|
Table of Content - Volume 3 Issue 3- September 2016
Study of correlation between ECG findings and echocardiographically detected left ventricular diastolic dysfunction
Vijay S Nagaonkar
Assistant Professor, Department of Medicine, D Y Patil Medical College, Vidyanagar, Kasaba Bawda, Kolhapur, Maharashtra-416006, INDIA. Email: drvijaynagaonkar@gmail.com
Abstract Background: Electrocardiographic evidence of left ventricular hypertrophy is one of the most widely used markers of cardiovascular morbidity. Inspite of their high specificity, the ECG indices are still less sensitive. Echocardiography has many advantages over electrocardiogram but it is expensive and not widely available in the rural regions of India. So, the study aimed to explore the correlation between ECG findings and echocardiographically detected left ventricular diastolic dysfunction. Material and Methods: Fifty clinically diagnosed patients of LVH were included in this study. The ECGs of patients enrolled in the study were scrutinized for evidence of left ventricular hypertrophy (LVH) by the Romhilt Estes Point Score system as well as Sokolow-Lyon Index. This was followed by echocardiography and left ventricular mass and left ventricular mass index was calculated. Results: The average age of a patient with left ventricular diastolic dysfunction was 59.66 years. Two patients had ECGs with evidence of LVH by the Romhit-Estes Point Score System and Sokolow-Lyon Index. Both patients with left ventricular hypertrophy on ECG had left ventricular diastolic dysfunction on echocardiography. Conclusion: ECG showed a low correlation with the echocardiogram however, sensitivity of ECG to detect LVH can be increased by Sokolw Lyons voltage criteria and Romhilt-Estes point score system. Key Words: Electrocardiogram, echocardiography, left ventricular hypertrophy, Sokolw Lyons voltage criteria, Romhilt-Estes point score system.
INTRODUCTION Diastolic dysfunction refers to a condition in which abnormalitiesin mechanical function are present during diastole. Abnormalitiesin diastolic function can occur in the presence or absence of a clinical syndrome of heart failure and with normal or abnormalsystolic function1. Left ventricular hypertrophy confers an increased mortality independent of other cardiovascular risk factors. Recent studies have focused attention on the association of left ventricular hypertrophy with left ventricular diastolic dysfunction as the earliest evidence of impaired left ventricular function in hypertension. Clinically, reduced ventricular compliance may be detected by the presence of an atrial (S4) gallop rhythm or left atrial enlargement on electrocardiogram. However, the non invasive techniques such as myocardial scintigraphy and echocardiography are more sensitive2. Echocardiographic methods of assessing diastolic function include the determination of left ventricular dimensions by M mode and 2D echo, and isovolumic relaxation time, transmitral valve blood flow velocities by Doppler, Pulmonary vein flow and Doppler tissue imaging. Electrocardiographic evidence of left ventricular hypertrophy is one of the most widely used markers of cardiovascular morbidity3.Inspite of their high specificity, the ECG indices are still less sensitive. It is very important to detect left ventricular hypertrophy by effective, low-cost screening, applicable to the population in general4,5. In addition to the initial assessment, echocardiography can be performed serially to monitor the course of the disease. Doppler evaluation of parameters of left ventricular filling and relaxation have shown good reproducibility when standard procedures for imaging and reading are followed6. Though echocardiographyhas many advantages over electrocardiogram, it is expensive and not widely available in the rural regions of India. So, the study aimed to explore the correlation between ECG findings and echocardiographically detected left ventricular diastolic dysfunction.
