|
Table of Content - Volume 19 Issue 2- August 2021
A study of etiological factors and associated co morbidities in children with cerebral palsy
Shivprasad Kachrulal Mundada1, Deepak Khushalrao Jaybhaye2*, Vikas Narayan Solunke3
1Professor and HOD, 2PG Resident, 3Associate Professor, Department of Pediatrics, Vilasrao Deshmukh Government Institute of Medical Sciences, Latur, Maharashtra, INDIA. Email: djaybhaye7@gmail.com
Abstract Background: Cerebral palsy (CP) is a disorder of the development of movement and posture causing activity limitation that are due to non-progressive disturbances that occurred in the developing fetal or infant brain. Aim and objective: To study the etiological factors and associated co morbidities in children with cerebral palsy Methodology: Present study was a prospective observational study carried out at tertiary health care centre during October 2017 to September 2019. 84 consecutive diagnosed cases of cerebral palsy from tertiary care centre were studied from Department of Paediatrics, outpatient and inpatient. Etiological factors and associated co morbidities of CP children were noted. Data was analysed with appropriate statistical tests. Results and Discussion: Maximum patients were 2-5 years of age at the time of presentation. Male-female ratio with male being slightly more but the difference was not significant. Perinatal asphyxia found to be most common cause for CP. Speech and language delay (89.2%), orthopedic problem (77.3), visual problem (55.9%), respiratory problem (47.6%), gastrointestinal problem (35%), dental problem (26.1%), hearing impairment (21.4%), sleep disorder (5.9%) were the commonest comorbidities in children with CP.
INTRODUCTION Cerebral palsy is a disorder of motor control due to a static lesion of the developing brain. It was coined 150 years ago 1 and is familiar to both the lay and medical communities. Cerebral palsy (CP) is the most common type of motor disability in childhood. It’s incidence in India is around 3 cases per 1000 live births. CP is a common developmental disability first coined by William Little in the 1840s.2 Cerebral Palsy describes a group of disorders of the development of movement and posture causing activity limitations that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The maximum age limit for brain injury is generally 3-5 years of age. Up to 2 years of age diagnosis of CP should not be made because some minor tone abnormalities that can be present during infancy can disappear as the child grows. But in children less than 2 years of age the diagnosis of CP can be made if the child is severely involved or child has other supporting evidence (e.g. neuroimaging studies). Newer brain imaging modalities are useful to know the extent of the underlying brain injury and studies on the neurobiology and pathology associated with brain development also helps to know the various etiologies of CP. Improvement in obstetric and advanced prenatal care had resulted in increased survival of low birth weight babies and is related with an increased incidence of cerebral palsy in these babies.2 The motor disorders of cerebral palsy are accompanied by disturbances of sensation, perception, cognition, communication and behaviour by epilepsy and by secondary musculoskeletal problems.3 Complete evaluation of a child with CP therefore should include an assessment of associated deficits such as vision, speech, hearing, sensory profile, oro-motor evaluation, epilepsy and cognitive functioning. CP is a chronic condition having considerable impact on affected individuals. Early diagnosis and comprehensive management with a multidisciplinary approach with the help of pediatrician, neurologist, orthopaedic surgeon, speech and language therapist, physio and occupational therapist are required for satisfactory management of a child with CP.4 As CP is a continuing problem it is important to study the various causes and newer aspects of the condition for proper understanding and management. In developed countries, CP registers have made substantial contributions to our understanding of CP. However, in developing countries there are gaps in knowledge especially in view of epidemiological research, intervention and service utilization.4 Present study was conducted to study the etiological factors and associated co morbidities in children with cerebral palsy. Aim and objective: To study the etiological factors and associated co morbidities in children with cerebral palsy
MATERIAL AND METHODS Present study was a cross sectional study carried out at Department of Paediatrics at a tertiary health care centre during October 2017 to September 2019. Study population was patients with cerebral palsy from pediatric OPD and inpatient wards at the tertiary health care centre. Inclusion criteria: 1. All patients of cerebral palsy attending the department of Pediatrics 2. Children up to 12 yrs of age. Exclusion criteria: 1. Children with non-central causes of motor deficits 2. Parents of those children not willing to participate in the study Study was approved by ethical committee of the institute. A valid written consent was taken from the parents of children after explaining study to them. Total 84 children were studied. Data was collected with pretested questionnaire. Data included demographic data like age and sex of neonates. Following features were considered for the diagnosis of CP: 1) The disorder is present since birth or early infancy. 2) The disorder is non-progressive and non-hereditary. 3) Presence of impairment of neurological function, especially voluntary motor activity. Early markers of CP like Delayed social smile, Persistence of primitive reflexes beyond 6 months, Persistence of asymmetric tonic neck response, Decreased head circumference, Excessive extensor tone(dystonia). Delayed developmental milestones, Persistence of asymmetry in posture, movement and reflexes were noted. Associated signs in CP children, Visual problems, roving eyes, no visual following, persistent squint. Lack of auditory response were also noted. Clinical diagnosis of Cerebral palsy was made by risk factors, regular developmental screening of all high risk babies and CNS examination. Systematic approach focusing on obstetric and perinatal history, developmental milestones and a thorough neurological examination and observation of the child in various positions such as supine, prone, sitting, standing, walking and running was made. Data was entered in Excel sheet. Data was analysed with SPSS version 22.
