|
Table of Content - Volume 19 Issue 2 - August 2021
Assessment of clinical profile and radiological finding in cases of cerebral palsy
Ramchandra Nagargoje1*, Ramesh Lomte2, Mona Gajre3, Sambhaji Chate4, Arpita Thakkar5
1,2Assistant Professor, 4Professor, Department of Paediatrics, SRTR Government Medical College, Ambajogai, Beed, Maharashtra, INDIA. 3Professor, 5Associate Professor, Department of Paediatrics, Lokmanya Tilak Medical College, Sion, Mumbai, Maharashtra, INDIA.
Abstract Background: Cerebral palsy (CP) is one of the leading causes of childhood disability worldwide with the greatest burden found in developing countries like India. The present study was undertaken to study the clinical profile, seizure, semiology and EEG finding in CP patients and its correlation with MRI. Method: Total 104 children of age 3month to 12years with CP attending paediatric Neurodevelopmental OPD and CP Clinic were enrolled in the study. A detail history was taken, demographic profile, birth details, clinical presentation, clinical examination (general and CNS), GMCSF level, MRI and EEG findings were noted. Results: The mean age of child was 5.4years for preterm and 4.06year for term whereas mean birth weight for preterm and term child was 1.68kg and 2.7kg respectively. Birth asphyxia was the commonest etiological factor seen in overall 63.5% cases, of them 60% preterm and 65.2% term children. Most common type of CP was spastic quadriplegic found in 57.9% preterm and 53% term children. Most of the preterm children were at GMFCS level I (42.1%) while majority of term child at GMFCS level IV (25.8%). EEG was abnormal in 14.4% of patients, preterm had incidence of 2.6% and term had incidence of 21%. Commonest MRI finding was periventricular leucomalacia (PVL) found in 44.7% of preterm and 33.3% in term children. Conclusion: In the present study, MRI positivity was seen in 96.15% of cases; hence MRI was useful in revealing underlying brain abnormalities in children with CP. Also, MRI helps in knowing the pathological basis of disease, but clinical findings carry utmost importance. Keywords: Cerebral palsy; Semiology; Seizure; Neurodevelopmental; Preterm; Term; Birth asphyxia; Spastic quadriplegic; GMFCS; MRI
INTRODUCTION Cerebral palsy is diagnostic term used to describe a group of permanent disorder of movement and posture causing activity limitation; that are attributed to non-progressive disturbances in developing foetal or infant brain1 The motor disorder often accompanied by disturbances of sensation, perception, cognition, communication, and behaviour as well as epilepsy and secondary musculoskeletal problem.2 CP is caused by group of developmental, genetic, metabolic, ischemic, infectious, and other acquired etiologies that produce a common group of neurologic phenotype.3 The incidence and prevalence of CP varies by region, population, age, severity, which may limit the generalize ability of population based limits. Recent advances in neonatal management and in obstetric care have not shown decline in the incidence of CP, on contrary, with decline in infant mortality rate, there is actually increase in incidence and severity of CP.4 Neuropathology identified by MRI corresponds well with clinical description of motor impairment in children with CP. The principal contribution of imaging to the understanding of etiology and pathogenesis including ruling in and out that may have implication for genetic counseling such as malformation.5 However, MRI will help to know the etiology; severity of CP. Gross motor function classification system [GMFCS] is used to know the severity of cerebral palsy. MRI finding may help in case at which age child requires orthoses or any other intervention. It will be a good tool to explain the nature of disease to parent, i.e. parental counselling.6 Hence the present study was undertaken to investigate the clinical profile, seizure, semiology, grading of CP as per GMFCS, also to study the disorders of white matter development, neuronal migration defects as well as EEG finding in cerebral palsy children and its correlation with MRI.
MATERIALS AND METHODS After obtaining Institutional Ethical Committee approval, this prospective observational study was conducted in the Department of Paediatrics at Tertiary Care Institution during a period of one year from December 2014 to November 2015. Total 104 children of age 3 month to 12 years with cerebral palsy attending paediatric Neurodevelopmental OPD and Cerebral Palsy Clinic were enrolled after informed consent obtained from parents. Children or parents not consenting to the study and those children with other neurodevelopmental disorders such as autism, learning disability were excluded from the study. Detail history was obtained from patients and their demographic profile (age of child, number of male and female children, and their birth weight), birth details ((history of birth asphyxia) and clinical presentation was entered in a preformed case Performa. Clinical examination included general and CNS examination were done. Type of the cerebral palsy (motor classification and topographical classification), grading of cerebral palsy as per gross motor function classification system (GMFCS), whether epilepsy present or not, radiological magnetic resonance imaging (MRI) findings, electroencephalograph findings and lastly any other significant finding also were noted. All these parameters were compared in preterm and term cerebral palsy children. Statistical Analysis The data were collected and analyzed using appropriate SPSS software or by applying the Chi-Square test as per the feasibility. We calculated the percentage of linear variables, and proportions for the categorical variables. The means between two groups were compared using t-test. The proportions were compared using the chi square test or the T test. A p-value of less than 0.05 was considered to be statistically significant.
