|
Table of Content - Volume 21 Issue 2 - February 2022
Management of Posterior reversible encephalopathy syndrome with 8 years child with dengue fever: A case report study
Dipak Marakwad1*, Phanish Kaushik2, Ganesh Kulkarni3, Prashant Jadhav4, Rahul Bharad5
Sanjeevani Children’s Hospital & Post Graduate Teaching Institute, Aurangabad, Maharashtra, INDIA. Email: dpkmarakwad73@gmail.com
Abstract Background: We report a case of 8 years female child who was dengue NS 1 positive, presented to emergency department with altered sensorium, seizures and later on noted to have symptomatic hypertension. Patient was diagnosed with PRES on MRI and managed with anti-epileptics and anti-hypertensives. Keywords: Posterior reversible encephalopathy syndrome.
INTRODUCTION Dengue an arthropod born disease can present with mild febrile illness to disastrous Dengue hemorrhagic fever or dengue shock syndrome. It is well known that it can be associated with sequele of complications due to widespread multisystem inflammation. Central nervous system complications include encephalitis, encephalopathy, intracranial hemorrhage etc. but there are hardly some studies where pediatric patients with dengue illness presented with PRES.1
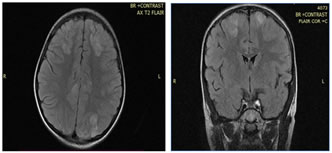
CASE REPORT An eight years female child presented to casualty with fever, pain in abdomen, vomiting since 3 days and excessive headache since 1 day. Patient was immediately shifted to critical care unit for further management. On visual examination, patient was sick looking, irritable and was complaining of excessive headache. After detailed clinical evaluation we noted that patient was having tender hepatomegaly, mild tachypnea and tachycardia, adequate volume pulse and significant hypertension (signs of volume overload). We started her on restricted IV fluids. Her recorded blood pressures were 145/100mmHg (> 99th centile for age). Patient developed generalized tonic clonic seizures lasting for 2 min that subsided with intravenous lorazepam (0.1 mg/kg). Intravenous infusion of anti-hypertensive (labetalol infusions) was started as she had persistently high blood pressure. We treated her with intravenous labetalol therapy till her blood pressure stabilized considering as symptomatic hypertension and started with maintenance intravenous antipileptic (leveteracetam). Hypertonic saline was infused to relieve cerebral edema. We then immediately started working for the evaluation of symptomatic hypertension bedside. Her two-dimensional echocardiography and renal artery Doppler study were normal. Next day after stabilization, we did MRI brain which demonstrated asymmetrical non enhancing areas of T2 and FLAIR hyperintensities noted in left parietal region, with subtle focal dural enhancement noted in left parietal region – features suggestive of posterior reversible encephalopathy syndrome. (figure 1 and figure 2)
Figure 1 Figure 2
After 3 days of intensive care, patient improved symptomatically, her blood pressures were on 55th centiles. We stopped all intravenous medications and shifted her on oral calcium channel blocker (Enalapril) and oral antiepileptic (Levetiracetam). We were able to achieve her blood pressures in normal range in the same course and patient got discharged from the hospital. Over next 6 – 8 weeks of follow up, child was neurologically stable with age-appropriate development.
DISCUSSION Despite of multiple and extensive research studies, the pathogenesis of dengue is still poorely understood.2 The primary target cells for dengue virus are dendritic cells and monocytes/macrophages that release various chemokines and cytokines upon infection, which can activate the endothelium and play a major role in dengue virus induced vascular permeability.3 It is well known that fluid resuscitation during the management of hypotensive shock in dengue may lead to fluid overload and subsequent hypertension. It is likely that there could be more such patients of dengue hypertensive emergencies with PRES that are not reported due to lack of availability of neuroimaging, inability to transport a sick baby with shock and clinical assumption that diagnosis of PRES requires hypertension to present, whereas dengue fever results in hypotension.4
CONCLUSION In children with severe dengue associated encephalopathy, PRES should be considered as a differential diagnosis, especially in those with hypertension. Neuroimaging is warranted in such cases as PRES can be identified by its characteristic findings on MRI as well as for reassurance of better prognosis, in contrast to those with dengue encephalitis.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home