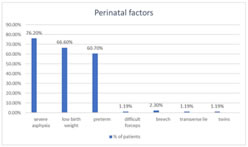
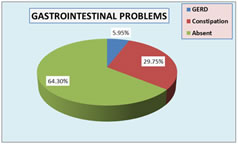
RESULTS In our study, majority of the patients were from the age group of 2-5 years (52%) followed by < 2 years and > 5 years (24% each). In this study male patients (55.95%) were more than female (44.05%). risk factor was maternal age <20 and above 35 years (32.1%) followed by (PIH) Pregnancy Induced Hypertension (25%). Consanguineous marriage was observed in 9.5 % of mothers. Bleeding was observed in 2.3%. Infection and trauma was observed in 1.19% mothers each. Spastic cerebral palsy was the commonest physiological type of cerebral palsy (90%) followed by athetoid type (8%). Atonic (1%) and dystonic (1%) types formed the rest of the cases. Fig 1 shows Distribution of CP children according to perinatal factors. In our study, most commonly observed perinatal factor was birth asphyxia (76.2%) followed by Low birth weight (66.6%). Preterm babies were 60.70%. Malpresentations like breech (2.3%), transverse lie (1.19%) was observed in less patients. 1.19% of babies were delivered by forceps delivery. 1.19% patients were twins. In our study, neonatal hyperbilirubinemia (15.4%) was most commonly observed postnatal factors followed by neonatal septicemia (9.5%). Meningitis was observed in 8.3% neonates. 5.9% neonates suffered from convulsions. In our study we studied associated comorbidities in CP children. Speech and language (89.2%) was most commonly affected followed by orthopedic (77.3%), vision (55.9%), epilepsy (47.6%), respiratory (47.6%), gastrointestinal (35%), dental (26.1%), hearing impairment (21.4%), sleep (5.9%), were other common problems. (table 4) Among 84 children with CP, 30 had gastrointestinal problem. Most common being constipation (29.75%) and GERD (5.95%). (fig 2) Our Study revealed that (55.9%) had visual problems. Refractory errors were commonest (30.95%), strabismus (11.9%), optic atrophy (5.95) and nystagmus (4.76%). (table 5) Table 1: Distribution of children according to age
Table 2: Distribution of CP children according to perinatal maternal risk factors
Figure 1: Distribution of CP children according to perinatal factors
Table 3: Distribution of children according to postnatal factors
Table 4: Distribution of children according to associated co morbidities
Figure 2: Distribution of children according to associated gastrointestinal problems
Table 5: Distribution of children according to associated visual impairment
DISCUSSION In this study maximum number of patients were of age group 2-5 years. Analytical study by Kondle et al. also showed most patient presented at age of 1-5 years. This is because during this period developmental retardation becomes more obvious and parents become worried and the child is brought to the hospital.5 This study showed that incidence of CP is more in males as compared to females. A high incidence of male sex has been reported by Kondle et al.5, Nabanita Das et al.6 and is consistent with this study. Early treatment or consultation for male child and negligence for female child can be one the factor. In present study perinatal asphyxia was the most common perinatal risk factor while maternal age and meningitis were natal and postnatal risk factors. Similar observation was found in study by Nabanita Das et al. 6 and Anant Bendale et al.7 Study by Nabanita Das et al.6 showed asphyxia and difficult deliveries are more common in spastic quadriplegia, prematurity and LBW in spastic diplegia and neonatal hyperbilirubinemia in athetoid CP. These findings were consistent with this study. A high incidence of prematurity is seen in diplegics. This association is due to the fact that certain periventricular vascular structures make this region vulnerable to ischemia. The pressure-passive cerebral circulation of preterm infant, particularly when sick and generally depressed in state. The enhanced vulnerability of the actively differentiating and/or myelinating periventricular glial cells. Other risk factors like malpresentation, abnormal labour were not found in this study but these were showed in study by Kondle et al.5 because the study population in their study was higher as compared to this study. Role of perinatal complications, particularly birth asphyxia has been implicated strongly in developing countries. CNS