OBSERVATIONS AND RESULTS Total 104 patients with CP were enrolled in the study, of them 57 (54.8%) were males and 47 (45.2%) were females. Out of 104 patients, 38 patients were born as preterm whereas 66 patients were born as term. The demographic data of the patients with CP are shown in table 1. Table 1: Demographic profile of the patients
Overall incidence of birth asphyxia was 63.5%; of them 60% were preterm and 65.2% term children. The overall percentage of epilepsy was 28.8%. Epilepsy in preterm and term group was 26.3% and 30.3% respectively. The cerebral palsy children who were born as preterm had better gross motor function (42.1%) in level I of GMFCS as compared to those who were born as term (19.7%) in level I, (p=0.064) as depicted in figure 1.
Figure 1: Distribution of preterm and term in GMFCS The most common type of CP was spastic quadriplegic found in 57.9% preterm and 53% term children. Second predominant CP in term children was spastic hemiplegic (24.2%) while in preterm was Spastic diplegic found in 21.1% as shown in table 2.
Table 2: Type of CP (motor and topographical) in preterm and term
EEG was abnormal in 14.4% of patients. Preterm had incidence of 2.6% and term had incidence of 21%, (p value=0.009). The most common MRI finding was periventricular leucomalacia (PVL) found in 44.7% of preterm and 33.3% in term children followed by subcotical lesion (SCL) found in 13.2% of preterm and 19.7% in term as shown in table 3.
Table 3: EEG and MRI finding in preterm and term CP children
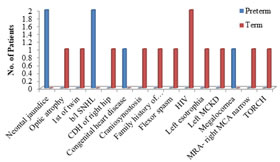
One case CP who was born as term was Craniosynostosis. CP who had history of neonatal jaundice were 2 cases, both were preterm, one requiring exchange transfusion. Other important significant findings in patients with CP are depicted in figure 2. Figure 2: Other significant finding in cerebral palsy patients
DISCUSSION Cerebral palsy is the commonest cause of physical and mental disability in children. It can affect both genders; however, boys are affected slightly higher than girls. In present study also males were higher than female child which is comparable with the other studies done in India.7-9 High incidence may be due to the better attention given to male child to seek medical help in Indian scenario. Spastic quadriplegic CP has been shown to be the commonest form of CP in various studies conducted in developing countries.10 Spastic diplegic CP has been reported as the commonest type in developed countries.11 In the present study, preponderance of spastic quadriplegic CP was noted accounting for 54.80% this finding is similar with previous studies.7, 9, and 12 This decrease in spastic quadriplegia in developed countries has been attributed to reduction in perinatal mortality rate and also the increase in survival rates of extremely premature and low birth weight babies. The role of perinatal asphyxia was found to be the major etiology in current study accounting for 63.5%, of which 60% of preterm and 65.2% of term children. This result is similar to the study done by Singhi et al.10 The most useful development in the classification of CP in recent years has been the development of the Gross Motor Function Classification System (GMFCS). The GMFCS is a five-level ordinal grading system based on the assessment of self-initiated movement with emphasis on function during sitting, standing and walking. Distinctions between different levels are based on functional limitations, the need for walking aids or wheeled mobility and quality of movement. Unlike the classification of motor type and topography, the GMFCS has been shown to be a valid, reliable, stable and clinically relevant method for the classification and prediction of motor function in children with CP between the ages of 2 and 12 years.13 One of international article, cerebral palsy in Victoria studied by Jason Howard et al.13 which has focused on gross motor function of CP child has findings given in table 4 while in current study, we have studied gross motor function separately in preterm and term and also combined as shown in below table.
