|
Table of Content - Volume 3 Issue 3- September 2016
Clinico-epidemiological study of Vitiligo
Garima Khurana1, Shilpa Pathrikar2*, Ashish Deshmukh3
Department of Dermatology, MGM’s Medical College and Hospital, Aurangabad, Maharashtra, INDIA, Email: garimak1016@gmail.com
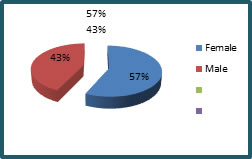
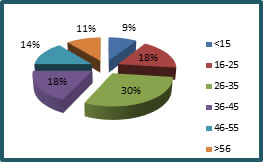
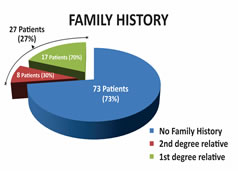
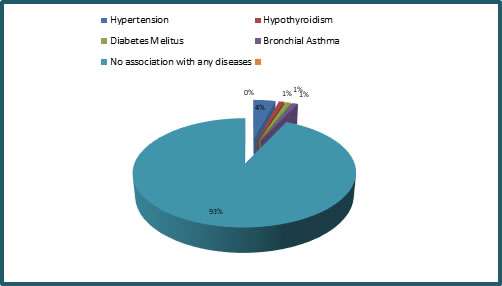
Abstract Background: Vitiligo is a commonly acquired, idiopathic, heritable depigmentary anomaly of the skin and/or mucous membranes. It is a major social and cosmetic concern, characterized by depigmented patches surrounded by a normal or a hyperpigmented border. Aims: To study the demographic, etiological and clinical profile of vitiligo patients. Methods: This cross-sectional hospital-based clinical study was conducted in a tertiary medical center over a period of one year which involved 100 patients with vitiligo who were assessed using detailed history taking and clinical examination for demographic, etiological and clinical data. Results: Majority of patients were in the age group of 26-35 years. Among 100 patients, female preponderance was noted in the study with a percentage of 57% followed by 43% males. Most of the patients (68%) had history of generalized lesions while 32% of the patients gave history of localized lesions. 27 (27%) cases give a definite family history, out of which 19 (70%) patients was the 1st degree relative and 8 (30%) cases were 2nd degree relative. Out of 100 patients, 93[93%] were not associated with any disease while diabetes mellitus was seen in 1(1%), hypertension in 4(4%), bronchial asthma in 1(1%), and hypothyroidism in1 (1%) patient. Key Words: vitiligo, familial, association
INTRODUCTION Vitiligo is a common, acquired, pigmentary disorder of skin, mucous membrane resulting from the destruction of functional melanocytes in epidermis and hair follicle which affects 1-2% of the general population, without racial differences1,2. Recent studies show that complex autoimmune, neural and self-destructive mechanisms are involved in its pathogenesis. Vitiligo is frequently associated with familial clustering and approximately 20% of probands have at least one affected first-degree relatives3,4 The risk for first degree relatives of patients with vitiligo to develop the disease is increased by seven to ten fold compared with the risk for the general population.5 Various studies suggest that patients with vitiligo have an increased risk of developing autoimmune disease such as thyroid disease, Addison's disease, pernicious anaemia, diabetes mellitus and alopecia areata.6
MATERIALS AND METHODS This was a single centered, cross-sectional descriptive study aimed at studying the epidemiological factors of vitiligo performed with the approval of the institutional ethical committee. 100 self reporting patients of vitiligo of any age and either sex, diagnosed on the basis of history and clinical examination were evaluated on a preformed proforma for the age of onset, sex ratio i.e male and female ratio, role of hereditary factors and association with other diseases. Inclusion/ Exclusion Criteria: The cases with the white patches due to secondary causes and those who were not willing to get enrolled in the study were excluded and the rest were included in the study.
RESULTS
Figure 1: Sex Figure 2: Age
Figure 3: Lesions Figure 4: Family History
Figure 5: Association with Other Diseases
Among 100 patients, females dominated the study with a percentage of 57% whereas only 43% were males as shown in figure 1. Majority of patients were in the age group of 26-35 years seen in figure 2. Most of the patients 68% had history of generalized lesions while only 32% of the patients gave history of localized lesions, figure 3. 27 (27%) cases give a definite family history, out of which 19 (70%) patients was the 1st degree relative and 8 (30%) cases were 2nd degree relative described in figure 4. Out of 100 patients, 93 (93%) were not associated with any disease while diabetes mellitus was seen in 1 (1%), hypertension in 4 (4%), bronchial asthma in 1 (1%), and hypothyroidism in 1 (1%) patient as shown in figure 5. The lower limb was the commonest site of involvement in 44 (44%) patients followed by upper limb, trunk, back and neck. DISCUSSION Vitiligo is considered to be a multifactorial disorder. An assortment of hypotheses, such as genetic, neural, biochemical (autocytotoxic), and autoimmune have been put forth to elucidate it’s etiopathological mechanism. Clinically, vitiligo is classified depending upon the site and extent of involvement into following types: generalized which is the most common, segmental, localised or focal, universal, acro-facial and mucosal type. Current clinical recommendations for vitiligo that is limited to only a few patches include treatment with topical agents such as corticosteroids and calcineurin inhibitors, and localised NB-UVB phototherapy such as excimer laser. For more extensive or spreading disease, whole body NB-UVB phototherapy is recommended. Surgical treatments are reserved for stable vitiligo and especially for vitiligo that is non-responsive to previous treatments areas. In our study, the female to male ratio was 1.3:1 which is different from the other studies.7,8,9 The females outnumbered males in our study presumably because social stigma and marital concerns prompt women to seek early consultation. In 30% of the patients, the age of onset was 26-35 years. However, other study10 showed the age of onset to be between 40 and 60 years. There was a definite family history of vitiligo in 27% of our patients; first-degree relatives were affected in 70% patients. Vitiligo has a polygenic or autosomal dominant inheritance pattern with incomplete penetrance and variable expression.11,12 Familial occurrence has been reported to be in the range of 6.25% to 30%.13 Positive family history is considered to be a poor prognostic factor for vitiligo. In our study, vitiligo vulgaris was the most common type observed, followed by localised vitiligo. The frequency of distribution of clinical types of vitiligo varies in different studies. According to the some studies14 generalized vitiligo was found to be more common. No significant systemic illnesses were observed in our study. The association of vitiligo with thyroid disease was 1% in our study but was reported to be 12% by Gopal et al.15 Diabetes mellitus is found in 1% to 7% of patients with vitiligo.17 although it was seen in 1% of the patients in our study.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home