|
Table of Content - Volume 3 Issue 1 - July 2016
Study etiology and clinical features of mono-articular arthritis in rural patients
Maroti Karale1*, Kailas Chintale2, Bhanudas Karale3, Paresh Patil4
1,2Assistant Professor, 3,4Jr. Resident, Department of Medicine, SRTR Government Medical College, Ambajogai, Maharashtra, INDIA. Email: drmskarale13@gmail.com
Abstract Background: Many musculoskeletal disorders resemble each other and some may take weeks or months to evolve into a readily recognizable diagnostic entity. It is important to understand the prevalence of each potential diagnosis and to use an organized and evidence-based clinical approach. Here, in this study we have made an effort to explore specific diagnosis to the most common causes of mono-arthritis identified in rural patients of India (Maharashtra). Materials and Methods: This is anobservational and descriptive study conducted at SRTR Government Medical College, Ambajogai. Patients with acute or chronic mono-articular arthritis presenting for the first time in OPD or those who were admitted in medical units were selected. Total 50 patients above the age of 12 yrs were enrolled in the study. Post traumatic and soft tissue rheumatism mono-articular arthritis cases were excluded from the study. Results: Total 50 cases of new onset mono-articular arthritis were enrolled for study purpose. Mono-articular arthritis was common in males with male to female ratio of 1.5:1.Most commonly affected age group was 22-55 years with 56% of the patients in age group 22 to 55 years and mean age at the onset of symptoms was 35 years. Incidence of acute and chronic mono-articular arthritis was 48% and 52%% respectively with chronic being common than acute. Irrespective of the etiology of arthritis, knee joint was most commonly involved in mono-articular arthritis. Inflammatory arthritis was most common type of mono-articular arthritis comprising 44% cases along with 30% cases of infectious and 8% cases of non-inflammatory type of mono-articular arthritis. Conclusions: Idiopathic arthritis is common diagnosis in patients presenting for first time withmono-articular arthritis. Joint tuberculosis is most common cause of mono-articular arthritis followed by gout, seronegative spondyloarthropathy, rheumatoid arthritis, septic arthritis, osteoarthritis. Key Words: Mono articular arthritis, septic, tuberculous arthritis, gout, osteoarthritis.
INTRODUCTION Joint pain can have multiple causes, a reflection of the diverse joint diseases, which arise from inflammation, cartilage degeneration, crystal deposition, infection, and trauma. The initial aim of the evaluation of a patient with joint pain is to localize the source of the joint symptoms and to determine the type of pathophysiologic process responsible for their presence. The differential diagnoses of joint pain are generated in large part from the history and physical examination. Screening laboratory test results serve primarily to confirm clinical impressions and can be misleading if used indiscriminately.1 Individuals with musculoskeletal complaints should be evaluated with a thorough history, a comprehensive physical and musculoskeletal examination, and if appropriate, laboratory testing. The initial encounter should determine whether the musculoskeletal complaint signals a red flag condition (septic arthritis, gout, or fracture) or not. The evaluation should proceed to ascertain if the complaint is (1) articular or non-articular in origin, (2) inflammatory or non-inflammatory in nature, (3) acute or chronic in duration, and (4) localized (mono-articular) or widespread (poly-articular) in distribution. With such an approach and an understanding of the pathophysiologic processes, the musculoskeletal complaint or presentation can be characterized (e.g. acute inflammatory mono-arthritis or a chronic non-inflammatory, non-articular widespread pain) to narrow the diagnostic possibilities. A diagnosis can be made in the vast majority of individuals. However, some patients will not fit immediately into an established diagnostic category.2,3 Many musculoskeletal disorders resemble each other and some may take weeks or months to evolve into a readily recognizable diagnostic entity. It is important to understand the prevalence of each potential diagnosis and to use an organized and evidence-based clinical approach.Here, in this study we have made an effort to explore specific diagnosis to the most common causes of mono-arthritis identified in rural patients of India (Maharashtra). The objective of this study is to to assess the aetiology of mono-articular arthritis in patients presenting for the first time with mono-articular arthritis in the rheumatology clinic in a tertiary care hospital and to categorise patients as inflammatory, non-inflammatory and infective arthritis.