Table 4: Comparison of other studies findings with current study
Epilepsy occurs in 25-45% of children with CP. According to Wallace, seizures are mainly of the symptomatic nature. If children with CP have difficulties in learning at the same time, the risk of also having epilepsy increases up to 71%. It is estimated that among children with CP only 10-32% will develop epilepsy, among children with mental impairment only 10-29%, and co-occurrence of CP and the impairment is associated with 50% risk of epilepsy. In Wallace’s opinion, epilepsy is more frequent in some forms of CP, e.g. it accompanies hemiplegia in 33-50%, where focal seizures dominate (69-73%).15 In present study overall percentage of epilepsy including preterm and term was 28.8%. There were 26.3% of patients in preterm group had epilepsy while in term group 30.3% of children had epilepsy. This finding matches with occurrence of epilepsy in CP (25-45%) as mentioned above. EEG was abnormal in overall 14.4% of patients of them 2.6% were preterm and 21.2% term patients which was statistically significant (p value=0.009). It means children with CP, when investigated for EEG, getting it as abnormal was more in term than preterm. As per study done by Ashwal et al., an EEG should not be obtained for the purpose of determining the etiology of CP (Level A; class I and II evidence). An EEG should be obtained when a child with CP has a history or examination features suggesting the presence of epilepsy or an epileptic syndrome (Level A; class I and II evidence).16 The pattern of brain injury of patients with CP is closely related to the gestational age of occurrence. Typical preterm brain injuries include PVL and post-haemorrhagic porencephaly. PVL usually occurs between 28 and 34 weeks of gestation and is caused by an ischaemic process in the watershed zone that exists in the periventricular white matter of the immature brain. The MRI features of PVL include a reduction in the quantity of periventricular white matter (late infancy and childhood), periventricular gliosis and ventriculomegaly with irregular outline of the lateral ventricles. After about 34 weeks of gestation, subcortical and cortical areas are the most vulnerable regions of the brain for hypoxic ischaemic insult and the resulting lesions include subcortical leucomalacia, multicystic encephalamalacia and gliosis.17 Commonly observed in preterm infants and full-term children with suffocation, PVL is a significant manifestation of infant brain injuries. PVL is the main cause of infant mortality; patients who survive suffer from nervous system disorders and mental retardation later in life. The pathogenesis of this condition has been linked to perinatal inflammation and/or hypoxia‑ischemia. Ischemia/reperfusion results in the formation of reactive oxygen species and reactive nitrogen species, causing cell death.18 In addition to early mortality due to the poor prognosis of PVL, 50% of the sequelae from cerebral palsy (CP) are related to the manifestation of PVL in survivors.19 Studies have shown that PVL is an independent risk factor of CP.20 CP is characterized by a group of developmental processes involving movement and posture; as a result, activity is limited and this finding is attributed to non‑progressive disturbances that occur in the developing foetal or infant brain.21 CP is a serious disorder in children and influences the survival and quality of life of infants. However, at present, no specific treatment is available to alleviate PVL; hence, the prevention of various risk factors associated with PVL is necessary. Shang et al. had done clinical study in cerebral palsy in 408 children with periventricular leucomalacia and it is found that 36.76% of the children had a gestational age of ≤32 weeks and 37.75% had a gestational age of ≥37 weeks. Severe PVL was observed in preterm infants (63.41% with a gestational age of <28 weeks and 21.95% with a gestational age of 28-30weeks).22 In present study, out of 38 preterm patients, 44.7% patients had PVL, 5.3% patients had PVL with SCL, cystic encephalomalacia in 5.3% and gliosis and infarct along with germinal matrix haemorrhage was 7.9% patients and SCL lesion, involvement of sub-cortex which includes basal ganglia lesion, involvement of thalamus; was found in 13.2 % of preterm. There were 2 cases noted which was due to the neonatal jaundice causing kernicterus. Involvement of basal ganglia was there. One patient had received exchange transfusion also. These findings are correlated with the study done by Ashwal et al.16 and the difference found in results may be due to less number of preterm in current study. In cases of term child, MRI finding PVL was 33.3%, Gliosis, infarct or germinal matrix haemorrhage was 16.7%. SCL in term children was 19.7%, cystic encephalomacia 7.6%, PVL with SCL was in 3%. Overall incidence of MRI finding was as-PVL was 37.5%; gliosis, infarct, germinal matrix haemorrhage was 13.5; SCL was 17.3%; cystic encphalomalacia was 6.7% and PVL with SCL was 3.8%. Out of 104 patients 4 patients had normal MRI finding. One patient was preterm born with spastic diplegic CP; other three were born as term. In this term children two were spastic hemiplegic CP cases without epilepsy and one was spastic diplegic with abnormal EEG pattern. There were 6.7% as miscellaneous group which does not fit in above groups. These findings are in accordance with the study done by Krägeloh-Mann et al.17 Cortical malformation in our study was 10.6% which is comparable with the previous studies23 of 10.6% cases, preterm were 13.2% and; 9.1% term babies. We also noted other significant finding. Two preterm patients with neonatal jaundice, of which one had required exchange transfusion. One with optic atrophy, one CP was first of the twin delivery; both were term children. Bilateral sensory neural hearing loss was found in 2 preterm patients. One term child had congenital dislocation of right hip. Another preterm born child was diagnosed as case of craniosynostosis. In one term CP child there was family history of other child (sibling) in spite of birth history normal in both the children. Genetic may be the cause in this scenario. One term child was with flexor spasm and two other patients were known cases of HIV positive. One term child had left esotrophia, another term child had left multi-cystic kidney disease. One preterm was with megalocornea whereas another preterm, on investigation found to have right middle cerebral artery narrowing. One term child was TORCH group of infection.
CONCLUSION In the present study, MRI positivity was seen in 96.15% of cases; hence MRI was useful in revealing underlying brain abnormalities in children with CP. Also, MRI helps in knowing the pathological basis of disease, but clinical findings carry utmost importance. Specific MRI findings in children with CP were found to be associated with neurological subtype and gestational age at birth. Because of the assessment of recurrence risk, counselling of families and potential implementation of prevention strategies, all children with CP should have age-appropriate MRI of the brain. Moreover, for parents seeking a cause for their child’s disability, a radiological diagnosis is now possible in the majority of cases. However, this radiological diagnosis may not necessarily provide information as to why the brain lesion occurred. Important evidence for the timing of the brain lesion may be provided which can be useful not only for individuals but for directing research efforts in the future.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home