|
Table of Content - Volume 3 Issue 2 - August 2016
Utility of spirometry in early case-identification and diagnosis of suspected cases of obstructive lung diseases
Gaurav R Dubey1, Anjali S Deshmukh2*, Vijay R Kapse3
1Assistant Professor, Department of Tb and Respiratory Medicine, Dr PDMMC Amravati, Maharashtra, INDIA. 2Assistant Professor, 3Associate Professor, Department of Medicine, Dr.S.C.G.M.C.Nanded, Maharashtra, INDIA. Email: dr.dranju@rediffmail.com
Abstract Background: Spirometry is an essential investigation to confirm the clinical diagnosis of obstructive lung diseses as well as a useful investigation in assessing severity. Spirometry is also an important investigation in confirming the clinical diagnosis of asthma and evaluating asthma severity and pattern of airflow limitation. Aims and objective: To study the utility of Spirometry in early case-identification and diagnosis of obstructive pulmonary diseases. Materials and Method: All the patients of obstructive lung diseases attending the respiratory OPD during the January 2016 to June 2016 were enrolled in the present study. The patients not willing to participate the study were excluded. The detail demographic characteristics such as age, sex, occupation etc were inquired and were entered a prestructured proforma. The associated risk factors were also investigated and were recorded. The presenting symptoms were also recorded. Spirometry was performed with Morgan transfer test with Wyvern software integrated pulmonary function program. The collected data was entered in Microsoft excel and was analyzed and presented with appropriate tables and graphs. Results: Majority of the patients were male (59.32%). The mean age of the study patients was 46.26±16.71 years. 28.81% patients were having smoking habit. Majority of them were using bidi and 5 were female. Majority of the patients (45.7%) in the present study were having Obstruction with good BDR pattern on Spirometry followed by mixed pattern (15.2%) and obstruction with poor BDR (12.4%). Normal Spirometry pattern was observed in 11.2% patients, small airway pattern was seen in 10.7% and 4.51% patients were having restrictive pattern. The Severity of Obstruction (GOLD) was also assessed and it was seen that majority of the patients (59.09%) with poor BDR were having moderate obstruction whereas majority of the patients (59.26%) with good BDR were having sever obstruction. Conclusion: Thus we conclude that spirometry is helpful in differentiating various obstructive lung diseases. It also provides and objective record of the degree of obstruction to aid in prognosis and therapy. Also it quantifies the stage of the disease. Thus it can be concluded that Spirometry is a very useful but neglected tool in the diagnosis of various obstructive lung diseases. Key Words: Obstructive pulmonary diseases, spirometry, diagnosis.
INTRODUCTION Chronic Obstructive Lung Disease (COPD) is a preventable and treatable disease that characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and associated with an abnormal inflammatory response of the lung to cigarette smoke and other noxious particles or gases1. Prevalence of clinically significant COPD (GOLD stage II or higher) is estimated to be 10.1% according to the results of an international population-based investigation2. It was estimated that 1 every 4 men and 1 every 6 women without COPD at the age of 55 years will eventually develop COPD at some time during their further life3. According to the Global Burden of Disease (GBD) study 2006, a systematic review and meta analysis was conducted based on the published medical literature and it was found that the global prevalence of chronic obstructive pulmonary disease in adults aged ≥40 years was 9-10%.4 The prevalence of COPD is explored in many community-based projects; and is found to be 16.4% for Spanish,5 2.8% for population from England and Wales,6 and 13.8% for population of Karachi.7 Spirometry is an essential investigation to confirm the clinical diagnosis of COPD as well as a useful investigation in assessing severity.1,8,9 Spirometry is also an important investigation in confirming the clinical diagnosis of asthma and evaluating asthma severity and pattern of airflow limitation.10,11 Barriers to performing spirometry in community settings include lack of access to calibrated spirometers, inadequate training in performing spirometry, lack of quality-control systems to ensure accurate results, and inadequate interpretation skills among health professionals performing the test.12,13
MATERIALS AND METHOD The present study was conducted in the department of respiratory medicine after the approval by the institute ethics committee. All the patients of suspected obstructive lung diseases attending the respiratory OPD during the January 2016 to June 2016 were enrolled in the present study. The patients not willing to participate the study were excluded. The detail demographic characteristics such as age, sex, occupation etc were inquired and were entered a prestructured proforma. The associated risk factors were also investigated and were recorded. The presenting symptoms were also recorded. Spirometry was performed with Morgan transfer test with Wyvern software integrated pulmonary function program. Asthma was diagnosed on the basis of Global Initiative for Asthma guidelines i.e. history of paroxysmal dyspnoea and spirometry showing forced expiratory volume in one second (FEV1 ) and forced vital capacity (FVC) ratio less than 70% and FEV1 less than 80% predicted with good bronchodilator reversibility i.e. an improvement in FEV1 by 12% and 200 ml. Diagnosis of COPD was based on Global initiative for Obstructive Lung Disease guidelines i.e. cough, sputum production, or dyspnoea with history of exposure to risk factors (e.g. tobacco smoking ≥ 20 pack-years) and spirometry showing FEV1 / FVC less than 70% and FEV1 less than 80% predicted with poor bronchodilator reversibility. Smoking history of one pack year was taken as smoking 20 cigarettes or bidis per day for one year. The collected data was entered in Microsoft excel and was analyzed and presented with appropriate tables and graphs. RESULTS
Table 1: Age, sex and occupation distribution of study patients
In the present study total 177 patients of chronic obstructive pulmonary disease were studied. It was seen that the patients were in the range of 14 – 81 years and majority of the patients were in the age group of 31-40 years of age followed by 51-60 years and 61-70 years. The mean age of the study patients was 46.26±16.71 years. It was seen that majority of the patients were male (59.32%) with male: female ratio of 1.46:1.
