|
Table of Content - Volume 3 Issue 1 - July 2016
Electrocardiographic and echocardiographic characteristics of patients with dilated cardiomyopathy
Sadanand D Kamble1, Rajesh R Bobade2*
1,2Assistant Professor, Department of Medicine, Government Medical College, Latur, Maharashtra, INDIA. Email: drrajeshrb@gmail.com
Abstract Background: Dilated cardiomyopathy (DCM) is a syndrome characterized by cardiac enlargement and impaired systolic function of one or both ventricles. Due to increased awareness of this condition along with improvement in diagnostic techniques, dilated cardiomyopathy is being recognized as a significant cause of morbidity and mortality. The current study aimed at understanding the electrocardiographic and echocardiographic characteristics of DCM patients. Material and Methods: A total of 50 patients (30 males and 20 females) of dilated cardiomyopathy were studied.ECG and 2D Echocardiography was done among all these patients using standard techniques. Diagnosis of dilated cardiomyopathy done by echocardiography. Results: All ages were affected but elderly and middle aged population werefound to be predominantly affected. Left axis deviation, LVH, bundle branch block, atrial fibrillation were common ECG abnormalities. The ECHO findings in patients revealed a dilated LV cavity with low ejection fraction. Valvular regurgitation were seen in 86% of patients predominantly MR. Key Words: Dilated cardiomyopathy, electrocardiography, 2D Echo, Screening.
INTRODUCTION Cardiomyopathy is a primary disorder of the heart muscle that causes abnormal myocardial performance and is not result of disease or dysfunction of other cardiac structures, systemic arterial hypertension and valvular stenosis or regurgitation1. World Health Organization (WHO) and American Heart Association (AHA) classified cardiomyopathies into dilated, hypertrophic and restrictive type depending upon the basic disturbance of the function2,3. Dilated cardiomyopathy (DCM) is a syndrome characterized by cardiac enlargement and impaired systolic function of one or both ventricles. With increasing awareness of this condition along with improvement in diagnostic techniques dilated cardiomyopathy is being recognized as a significant cause of morbidity and mortality.DCM is considered to be an important cause of heart failure and accounts for up to 25% of all cases of congestive heart failure4. The Framingham study has reported 10% annual mortality rate for subjects having congestive cardiac failure5. Due to the increasing use of electrocardiogram (ECG) and 2D echocardiography, the incidence of dilated cardiomyopathy is also showing rising trend. It is a topic of interest of physician, cardiologist, cardiac surgeons and many other group of scientists. The present study was therefore undertaken to study the electrocardiographic and echocardiographic findings in patients with dilated cardiomyopathy.
MATERIAL AND METHODS The present study was performed in 50 patients of dilated cardiomyopathy either admitted in a teaching hospital or attending cardiology clinic. 30 patients were male and 20 were female. Patients were selected from those presenting with signs and symptoms of congestive cardiac failure, asymptomatic patients having unexplained cardiomegaly on chest X-ray and abnormal ECG changes. Diagnosis of dilated cardiomyopathy was done by echocardiography1. Patients were excluded from the study with signs and symptoms of congestive cardiac failure with cardiomegaly on chest X-ray due to other diseases like coronary artery disease (past history of myocardial infarction, significant Q wave in ECG, scars or akinetic segment on ECHO), rheumatic valvular heart disease (by history rechocardiography), congenital heart disease(by echocardiography) and pericardial disease (by echocardiography). After selection of patients, detail history was obtained from each patients. Each patient was specifically asked about dyspnea, palpitation, fatigability, sweating, swelling over feet, abdominal pain, syncope, and chest pain. Patient was asked regarding the major illness like Hypertension, Diabetes Mellitus, Myocardial Infarction, Renal disease, COPD. Family history suggestive of dilated cardiomyopathy was asked. Complete clinical examination was carried out. On physical examination, special attention was given to presence of raised JVP, edema, gallop rhythm, systolic murmur, respiratory rate and congestive hepatomegaly. Routine laboratory investigations such as BSL profile, Liver function tests, Renal function tests, Serum calcium and phosphorus, and serum cholesterol were done. Electrocardiography (ECG) Standard 12 lead electrocardiograms were recorded as 25 mm per second and 1 mV per cm standardization. Rate, rhythm, P-R interval, QRS interval, QTc interval were measured.QRS axis was determined in frontal plane. Axis directed to the region between 0 counter clockwise to 90 was taken as left axis deviation. P wave abnormalities were noted. Left atrial enlargement was defined as P terminal force in V1 equal to more negative than -0.04 mm sec or notched P wave with duration of 0.12 second or more. Right atrial enlargement was the presence of peaked P wave with a height of 2.5 mm or more in a lead II, III, and avF. Biatrial enlargement was defined as presence of large diphasic P wave in lead V1 with the initial positive component reading greater than 1.5 mm and the terminal negative component reading 1 mm in amplitude and 0.04 sec. in duration. Left ventricular hypertrophy was defined as per Sokolows criteria103,104 as R-wave in V5 or V6 + S-wave in V1 > 35 mm. ratio of R wave in V6 and maximum R wave in leads I, II, III (RV6/R max.) was calculated to find out the correlation the correlation of this ratio with ventricular dilatation and ejection fraction103. ST segment and T wave abnormalities were noted. Echocardiography Comprehensive M-mode, two dimensional and Doppler echocardiographic examinations were performed in all patients. Various measurements were done using long axis, short axis, two chamber and four chamber views. Measurements of left ventricular inner diameter in diastole (LVIDd), Left ventricular inner diameter in systole (LVIDs), Ejection fraction (EF), Right ventricle, Left atrium(LA), Intraventricular septum (IVS) and of Left Ventricular Posterior wall thickness (LVPW) were taken and compared with standard normal values in adults. Patients having left ventricular dilatation and ejection fraction less than 40 per cent were diagnosed as dilated cardiomyopathy and included in the study. Patients looked for scar and akinetic segments and such patients were excluded from study. Valvular regurgitations were semi-quantitatively assessed with colour flow Doppler echocardiography. Other features like diastolic dysfunction, pulmonary hypertension, pericardial effusion and intra-cavitatory clots were looked for.
