|
Table of Content - Volume 21 Issue 2 - February 2022
Thyroid profile in critically ill children and its effect on the clinical outcome
Joewin Monteiro1*, Jyotirmanju2, Vanitha Gowda3
1Senior Resident, Department of Paediatrics, Rajarajeswari Medical College, Bengaluru, Karnataka, INDIA. {2Associate Professor, Department of Paediatrics} {3Professor, Department of Biochemistry} Ramaiah Medical College, Bengaluru, Karnataka, INDIA. Email: joewinmont@gmail.com
Abstract Background: Various endocrine axes respond in varied manner in stressful conditions. The adjustments taking place because of those variations assist the body to keep homeostasis. The endocrine changes might also overshoot the bounds in a few people leading to deleterious consequences. Few studies have reported that the low thyroid hormones are independent predictors of mortality in patients admitted to intensive care units. Surprisingly, very constrained records exists from India concerning the endocrinological parameters in critically ill children and for this reason we carried out this prospective observational study to evaluate the thyroid hormone profile in terms of survival in children admitted to PICU. Aims and Objectives: To assess serum levels of serum T3, T4 and TSH and their role in recovery and duration of hospital stay in sick children. Methodology: This study was conducted in Department of Paediatrics, in a tertiary care hospital, during the period of Oct 2017 to May 2019. It was an observational study. Samples of 85 patients who satisfied the inclusion criteria were analysed. Children were categorised into 2 groups based on the PRISM-II score. Co-relation of thyroid profile and clinical outcome and duration of stay in PICU and hospital was done. Results: Low T4 was noted among all 85 children. T4 levels had a significant co-relation with mortality and duration of hospital stay in children with PRISM-II score >5. Higher levels of T4 and T3 levels at admission was associated with higher risk of mortality among children with higher PRISM-II score. Conclusion: This study shows that T4 levels had a significant co-relation with mortality and duration of hospital stay in children with PRISM-II score >5. Higher levels of T4 at admissions was associated with increased risk of mortality and decreased duration of hospital stay. Higher T3 levels at admission was associated with higher risk of mortality among children with higher PRISM-II score.
INTRODUCTION Various endocrine axes reply in varied manner in stressful conditions. The response is complex and assists the body to keep homeostasis. Changes in the levels of thyroid hormones, sex hormones, and corticosteroids are the predominant changes in critical illness.1 The endocrine alterations may overshoot the boundaries in some individuals leading to deleterious consequences.2 Thyroid hormones play a major role in the maintenance of body growth by modulating metabolism and the immune system. Critical illness is regularly associated with alterations in thyroid hormone concentrations in patients with no preceding intrinsic thyroid disease. The abnormal thyroid activity is referred to as euthyroid sick syndrome (ESS) or non-thyroidal illness syndrome (NTIS). Euthyroid Sick Syndrome (ESS) is the commonest endocrine change seen in critically ill patients.3,4 Patients present with low serum levels of free triiodothyronine (fT3) and thyroid-stimulating hormone (TSH), and low or normal levels of free thyroxine (fT4).5 Also, high levels of reverse T3 (rT3) are observed in nonthyroidal illness due to the reduced conversion of rT3 to diiodothyronine (T2) due to the inhibition of 5’-monodeiodinase activity.6 The impairment of 5’ deiodinase may be due to reduced availability of the enzyme co-factor glutathione due to reduced intake of carbohydrates.7 Stress induced elevated steroids in the body also inhibit T4 to T3 conversion.8 Serum T4 is reported to fall in proportion to severity of illness. The magnitude of T4 level decrease was found to correlate with patient’s outcome in many studies. Few studies have reported that the low thyroid hormones are independent predictors of mortality in patients admitted to intensive care units. Surprisingly, very constrained records exists from India concerning the endocrinological parameters in critically ill children and hence we performed this prospective observational study to assess the thyroid hormone profile in relation to survival in children admitted to PICU. OBJECTIVES: 1. To assess serum levels of serum T3, T4 and TSH and their role in recovery and duration of hospital stay in sick children. 2. Correlate the initial levels of serum T3, T4 and TSH with mortality (if any) in these children.