Table 2: Distribution of study patients according associated to risk factors
It was seen that 51 (28.81%) patients were having smoking habit. Majority of them were using bidi. And 5 were female. It was seen that out of total 72 female in the present study 33 were exposed to chullah smoke. Past history of tuberculosis was reported by 18.08% patients. Family history of atopy was reported by 13.56% patients.
Table 3: Distribution of study patients according Spirometric pattern
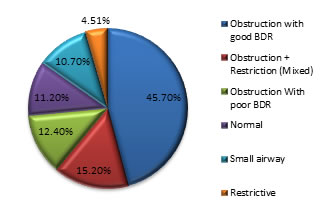
It was seen that majority of the patients (45.7%) in the present study were having Obstruction with good BDR pattern on Spirometry followed by mixed pattern (15.2%) and Obstruction With poor BDR (12.4%). Normal Spirometry pattern was observed in 11.2% patients, small airway pattern was seen in 10.7% and 4.51% patients were having restrictive pattern.
Figure 1: Distribution of patients according Spirometric pattern
Table 4: Distribution of study patients according severity of Obstruction (GOLD) in BDR
The Severity of Obstruction was also assessed and it was seen that majority of the patients (59.09%) with poor BDR were having moderate obstruction whereas majority of the patients (59.26%) with good BDR were having sever obstruction.
DISCUSSION The present study was conducted in the department of respiratory medicine of ABC medical college with the aim to utility of Spirometry in early case-identification and diagnosis of chronic obstructive pulmonary diseases. For this purpose total 177 patients of COPD were enrolled in the study and the results of Spirometry were studied in them. Asthma was diagnosed on the basis of Global Initiative for Asthma guidelines i.e. history of paroxysmal dyspnoea and Spirometry showing forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) ratio less than 70% and FEV1 less than 80% predicted with good bronchodilator reversibility i.e. as improvement FEV1 by 12% and 200 ml. Diagnosis of COPD was based on global initiative for obstructive lung Disease guidelines i.e. cough, sputum production, or dyspnea with history of exposure for risk factors (e.g. tobacco smoking) and Spirometry showing FEV1 / FVC less than 70% and FEV1 less than 80% predicted with poor bronchodilator reversibility. It was seen that the patients were in the range of 14 – 81 years with the mean age of the study patients was 46.26±16.71 years. Majority of the patients were in the age group of 31-40 years of age followed by 51-60 years and 61-70 years. COPD prevalence is higher in subjects older than 40 years of age compared with those younger than 40 years, regardless of the diagnostic criteria used14. It was seen that majority of the patients were male (59.32%) with male: female ratio of 1.46:1. The role of sex in determining COPD risk remains unclear14. In the past, most studies showed that COPD prevalence and mortality were greater among men than women. More recent studies showed that the sex difference in COPD prevalence tends to disappear15,16. Regarding COPD incidence, most17-19 but not all20 studies found a higher risk in men than in women. Out of total 177 subjects, most common Spirometric pattern was Asthma. This is similar to study done by D.V. Gothi et al21. Also slight female predominance found is similar to study done by P. Vaidya et al22. It was seen that majority of the patients (45.7%) in the present study were having Obstruction with good BDR pattern on Spirometry followed by mixed pattern (15.2%) and Obstruction With poor BDR (12.4%). Normal Spirometry pattern was observed in 11.2% patients, small airway pattern was seen in 10.7% and 4.51% patients were having restrictive pattern. Majority of cases (86.36%) presenting with Spirometry suggestive of obstructive airway disease with poor BDR (COPD) were in stage II and III. It was seen that majority of the patients (59.09%) with poor BDR were having moderate obstruction whereas majority of the patients (59.26%) with good BDR were having sever obstruction. Similar findings have been found in study done by D.V. Gothi et al21. Most common etiological factor identified in patients with final diagnosis of COPD was smoking (70.58% males and 20% females), post T.B. and history of exposure to chullah smoke constitute second and third largest group. Smoking is a well known etiological factor for COPD. In study done by D.V. Gothi et al21 98% of patients were smokers. In non smokers, especially women exposure to indoor pollution from domestic combustion of solid fuel is an important factor as reported by Surinder K Jindal23. Age range of patients with COPD was 28-75 years. It was similar to study done by Bhattacharya et al (1975). Mean age of patients was 53 years. Mean age was nearly equal to study done by D.V. Gothi et al21 where mean age 54 years male to female ratio was 3.4: 1. In study by Surinder K Jindal23 male to female ratio was 1.56: 1. More number of males in our study may be due to rural population in our study where very less females smoke compared to males. Age range for patients with final diagnosis of bronchial asthma was similar to study done by D.V. Gothi et al21. Majority (57%) of cases had moderate or severe obstruction in study by D.V. Gothi et al21. In our study more than 90% had moderate or severe obstruction. This difference may be due to more no. of cases from rural population in our study with late presentation. CONCLUSION Thus we conclude that spirometry is helpful in differentiating various obstructive lung diseases. It also provides and objective record of the degree of obstruction to aid in prognosis and therapy. Also it quantifies the stage of the disease. Thus it can be concluded that Spirometry is a very useful but neglected tool in the diagnosis of various obstructive lung diseases.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home