RESULTS In present study dilated cardiomyopathy was more common in the middle age, most common in fifth decade. Males were affected more common than female (M: F ratio - 3:2) (Table 1).
Table 1: Age and Sex distribution
In the present study, range of QRS axis was from -500 to + 900. Left axis deviation was seen in 22 (44%) patients. Mean ventricular rate in the present study was 107.0±10.51 per min.PR interval ranged from 0.16 to 0.26 seconds with mean of 0.176±0.0303 seconds. 5 patients (10%) had first degree AV block. No patients had second or third degree AV block. P waves were absent in 5 patients with atrial fibrillation, 14 (28%) patients had abnormal P waves. Mean left ventricular QRS voltage (S in V1 + R in V5 or V6) was 32.38 ± 11.08 mm. 22 patients had evidence of LVH on ECG (Table 2 and 3).
Table 2: ECG Features in dilated cardiomyopathy patients (n=50)
Table 3: ECG Abnormalities in Dilated Cardiomyopathy
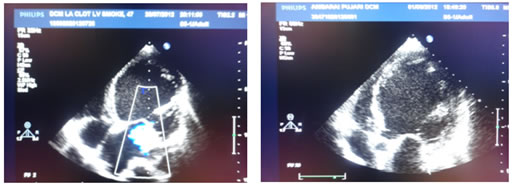
In present study, left ventricular dimensions were less but all patients had global hypokinesia and poor ejection fraction. LVPW and IVS thickness was within normal limits. Right ventricular dilatation was seen in 20 (40%) of patients and mean right ventricular diameter was 22.84 ± 7.20 mm. Left atrial enlargement was seen in 27 (54%) patients and mean LA diameter was 40.94 ± 6.30 mm. Valvular regurgitation was seen in 43 (86%) of patients. There was isolated MR in 12 (24%) of patients, while MR was associated with TR in 26 (52%) patients and with TR and AR in 4 (8%) patients. There was isolated TR in 1 (2%) patient. Diastolic dysfunction was present in 21 (42%) patients in the present study. Pericardial effusion was present in 15 (30%) patients. In 5 (10%) patients, clots were detected (Table 4 and 5) (Fig. 1 and 2).