METHODOLOGY After clearance from the ethical committee and due consent from the parents, consecutive paediatric patients aged between 1 month to 18 years admitted to PICU at MS Ramaiah Medical college Hospital fulfilling the inclusion criteria were recruited into the study. This study was conducted between October 2018 to May 2020. Critically ill was defined as any child who on initial admission had a PRISM-II score of ≥5. Children with records of previous thyroid illness/ on iodine containing drugs/ family history of thyroid ailments have been excluded from the study. 3ml of blood was collected soon after admission, with due aseptic precautions in plain vacutainer tubes. Serum TSH, Serum T3 and Serum T4 were measured by enzyme linked immunosorbent assay[ELISA] method, using ELISA kits manufactured by Calbiotech on the ELISA Reader. The reference ranges used were provided by the ELISA Kit manufacturer. Other investigations like CBC, SGOT, SGPT, Serum Albumin, Serum Electrolytes and Serum Creatinine that were a part of the management protocol for all critically ill cases were done using automated analysers- Roche COBAS 6000 analyser in the clinical Biochemistry Section. Serum T3, T4 and TSH of all subjects were assessed. Correlation between Serum thyroid levels and clinical diagnosis of the patients was studied. Any relation between the serum thyroid levels (T3, T4 and TSH) and clinical outcome was looked for. All the quantitative variables were summarized using descriptive statistics such as mean and standard deviation. All the qualitative variables were summarized using frequency and percentage. Statistical analysis was done using Fisher Exact test. p value of <0.05 was considered statistically significant.
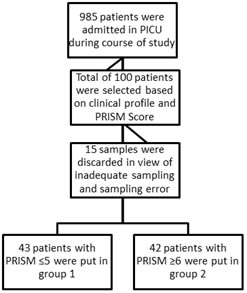
RESULTS This study was conducted at M S Ramaiah Hospital during the period of Oct 2017 to May 2020. 100 critically ill children out of 985 who were admitted to RMCH PICU and met the criteria were enrolled into the study. 15 samples were excluded in view of inadequate samples and sampling error. A total of 85 samples were analyzed at the end of the study. Patients were divided into 2 groups based on PRISM-II score. PRISM-II Patients with PRISM-II score of ≤5 were put in group 1 and ≥6 were put in group 2. Figure 1 Children aged between 1 month to 18 years were included in the study. They were further divided into following age intervals Table 1: Showing distribution of cases according to the age interval
Out of 85 children between age group of more than 1 month to 15 years studied, 22 (26%) were between 1month – 1year, 28 (33%) were between 1-5 years, 17 (20%) were between 6-10 years and 18 (21%) were between 11-18 years. Among 85 children 25 (29.4%) had CNS involvement, 18 (21.2%) had respiratory system involvement, 9 (10.6%) had gastrointestinal involvement, 3 (3.5%) each had cardiovascular and endocrinal involvement. Of the 85 patients admitted 61 patients were discharged, 11 went against medical advise and 13 deaths were noted. Among 85 patients 72 had low TSH levels and 13 had normal TSH levels, 19 had low T3 levels and 62 had normal T3 levels. TSH among group 1 was low in 38 children and normal in 5 children. T3 among group 1 was low in 3 children, normal in 23 and high in 2 children. TSH among group 2 was low in 34 and normal in 8 children. T3 among group 2 was low in 11, normal in 29 and high in 2 children. All 85 children had low T4 levels. There was no statistically significant difference between T3, T4, TSH levels among 2 groups. Table 2: Thyroid Profile of patients
Table 2: Shows the T3, T4, TSH values among two groups, Inter quartile ranges of thyroid hormones and p values.
Co-relation of thyroid profile with patient profile Table 3: Corelation of T3, T4 and TSH levels with clinical outcomes in Group 1
Table 3: Shows Correlation co-efficient [r] and p values of TSH, T3, T4 levels compared to Hospital stay, PICU stay and Mortality risk among patients in group 1 There was significant co-relation between T3 levels and duration of hospital stay among patients in group 1. Longer duration of hospital stay was noted among children in group 1 who had a higher value of T3 at admission.
Table 4: Corelation of T3, T4 and TSH with clinical outcome of patients in group 2
Table 4: Shows Correlation co-efficient [r] and p values of TSH, T3, T4 levels compared to hospital stay, PICU stay and Mortality risk among patients in group 2. There was significant co-relation between T4 levels and duration of hospital stay. Lower the T4 levels at admission longer the duration of stay in hospital. There was also significant co-relation between T3 and T4 levels with mortality risk. Higher T3 and T4 levels (from the the baseline in our study) at admission was associated with increased risk of mortality.