MATERIAL AND METHODS This is an observational and descriptive study conducted in department of medicine at SRTR Government Medical College, Ambajogai during March 2015 to March2016.Institutional ethics committee approval was taken for the study.Patients with acute or chronic mono-articular arthritis presenting for the first timeto medicine OPD and or those who were admitted in medical units were selected. Mono-articular involvement was defined by single joint involvement with two out of three features namely, swelling restricted to the joint, pain or tenderness of the joint and limitation of joint movement. Total 50 patients of above the age of 12 yrs were enrolled in the study. Traumatic arthritis and soft tissue rheumatism (tendinitis, bursitis, strain, sprain, osteomyelitis, soft tissue infections) patients and those who lost follow up were excluded from the study. Sample size was decided by random sampling method. Informed consent was taken from patient, parents or next of a kin. Individual patients were asked about detailed clinical history including personal habits, occupation and drug abuse. Detailed physical examination and examination of joints for pain, swelling, tenderness, local warmth and limitation of joint movement was carried out. We collected the demographic data, history, data on clinical examination and the relevant laboratory investigations, in addition to the data on radiological studies from patient’s outdoor and indoor records. All routine investigations and special investigations advised by treating physician were entered in the proforma. All patients were investigated and treated by physician who had experience in Rheumatology.ESR and CRP was measured for all patients at first and last visit. Procedures like aspiration of joint fluid and synovial biopsy were done by experienced physicians. Therapeutic interventions like synovectomy, joint replacement and arthrodesis were done by orthopedic surgeon with combined decision of Rheumatologists and Orthopedic surgeon. Etiology and clinicalfeatures were analyzed. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethics committee. Standard diagnostic criteria and guidelines were used for diagnosis and treatment of mono-articular arthritis. Investigations like AFB culture, crystals in the aspirate etc. were carried out only as per clinical suspicion. They were not applied universally across the study population. For tubercular arthritis where AFB smear or culture was negative, clinical features and other relevant investigations such as MRI of joint, lymphocyte predominant synovial fluid along with elevated ADA were used for supporting the diagnosis. Patients were categorized as inflammatory/infective/non-inflammatory on the basis of clinical features and laboratory evidence of inflammation, aetiology of arthritis and routine microscopic findings of joint fluid aspirate. Inflammatory disorders were identified by any of the four cardinal signs of inflammation (erythema, warmth, pain, or swelling), systemic symptoms (fatigue, fever, rash, weight loss), or laboratory evidence of inflammation namely, elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) and inflammatory type of morning stiffness (>30 min).Non inflammatory disorders were identified by pain without synovial swelling or warmth, absence of inflammatory or systemic features, daytime gel phenomena rather than morning stiffness and normal (for age) or negative laboratory investigations such as ESR and CRP.Infective etiology was identified by features of inflammatory etiology along with joint aspirate positive for Gram stain, culture, polymorphs >70% or WBC count >50,000/mm.4 All the information and data obtained was entered in Microsoft Excel and master chart was prepared. Statistical analysis was done by using Microsoft Excel 2013 and Graph Pad software.
RESULTS Total 50 cases of above age 12 years were enrolled in the study. Clinical features and etiology of mono-articular arthritis was studied. Total number of patients (n) = 50. Number of cases with Acute mono-articular arthritis =24/50 (48%). Number of cases with Chronic mono-articular arthritis =26/50 (52%). Mean age at presentation was 35 years with maximum (56%) patients in the range of 22-55 years with male to female ratio of 1.5:1. Total number male and female patient were 30 and 20 respectively.
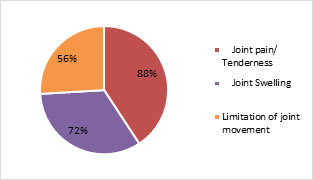
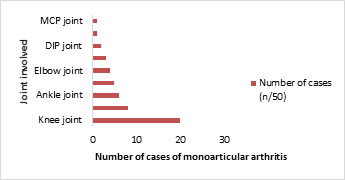
Figure 1: Clinical features of mono-articular arthritis Figure 2: Joint involvement at presentation in mono-articular arthritis
Table 1: Etiological classification of mono articular arthritis –Infectious, inflammatory, and Non-inflammatory arthritis
Joint pain was main presenting feature of mono-articular arthritis seen in 44 (88%) patients followed by limitation of joint movement in 28 (56%) patients and swelling or tenderness of joint in 36 (72%) patients. Irrespective of the etiology of arthritis, knee joint was most commonly involved in mono-articular arthritis. The knee joint mono-articular arthritis was present in 20 (40%) patients with other joints involved in decreasing frequency were, hip joint (n=8) 16%, ankle joint (n=6) 12%, shoulder joint (n=5) 10%, elbow joint (n=4) 8%, MTP joint (n=3) 6%, DIP joint (n=2) 4%, sternoclavicular joint (n=1) 2%, MCP joint (n=1) 2%. MCP-Metacarpo-phalangeal joint, DIP-Distal Interphalangeal Joint, MTP-Metatarso-phalangeal joint. On the basis of etiology, all cases were categorized into four main classes as idiopathic arthritis, infectious arthritis, inflammatory and non-inflammatory arthritis. In infectious arthritis, 10% (n=5) cases were of tuberculosis etiology and remaining 20% were due to staphylococcal aureus (n=4) and Burkholderia pseudomallei, Streptococcus viridans, S. pneumoniae and Pseudomonas aeruginosa. By etiopathogenesis, inflammatory arthritis was most common type of mono-articular arthritis comprising 44% cases. Considering etiology, idiopathic arthritiswas most common diagnosis (18%) in patients presenting for first time with mono-articular arthritis.