Table 4: Echocardiographic Features of DCM
Table 5: 2D ECHO features of DCM
Fig 1 and 2: Echocardiographic features of dilated cardiomyopathy
DISCUSSION In the present study dilated cardiomyopathy was more common in middle age and elderly but commonest age group affected was 31-70 years. Males were affected more than females. Studies by Roberts et al6, Pelliccia et al7 and Parale et al8 reported 45, 48±11 and 51.6 years commonest age group respectively. Mean ventricular rate in the present study was 107.0±10.51 per min. Most of the patients had sinus tachycardia as they were in congestive heart failure. Tachycardia in patients with dilated cardiomyopathy is also reported by studies done by Werner et al9, Wilensky et al10. In the present study, range of QRS axis was from -500 to +900. Left axis deviation was seen in 22 (44%) patients. Roberts et al6 have reported left axis deviation in 43% and right axis deviation in 7% of patients. Wilensky et al10 have found that range of QRS axis was from -1300 to +1300 and mean QRS axis was -210.Parale et al8 have found left axis deviation in 59% of patients. Techuan Chou11 mentioned left axis deviation in 42% of patients of dilated cardiomyopathy. Findings in the present study were comparable with other studies. In the present study, PR interval ranged from 0.16 to 0.26 seconds with mean of 0.176±0.0303 seconds. 5 patients (10%) had first degree AV block. No patients had second or third degree AV block. In a study by Wilensky et al10, mean PR interval was 0.20 sec. (Range 0.14 – 0.29). Barbosa et al12 found first and second degree AV block in 11% and Scholler et al13 found first degree AV block in 17.6% and second degree AV block in 10.6%.AV blocks are poor prognostic markers in dilated cardiomyopathy and the progress over time with increasing fibrosis and myocyte hypertrophy. In the present study. AV block were seen in 10% of cases comparable to other studies. In the present study, P waves were absent in 5 patients with atrial fibrillation, 14 (28%) patients had abnormal P waves. Techuan Chou11, in a series of 40 patients, noted P wave abnormalities in 15 patients. Left atrial enlargement was the most common feature. Roberts et al6 and Barbosa et al12 also found left atrial enlargement more commonly than right atrial or biatrial enlargement. In the present study mean left ventricular QRS voltage (S in V1 + R in V5 or V6) was 32.38 ± 11.08 mm. 22 patients had evidence of LVH on ECG. Results in the present study were comparable with other studies6,14. Techuan Chou11 mentioned that relative incidence of LBBB in idiopathic dilated cardiomyopathy is higher than in IHD. In patients with cardiomegaly of unknown cause, the presence of LBBB further supports the diagnosis of primary myocardial disease. Abnormal left axis deviation consistent with LAHB was also common, occurring in as many as 42% in some series15. Many of the studies had used 24 hours ambulatory ECG monitoring for the detection of arrhythmia, incidence in studies by Scholler et al13, Anderson et al (19%)16 and Parale et al (12%)8 was much higher than present study. 2D Echocardiographic observations during the study period revealed dilated poorly contracting ventricles as features of dilated cardiomyopathy. Left ventricular dimensions were less (mean LVIDd=60.78±6.56 mm; LVIDs=50.38±7.86 mm) but all patients had global hypokinesia and poor ejection fraction (mean ejection fraction=28 ± 7.0%) which was comparable to studies by Karl et al17 and Fazio et al18. Abbassi et al19 found that left ventricular posterior wall motion was markedly reduced in congestive cardiomyopathy. According to Harvey Feigenbaum20, both septal and posterior ventricular walls moves poorly, however, wall thickness in within normal limits. In the present study, LVPW and IVS thickness was within normal limits. In the present study, right ventricular dilatation was seen in 20 (40%) of patients and mean right ventricular diameter was 22.84±7.20 mm. According to Dec et al21, idiopathic dilated cardiomyopathy is diffuse process and concomitant right ventricular dysfunction is seen in 85-90% of patients. Werner et al9 found that mean right ventricular diameter was 27±6 mm in surviving patients and 29±4 mm in patients who died at the end of study. Right ventricular dilatation was a predictor of mortality. In the present study, left atrial enlargement was seen in 27 (54%) patients and mean LA diameter was 40.94 ± 6.30 mm. In a study done by Karl et al17, mean left atrial diameter was 47 ± 7 mm. In the present study, valvular regurgitation was seen in 43 (86%) of patients. There was isolated MR in 12 (24%) of patients, while MR was associated with TR in 26 (52%) patients and with TR and AR in 4 (8%) patients. There was isolated TR in 1 (2%) patient. Werner et al9 found the presence of MR in most of the patients with dilated cardiomyopathy. Karl et al17 found that MR was present in 89% of the patients. This finding was a marker of poor outcome in patients with either ischemic or idiopathic dilated cardiomyopathy. In heart failure, the functional MR is frequently attributed to one of 3 factors – LV enlargement, dilatation of mitral valve annulus or dysfunction of the papillary muscles. Diastolic dysfunction was present in 21 (42%) patients in the present study. Bahl et al22 in their study of LV diastolic dysfunction in patients of idiopathic dilated cardiomyopathy that patients with advanced disease demonstrate a restrictive pattern on pulse Doppler echocardiography. Similar findings were reported by Karl et al17. Diastolic dysfunction is very complex and is influenced by several factors such as age, systolic function, heart rate atrioventricular pressure gradient, preload and mitral regurgitation Anderson et al16 have shown the presence of diastolic dysfunction even in patients without LV dilatation. In the present study, pericardial effusion was present in 15 (30%) patients. In the present study, in 5 (10%) patients clots were detected. In a study done by Robert et al6 on necropsy of patients of dilated cardiomyopathy, intracavitory thrombi were present in 53% cases. Blood stasis and low shear rate in that hypocontractileventricle lead to the activation of coagulation process. Intracavitatory thrombi are most commonly seen at the left ventricular apex21. The study concluded that regular echochardiographic screening of patients with dilated cardiomyopathy is very important to identify and prevent complications among them.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home