MATERIAL AND METHODS This cross sectional study was done over a period of two years from September 2006 to September 2008 in a Department of Medicine. Inclusion Criteria All hypertensive patients newly or previously detected with BP more than 140/90 (JNC VII Stage I and II) at two or more recordings after an initial screening. The BP were measured with the mercury sphygmomanometer in the consulting room in sitting position after about 5–10 minutes of rest according to standard guidelines. Exclusion Criteria Patients of HTN with renal failure, valvular heart disease, severe anemia, co-existent IHD, gross CCF, Diabetes Mellitus, atrial fibrillation, patients of hypertrophic obstructive cardiomyopathy and on treatment with antihypertensive drugs. Patients with renal failure are excluded by doing renal function tests and urine biochemistry and microscopy. Screening for valvular heart disease is done by history, Physical examination, Chest X-Ray, Electrocardiogram and Echocardiography itself. Severe anemia was excluded by complete blood count, clinical features. IHD was excluded by history, physical examination, normal ECG and absence of regional wall motion abnormalities.CCF was excluded clinically by history, S3, S4 gallop rhythm, tachycardia, raised JVP, dependent edema, congestive hepatomegaly and basal crepts. Atrial fibrillation was ruled out by clinical features and ECG findings. Echocardiography Patients satisfying all the inclusion criteria were subjected to echocardiography. Echocardiography was done by a doctor trained and accredited by Indian Academy of Echocardiography on GE (Logiq 3) expert model no. AY-15 CUI.M-mode echocardiography was used to measure Left ventricular interior diameter at end systole –LVIDes, Left ventricular interior diameter at end diastole- LVIDed, Interventricular Septal Dimension end systole –IVSes, Interventricular Septal Dimension end diastole- IVSed, Left ventricular Posterior wall dimension end systole LVPWDes, Left ventricular Posterior wall dimension end diastole LVPWDed, End diastolic volume – EDV and End systolic volume-ESV. Left ventricular mass was calculated according to CUBED formula (i.e. TECHHOLZ formula) as, Left ventricular Mass = (IVS + LVIDed+ LVPWD)3 - (LVID)3× 1.05gm/cm3 (Where 1.05gm/cm3 is specific gravity of muscle). Left ventricular hypertrophy was reported if Left ventricular mass was >150gm/cm3 for men and>120gm/cm3 for women. The ejection fraction (EF) in percentage was calculated using the formula – E.F.= (LVIDd3 – LVIDs3) / LVIDd3 and E.F. (%)= EDV- ESV / EDV ×100 Evaluation of diastolic dysfunction was carried out by E/A ratio, Deceleration time and LA size. Ventricular diastolic function was measured by pulsed wave and continuous wave Doppler echocardiography. The mitral inflow velocities at the leaflet tips was used to assess LV diastolic dysfunction as this is the point at which mitral flow velocities are equal. Electrocardiography A standard 12 lead ECG was obtained for all patients enrolled in this study. The ECGs of patients enrolled in the study were scrutinized for evidence of left ventricular hypertrophy (LVH) by the Romhilt Estes Point Score system7 as well as Sokolow-Lyon Index8. Patients whose ECG scored 5 or more out of 12 on the Romhilt Estes Point Score System (81) were labeled as having electrocardiographic (ECG) criteria for left ventricular hypertrophy. Patients with SV1 +(RV5/RV6)>3.5mV or RaVL>1.1mV were labeled as having electrocardiographic criteria for left ventricular hypertrophy according to Sokolow-Lyon Index.
RESULTS During the Specified study period, 200 hypertensive patients were considered for participation in the study and assessment of left ventricular diastolic dysfunction. Of the 200 patients, screened for the study, 50 patients had ischemic heart disease and 50 patients had diabetes mellitus and 50 patients had deranged renal function tests. These patients were studied clinically but excluded because they didn’t satisfy the biochemical and other inclusion criteria. The remaining 50 patients who satisfied all the inclusion criteria were enrolled and studied. The age of the participants in the study ranged from 35 years to 70 years with a range of 35 years. The average age of a study subject was 53.48 years. The age of patients with left ventricular diastolic dysfunction ranged from 45 years to 70 years with a range of 25 years. The average age of a patient with left ventricular diastolic dysfunction was 59.66 years. The age of patients without left ventricular diastolic dysfunction ranged from 35 years to 72 years with a range of 37 years. The average age of a patient with hypertension and without left ventricular diastolic dysfunction was 47.69 years.
Table 1: Age distribution of patients of hypertension with left ventricular diastolic dysfunction (LVDD)
Thus, the prevalence of left ventricular diastolic dysfunction in different age groups is 16.66%, 41.77%, 77.77% and 91.66% respectively. The difference between 35-45 age group and 66-75 age group was analyzed by applying Z test of proportion with a p value of <0.01 showing that the difference is highly significant statistically. Of the 50 patients studied, 25 were female and 25 were male. Of the 27 patients with left ventricular diastolic dysfunction 14 were female and 13 were male. In the present study, 2 patients had ECGs with evidence of LVH by the Romhit Estes Point Score System and Sokolow-Lyon Index. Both patients with left ventricular hypertrophy on ECG had left ventricular diastolic dysfunction on echocardiography. Table 2: Correlation between ECG findings and echocardiographically detected left ventricular diastolic dysfunction (LVDD)
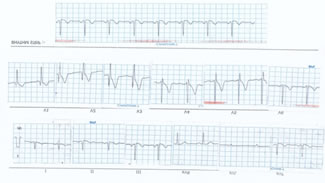
Figure 1: Electrocardiogram of 62-years old male known hypertensive for 7 years showing left ventricular hypertrophy according to Sokolow-Lyon Index.