DISCUSSION Total 50 patients with acute or chronic onset symptoms of mono-articular arthritis were studied. Data was analyzed for etiology of mono-articular arthritis. Mean age at onset of arthritis symptoms was 35 years with maximum cases (28/50) 56% in the age group of 22 to 55 years. Male and female patients were 30 (60%) and 20 (40%) with male to female ratio of 1.5:1 which explains slight male preponderance in mono-articular arthritis. According to previous study by Windisch et al3, mean age at the onset of symptoms was 39 years, with 51% of patients presenting in the range between 20 and 40 years. Also Windisch et al3study showed male preponderance (56%) which is comparable to our study (60%). Based on etiology male preponderance is seen in septic arthritis, tubeculous arthritis, seronegative spodyloarthropathy, osteoarthritis and gout as studied before.3,4 In our study, we found 24 (48%) cases of acute mono-articular arthritis and 26 (52%) cases of chronic mono-articular arthritis which suggest chronic mono-articular arthritis more common than acute. Duration of symptoms at presentation varied from a minimum of 3 days to maximum up to 5 years with most in the range of 2 months to 1 year. As shown in Chart 1, joint pain or tenderness was main presenting feature of mono-articular arthritis seen in 44 (88%) patients followed by swelling or tenderness of joint in 34 (68%) patients and limitation of joint movement in 28 (56%) patients. History of morning stiffness lasting more than one hour was seen in 28 (56%) patients which were of inflammatory type of arthritis. Systemic features like fever, generalized body ache fatigue, anemia, lymphadenopathy, rash, serositis, weight loss and Reynaud’s phenomenon were present in (18) 36% cases. Fatigue, generalized body ache and fever was common in patient with inflammatory type of arthritis such as rheumatoid arthritis, seronegative arthropathies, juvenile idiopathic arthritis and crystal induced arthritis (gout). The knee joint mono-articular arthritis was present in 20 (40%) patients with other joints involved in decreasing frequency were, hip joint, ankle joint, shoulder joint, elbow joint, MTP joint, DIP joint, sternoclavicular joint, MCP joint (Chart 2). Previously joint involvement has been studied according to the etiology of arthritis and not as mono-articular arthritis which revealed that knee is the commonly affected joint in different etiologies. Irrespective of the etiology of arthritis, knee joint was most commonly involved in mono-articular arthritis. As per the available literature5,6 most commonly involved joint in septic arthritis is knee (50%), followed by hip (20%), shoulder (8%), ankle (7%) and wrist (7%). The elbow, interphalangeal, sternoclavicular, and sacroiliac joints each make up 1.4% of cases.5Siu Fai Li et al studied 92 cases of septic arthritis out of which 42 cases had knee joint arthritis followed by 11 to 6 cases for shoulder and hip joint respectively.7 Previous study on septic arthritis describes non-gonococcal septic arthritis is generally mono-articular (80 percent of cases) and most often affects the knees (50 percent of cases).8 A study report in osteoarticular, tuberculosis, 50% of the cases involves spine; hip and sacroiliac joint, 12% to 15%, knees, 10% ribs, 10% shoulder,7% ankle, 7% elbow, 2% and wrist 2%.9Hence this study supports the knee joint as commonly affected extra-axial joint in mono-articular arthritis. In a detailed report of bone and joint TB in Saudi Arabia, El Titi et al9 reviewed 68 cases in Riyadh that involved the spine in 57% of the cases; knee was affected in 14% followed by the hip in 10% of the cases.9 Harrison’s principles of internal medicine mentions that approximately 30% of patients with psoriatic arthritis have asymmetric oligo-arthritis commonly involving knee or another large joint with a few small joints in the fingers or toes and osteoarthritis is the most common cause of chronic knee pain in persons over age 45. With the supporting evidence of literature we conclude knee as most commonly affected joint in mono-articular arthritis. On the basis of etiology, all cases were categorized into four main classes (Table 1) as idiopathic arthritis, infectious arthritis, inflammatory and non-inflammatory arthritis. Inflammatory arthritis was further classified as crystal induced arthritis (gout), seronegative spondyloarthropathy, rheumatoid arthritis, juvenile idiopathic arthritis, osteoarthritis, and pigment induced arthritis and chronic hypertrophic synovitis. Infectious arthritis was most common etiology of mono-articular arthritis comprising (n=15) 30% cases. In infectious arthritis, 10% (n=5) cases were of tuberculosis etiology and remaining 20% were due to staphylococcal aureus (n=4) and Burkholderia pseudomallei, Streptococcus