DISCUSSION Alteration in thyroid hormone is often seen in patients with critical illnesses with no prior intrinsic thyroid disease. The non-thyroidal illness syndrome, also known as the low T3 syndrome or euthyroid sick syndrome, is a condition characterized by abnormal thyroid function tests encountered in patients with acute or chronic systemic illnesses. The reason behind the decreased fT3 levels in majority of the critically ill patients with non-thyroidal illness is the inhibition of 5’-monodeiodinase which leads to decreased conversion of T4 to T3. Several factors are involved in the inhibition of 5’-monodeiodinase including cytokines, circulating deiodenase inhibitors (free fatty acids), and glucocorticoid therapy. The reduced levels of TSH and fT4 are a sign of severe chronic illness and a prognostic marker of poor outcome.5 In our study of the 100 samples collected, 85 were subjected to analysis. The rest were excluded due to sampling error and inadequate sampling. Of the 85 samples, 43 were put in group 1 and 42 were put in group 2. Children were separated into two groups based on PRISM-II score on admission. Children who had a score of more than 5 were grouped as cases and a score of ≤5 were grouped as controls. Our study demonstrated low T4 (N-85, 100%) and low TSH (N-72, 84.7%) in the majority of the patients admitted to PICU. Subjects with low T4 levels had higher risk of mortality and morbity. Higher the baseline T4 level at admission to PICU was associated with increased risk of mortality among critically ill children (r- 0.356, p- 0.023). Low T4 levels co-related with PRISM-II score and mortality risk among critically ill children in PICU. It was also noted that serum T3 values among cases had a significant positive co-relation with risk of mortality. Suvarna JC et al. also described similar findings in their study where in Serum T4 levels in children who suffered mortality was significantly lower as compared to children who survived. Patients with combined low T3 and T4 levels had a 30 times increased risk of mortality.8 PRISM-II score at 24 hours and T4 levels can predict survival. They also noted that Low T3 and T4 values could predict mortality which was similar to the findings in our study. Our study findings were similar to the findings of study done by Kiran et al. which demonstrated low T3 and T4 levels in critically sick children.3 In our study we found that low T4 level at admission as the single most powerful predictor of mortality risk among the parameters of thyroid profile which has not been consistent with any other previous studies. Meyer et al. noted that fT4 levels decreased significantly in non-survivors which was very similar to the findings of our study.9 Anna G et al. demonstrated that T3 and T4 levels were significantly low on admission in sick children which was similar to our study. However T3 levels were borderline normal in our patients.10 Wang et al. demonstrated that T3 levels co-related well with APACHE score in adults. 11 Similar to this study, we found a significant co-relation between PRISM-II score and mortality risk. Study done by Kumar et al. showed similar findings as our study where in they demonstrated significantly low levels of T3, T4, TSH levels in critically ill children.12 Kothiwale VA et al. noted that mean fT3 and TSH levels were reduced in non-survivors as compared to survivors, with increased mean fT4 levels in the non-survivors. APACHE II score was inversely correlated with fT3 and fT4 levels. Where as in our study we noted that mean T4 and TSH levels were low in most critically ill children and T4 levels co-related well with PRISM-II scores in critically ill children.5 In our study we found that all children admitted to PICU had low T4 levels at admission. This could be due to the reason that our hospital being a tertiary care centre and a referral hospital received patients after a prolonged initial course of illness by which time the hypothalamo-pituitary axis is already suppressed and the body is unable to cope up with the metabolic needs during the illness.
CONCLUSION In our study we have noted that all 85 children enrolled in the study had a low T4 level from the baseline. 62 children (73%) had normal T3 (0.82-1.85 ng/mL), 19 children (22%) had low T3 (<0.82 ng/mL) and 4 children (5%) had high T3 (>1.85 ng/mL) levels. 72 children (85%) had low TSH and 13 (15%) had normal TSH (Age specific) at admission. This study shows that T4 levels had a significant co-relation with mortality and duration of hospital stay in children with PRISM-II score >5. Higher levels of T4 at admissions was associated with increased risk of mortality and decreased duration of hospital stay. Higher T3 levels at admission was associated with higher risk of mortality among children with higher PRISM-II score. Limitations We collected a single sample for TH assessment on admission. A paired sample at discharge from PICU or at discharge/death would have helped us to better assess the further fall or change in TH during course of illness. We did not assess free T3 and T4 levels in view of financial constraints as most studies showed significant co-relation between fT3, fT4 level and mortality.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home