infection, neonatal septicaemia, neonatal hyperbilirubinemia, neonatal hypoglycaemia and vitamin k deficiency associated intracranial bleeds constitute important preventable causes of acquired CP in the developing world.8 Spastic cerebral palsy was the commonest physiological type of cerebral palsy (90%) followed by athetoid type (8%). Atonic (1%) and dystonic (1%) types formed the rest of the cases. In this study among the spastic group, quadriplegias were 55%, diplegia 22%, monoplegia 1% and double hemiplegia 12%. There are other comparable studies Kondle et al.5, P.Singhi et al. 8, Bendle et al.7 showed spastic cerebral palsy was the commonest type. Refractive error (30.9%) was most common type of abnormality documented in this study similar to study by Marasani et al.9 In contrast study by Govinda et al.56 found strabismus to be most frequent abnormality. Many literature including Govinda et al.10 quotes a higher prevalence of hyperopia in CP but our study did not agree with the prior studies. Instead, present study showed myopia (18.2%) occurred to greater extent than hyperopia (12.7%). The higher prevalence of refractory error even in lower age group suggests the emmetropization process may have been hampered. Respiratory problems were present in 47.6% of the children. Aspiration pneumonia, repeated upper respiratory tract infections, pneumonia were the common problems. Chest expansion was decreased in spastic CP patients due to decrease in chest mobility when compared with normal children of similar age and gender. Chest expansion was significantly decreased on CP subgroups according to type of involvement, mental status, grade of spasticity and level of ambulation. For chest expansion normal function of nervous system, respiratory muscles and costovertebral joints are needed as CP does not have articular involvement the limited chest mobility may be due to impaired neuromotor control and co- ordination, weakness, spasticity and secondary changes in the respiratory muscles. This limited chest mobility lead to stiffening of costovertebral joints which may also decrease chest expansion.11 According to some authors children with CP behave like patients with obstructive lung disease although they no signs of obstruction. This may be the result of neuromotor disturbance which caused inability to force the thorax back to normal size and/ or may be due to at least in part to some degree of obstruction of the upper airways because of the improper posture of thorax, neck and head. Inco-ordinated laryngeal opening with diaphragmatic activity may be another possible cause of airway obstruction. Aspiration with or without gastroesophageal reflux may be causative factor for obstructive respiratory dysfunction in CP. The possible explanation of uniform decrease chest expansion in all CP subgroups may be the limited physical activity.11 In this study, 36% of patients had gastrointestinal problems, the most common being constipation (30%) and GERD (6%). In study by Vishnu Prasad et al.12, constipation (52%) commonest among the children with CP. The study revealed that 89.2% of these CP children had speech and language delay. In the study by P. D. Singhi et al. 8 speech disorders were 78%. Another study done by Srivastava VK et al. reported speech problems in 37% children. 13 Speech disorders in study by Vishnu Prasad et al. were reported 60%.12 Hearing impairment was present in 21.4% of children. The study by P. D. Singhi et al. 8 reported hearing disorder 14% and 2.9% in study by Srivastava VK et al.13 Occurrence of hearing impairment was slightly higher than these studies might be because of about 60% of cases were preterm in this study. Orthopedic problem was present in 77.3% of children. Most of the children had deformity and joint contracture. Hoffer et al.14 reported that contractures in cerebral palsy usually in flexion at the hip and knee and in plantar flexion at the ankles which is similar to this study.
CONCLUSION Perinatal asphyxia found to be most common cause for CP. Speech and language delay, orthopedic problem, visual problem, respiratory problem, gastro intestinal problem, dental problem, hearing impairment, sleep disorder were the commonest comorbidities in children with CP.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home