viridans, S. pneumoniae and Pseudomonas aeruginosa. By etiopathogenesis, inflammatory arthritis was most common type of mono-articular arthritis comprising 44% cases, 30% cases of infectious arthritis, 18% cases of idiopathic arthritis and 8% cases of non-inflammatory type of mono-articular arthritis. Considering single etiology, idiopathic arthritis was most common diagnosis (18%) in patients presenting for first time with monoarticular arthritis. Tuberculous arthritis patient were presented with chronic onset symptoms varying from 4 weeks to 2 years. All infectious arthritis cases required interventions like joint fluid aspiration or synovial biopsy. Two cases required synovial biopsy for diagnosis of tuberculous arthritis. Remaining 10 cases of infectious arthritis (Table 1) due to Staphylococcus aurous, Burkholderia pseudomallei, Streptococcus viridans, S. pneumoniae and Pseudomonas aeruginosa were positive on culture of the joint fluid. The available studies on mono-articular arthritis also described infections as most common cause of arthritis followed by crystal induced arthritis.11 According to literature, three main etiologies to be considered when a patient presents with acute mono-articular arthritis are trauma, infection and crystal-indeed arthritis such as gout or pseudo gout. S. aurous has been described as the most common organism that causes non-gonococcal arthritis.12 But in our study, mycobacterium tuberculosis was most common etiology for mono-articular infectious arthritis. With these findings, we can conclude that tuberculosis should not be missed as cause of infectious arthritis particularly in patients with long standing localized symptoms of mono-articular arthritis. Similar reports also found in a retrospective study done in Saudi Arabia. They report tuberculous arthritis as a forgotten cause of mono-articular arthritis due to understanding the disease and difficulty in diagnosis, which requires tissue sampling.13 Total 6 out of 50 cases were of crystal induced arthritis (Table 1)which were finally diagnosed as gout. Three cases presented with 1st metatarsophalangeal (MTP) joint involvement, one with two cases with distal interphalangeal (DIP) joint and one with ankle joint involvement. Four cases showed crystals in joint aspirate and remaining 2 were diagnosed on the basis of hyperuricemia, joint pain and risk factors. Pigmented villonodular synovitis can also present as mono-articular arthritis. Here we found one case of mono-articular arthritis due to pigmented villonodular synovitis. He presented with knee joint pain, swelling and tenderness with history of trauma to the knee five years before. MRI of the joint and histopathology of the synovium was consistent with the features of pigmented villonodular synovitis. According to the literature, 14 the incidence of pigmented villonodular synovitis is 1.8 cases per 1 million people per year, with no environmental, genetic, ethnic or occupational predilection.19 Pigmented villonodular synovitis generally occurs in patients between the ages of 20 and 45 years, but it has been found in patients as young as 11 years and as old as 70 years.14 The data described above may provide a reference for application to the Indian population. Additional studies with a larger study population are required to meet the need for population based information on etiology of mono-articular arthritis.
CONCLUSION Idiopathic arthritis is common diagnosis in patients presenting for first time withmono-articular arthritis. Joint tuberculosis is most common cause of mono-articular arthritis followed by crystal induced arthritis, seronegative spondyloarthropathy, rheumatoid arthritis, septic arthritis, osteoarthritis, juvenile idiopathic arthritis. Knee joint is most commonly affected in mono-articular arthritis with other commonly affected joints include hip joint, ankle joint, shoulder joint and elbow joint. By etiopathogenesis, inflammatory arthritis is most common type of mono-articular arthritis followed by infectious and non-inflammatory type arthritis.
ACKNOWLODGEMENTS Author contributions: All authors confirmed they have contributed to the intellectual content of this paper and have met the following 3 requirements: (a) significant contributions to the conception and design, acquisition of data, or analysis and interpretation of data; (b) drafting or revising the article for intellectual content; and (c) final approval of the published article. Authors’ disclosures of potential conflicts of interest: No authors declared any potential conflicts of interest. Role of sponsor: The funding organizations played no role in the design of study, choice of enrolled patients, review and interpretation of data, or preparation or approval of manuscript.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home