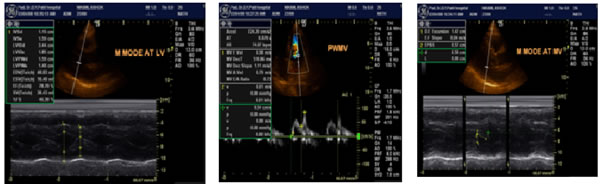
Figure 2: Echocardiography and color doppler of 60-yrs old male known hypertensive since 6 years showing LVdiastolic dysfynction with E/A ratio 0.73
DISCUSSION It was seen that with advancing age, the prevalence of left, ventricular diastolic dysfunction increases. This is explained by the increased duration of arterial hypertension with advancing age and also the independent effects of aging on left ventricular relaxation characterized by decreased peak velocity of early diastolic mitral inflow, increased peak velocity of late diastolic inflow, increased isovolumic relaxation time and increased early diastolic deceleration time as elucidated by Burlew BS9 in their assessment of left ventricular diastolic function in the elderly. This is due tomaladaptive remodeling of the interstitium associated with aging, resulting in an increase in interstitial collagen content. The interstitium normally plays a critical role in the generation of early diastolic suction. When there is a significant enough increase in myocardial collagen volume fraction, with its increased viscoelastic burden, this normal early diastolic suction is compromised and diastolic pressures increase. Shi-Yan li et al10 also detailed the effects of aging on left ventricular diastolic dysfunction and pointed out that the increased incidence of impaired relaxation and increased passive stiffness was due to increased interstitial collagen content and decreased number of functioning myocytes that occur as part of the normal ageing process. In the present study, a standard 12 lead ECG was obtained for all patients and scrutinized for evidence of left ventricular hypertrophy by the Romhilt Estes Point Score System; with a score of 5 or greater out of 12 being considered positive ECG evidence of left ventricular hypertrophy as well as Sokolo Lyon Index. A total of 2 patients out of 50 had ECG criteria for left ventricular hypertrophy. Thus, prevalence of identifying LVH on ECG is only 4%.Borhani NO11 reported that left ventricular hypertrophy (LVH) is a major complication of hypertension. It is a major risk factor for mortality, including sudden death. Although LVH is not always directly related to the level of blood pressure (BP), it occurs early in the course of hypertension. In the early stages of hypertension, LVH is associated with reduced cardiac function, even in the presence of a well-maintained ejection fraction and cardiac output. Thus, it is important to detect LVH early in the course of hypertension and halt its progression. Prevalence of LVH in the hypertensive population varies, mostly because of the different methods used for its diagnosis. Prevalence of increased left ventricular mass, determined by echocardiography, ranges from 26% to 48% in patients with hypertension. On the other hand, prevalence of tall R wave, ST segment deviation, and T-wave inversion, determined by ECG, is considerably lower than that. In the Hypertension Detection and Follow-Up Program (HDFP), in which all hypertensive participants had a 12-lead ECG at baseline, the prevalence of ECG-determined LVH was between 5% and 11%, depending on criteria used (e.g., tall R wave alone or ST segment deviation). Rigorous treatment of hypertension halts the progression of LVH and may cause regression as well. To be effective, treatment must begin early in the course of hypertension, especially mild hypertension (i.e., diastolic BP (DBP) 90-104 mmHg). It is in the early stages of hypertension that effective treatment will most likely exert its beneficial effect in the prevention of LVH. Woythaler JN et al12 compared the accuracy of electrocardiography, M-mode echocardiography and two-dimensional echocardiography in predicting left ventricular hypertrophy in 50 patients who came to autopsy within 6 months after the studies were performed. Several methods for determining left ventricular hypertrophy were examined for each of the three techniques. M-mode echocardiography was technically adequate to evaluate the presence or absence of left ventricular hypertrophy more often than either electrocardiography or two-dimensional echocardiography. Measurements from M-mode echocardiography also correlated best with autopsy measurements. Both echocardiographic techniques had a higher sensitivity than electrocardiographic criteria in diagnosing left ventricular hypertrophy. Two-dimensional echocardiography was not shown to improve the M-mode assessment of left ventricular hypertrophy. In an attempt to simplify both M-mode left ventricular mass calculations and the diagnosis of left ventricular hypertrophy for the clinician, a left ventricular mass nomogram was constructed, enabling quick insertion of standard M-mode echocardiographic measurements. All patients with ECG evidence of left ventricular hypertrophy had evidence of left ventricular diastolic dysfunction on echocardiography. Thus, hypertensive patients with ECG evidence of left ventricular hypertrophy constitute another group that would benefit from energetic screening for the evidence of left ventricular diastolic dysfunction on echocardiography. In conclusion, since LVH is a known independent risk factor of mortality, improved ECG detection may lead to more widely applied treatment; however, it has been found that despite various ECG criteria having greater sensitivities, their prognostic value in predicting cardiovascular morbidity and mortality varies considerably.ECG showed a low correlation with the echocardiogram however, sensitivity of ECG to detect LVH can be increased by Sokolw Lyons voltage criteria and Romhilt-Estes point score system.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home