean circumference was carried out to measure ponderal Index (PI). The small for gestational age (SGA) and appropriate for gestational age (AGA) newborns were also classified and compared to evaluate FM and nourished neonates. Results: The CAN parameters was 12 (4%) hair, 6 (2%) checks, 4 (1.3%) neck and chin, 3 (1%) Arms, 4 (1.3%) chest, 2 (0.66%) Abdomen. In AGA group – 16 (5.3%) were FM, 169 (56.3%) were nourished, in the comparison of CAN and PI (<2.2), 19 (6.33%) were FM, 66 (22%) nourished. In PI (>2.2) 20 (6.6%) were FM, 195 (65%) were nourished. Conclusion: This study will help to anticipate growth of baby and helps to prevent morbidity and mortality, because most of the FM babies will have intellectual and neurological defects in their later life apart from early death. Keywords: CAN, FM, SGA, AGA, PI.
INTRODUCTION Fetal Malnutrition (FM) is a term coined by scott and usher in 1966 to describe infants who showed evidence of specific aetiology.1 It is defined as failure to acquire adequate quantum of fat and muscle mass during intra-uterine growth. The existing terminologies intra uterine malnutrition includes small Gestation age (SGA) and placental insufficiency. Despite of their genetic and ethnic variations newborns with malnutrition’s observed in later life. Third trimester may have birth weight above 2.5kg are misdiagnosed as normal despite being malnourished. The importance of fetal malnutrition is emphasized because of the potentially serious sequel of malnutrition on multiple organ systems with studies showing that, 39% fetally malnourished babies had intellectual and neurological defects.2,3 As per the Roher’s Ponderal Index (PI), head circumference, to length ratio, chest circumference or mid arm circumference and/or mid arm circumference ratio (MAC/HC). The clinical assessment of nutrition (CAN) score scoring system is based on nine superficial readily detectable signs of malnutrition in the new born (4). Hence attempt was made to assess CAN score, ponderal Index (PI), AGA, SGA, to rule out various observations and results.
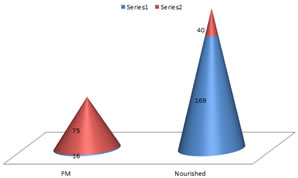
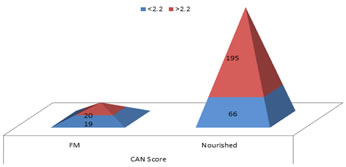
MATERIAL AND METHOD 300 new born in Nimra Institute Medical Sciences hospital Jupidi, Vijayawada, Krishna (dist) Andhra Pradesh – 521456 were studied. Inclusive Criteria: 300 term singleton new born derived consecutively in the hospital were selected. Exclusion Criteria: Newborn with NICU care, Newborn with congenital anomalies, those born mother with gestation diabetes Mellitus were excluded from study. Procedure: The observations of CAN score were tested in Newborn of normal term (38-42 week of) gestation. All neonatal anthropometry carried out. All newborns were weighed by digital lever standardized weighed machine having precision of 10 gms. Length was measured by infantometre. Head circumference was measured with non stretchable measuring tape. Infant’s age was assessed by using New Ballard score and it was further correlated with last menstrual period and Ultrasonic measurements taken antenatal period. New born were classified as SGA = small Gestation age and AGA = Appropriate for Age on the guidelines of Alexander and associates intrauterine growth curves. The ponderal Index was calculated from these babies. The duration of study was about two years (February 2018 to January 2020). Statistical analysis: fetally Malnourished, Nourished were categorised. Parameters of ponderal index was also categorised with percentage. The statistical analysis was done in SPSS software. The ratio of male and female newborn was 2:1 OBSERVATION AND RESULTS Table-1: Signs of clinical assessment in new born (CAN) 12 (4%) Hair, 6 (2%) Cheeks, 4 (1.3%) Neck and Chin, 3 (1%) Arms, parameters are similar Legs like arms 4 (1.3%) Back, 4 (1.3%) Buttocks, 4 (1.3%) Chest, 2 (0.66%) Abdomen. Table-2: In AGA group – 16 (5.3%) were FM, 169 (56.3%) were Nourished; Total neonates were 185 (61.6%). In SGA group – 75 (25%) were FM, 40 (13.3%) were nourished, Total neonates 115 (38.3%). Table-3: In comparative study of Ponderal Index and CAN score – In Ponderal Index < 2.2, 19 (6.33%) were FM, 66 (22%) were Nourished and total neonates were 85 (28.3%). In pondering Index > 2.2, 20 (6.6%) were FM, 165 (55%) were nourished and total neonates were 215 (71.6%). Weight – Mean birth weight was 2.74 (SD 0.38) kilogram (kg) Length – Mean length was 48.9 (SD±1.89) centimetre (cm) Head circumference was 34.09 (SD±0.3) centimetre (cm)
Table 1: CAN Score (Total No. 300)
Out of nine parameters only eight were significant Table 2: Study of SGA and AGA in Fetally malnourished and nourished neonates
SGA = Small Gestation Age; AGA = Appropriate for Age; FM = Fetally Malnourished
Table 2: Study of small for Gestage Age, Average, appropriate age in Fetally malnourished and nourished neonates
Table 3: Comparative study of CAN score and ponderal Index (Total No. of Neonates – 300)
Table 3: Comparative study of CAN score and ponderal Index
DISCUSSION In the present clinical assessment of Fetal Malnutrition (FM) in Andhra Pradesh population. The CAN study assessment 12 (4%) hair, 6 (2%) Cheeks, 4 (1.3%) Neck and Chin, 3 (1%) parameters of legs like arms are similar, 4 (1.3%) Back, 4 (1.3%) Buttock, 4 (1.3%) Chest, 2 (0.66%) Abdomen. (Table-1). In AGA group – 16 (5.3%) were FM, 169 (56.3%) were nourished. In SGA group – 75 (25%) were FM, 40 (13.3%) nourished, (Table-2). In the comparison of PI (<2.2) and CAN score – 19 (6.33%) were FM, 66 (22%) were nourished. In PI (>2.2) and CAN score – 20 (6.6%) were FM, 165 (55%) were nourished (Table-3). Mean birth weight was 2.74 kg (SD±0.38), Mean length was 48.9 cm (SD±1.89) mean circumference was 34.09 cm (SD±0.3) These findings are more or less in agreement with previous studies (5) (6) (7) It was reported that majority of the FM infants with handicaps including spastic diplegia, seizures, visual problems, learning disabilities or mental retardation (8). Moreover about three fourths of neonates with FM death occur in first week of life (9).The root cause of FM is poverty and illiteracy mainly in rural part of India and neonates born in these populations are expected to be the vulnerable to FM, morbidity and mortality (10). Ponderal Index relies on principles of length is spared at the expanse of weight during period of acute malnutrition.
SUMMARY AND CONCLUSION In the present study of clinical assessment of FM in Andhra Pradesh CAN scoring is gold standard method to diagnose FM, but this study demands further nutritional, genetic and patho-physiological studies moreover balanced diet or proper nutrition in pregnant women plays vital role because without proper nutrition genes stop functioning called “Silenced genes”. It requires creating awareness by medico-social workers in rural India. This research paper was approved by Nimra Institute of Medical Sciences Jupidi, Vijaywada, Krishna district Andhra Pradesh-521456.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home