|
Table of Content - Volume 3 Issue 3- September 2016
A comparative study of serum magnesium in type II diabetes mellitus patients and non diabetics and its correlation with treatment modality and duration of diabetes
Omkar R Patil1, Sanjay T Thorat2*, Mayur Kondewar3
1,3Jr. Resident, 2Associate Professor, Department of Medicine Krishna Institute of Medical Sciences, Karad, Maharashtra, INDIA. Email: omkarpatil5511@gmail.com
Abstract Background: Magnesium (Mg) deficiency is a common problem in diabetic patients. Deficiency of Mg may increase the incidence of diabetes mellitus (DM). In this study, our aim was to evaluate level of serum magnesium in type II DM patients and non diabetic individuals and its correlation with duration of diabetes and treatment modality. Material and Methods: 140 patients of type II diabetes mellitus in patients and out patients of tertiary care hospital between were included in the study. Also 140 non diabetic age and sex matched patients or relatives of patients attending opd during the same period were included in the study under the control group. Results: The mean age of cases was 57.06 ± 12.77 years while age of controls was 56.67 ± 12.7 years. This small difference was statistically not significant. There was no significant difference between mean serum Mg2+ values of male and female patients. (‘p’ = 0.18). The mean serum Mg2+ level in controls was 1.96 ± 0.18 mg/dl, which was significantly higher than the mean Mg2+ level of cases (1.69 ± 0.29 mg/dl). This difference was statistically significant. (‘p’< 0.001). Longer duration of diabetes has statistically significant influence on low levels of serum magnesium in diabetic subjects under study. (X2=15.353, R.R.= 0.46; ‘p’<0.0001). Amongst patients serum magnesium levels are significantly low in insulin treated patients as compared to those with OHA. (X2=5.884, R.R.=1.632, ‘p’=0.01). Conclusion: There is negative correlation between serum magnesium level and duration of diabetes mellitus type II. Serum magnesium levels are significantly low in insulin treated patients as compared to those with OHA. Key Words: Diabetes mellitus type II, duration of diabetes, serum magnesium, treatment modality.
INTRODUCTION Diabetes mellitus is the most common endocrine disorder, encountered in practice. The incidence of diabetes is increasing at a rapid pace and is evolving into an epidemic. The worldwide prevalence of diabetes mellitus has risen dramatically over the past two decades, from an estimated 30 million cases in 1985 to 177 million cases in 2000. Based on current trends more than 360 million individuals will have diabetes by year 2030. Since the 1940s, it has been reported that T2DM is associated with hypomagnesemia.1,2 Low serum magnesium (Mg2+) levels have been reported in large cohorts of patients with T2DM.3 In T2DM, the prevalence of hypomagnesemia ranges between 14 and 48% compared with between 2.5 and 15% in healthy control subjects.2 Hypomagnesemia is associated with a more rapid, and permanent, decline in renal function in patients with T2DM.4 In addition, epidemiological studies consistently show an inverse relationship between dietary Mg2+ intake and risk of developing T2DM.5 Several patient studies have shown beneficial effects of Mg2+ supplementation on glucose metabolism and insulin sensitivity.(6-8) Recently, Rodríguez-Morán et al.9 published an excellent overview of the clinical studies addressing the role of Mg2+ in T2DM. In our review, we will focus on the molecular mechanisms underlying these clinical observations. Magnesium modulates glucose transport through the membrane and it is a cofactor in several enzymatic reactions involving glucose oxidation. Its deficiency may increase insulin résistance. The reasons for magnesium deficiency in diabetes are not very clear. This could be due to higher urinary loss and lower dietary intake/impaired absorption10. Studies have shown that magnesium levels are lower in patients with diabetes compared with non diabetic controls.
MATERIALS AND METHODS It is a case control study. 140 clinically diagnosed and confirmed cases of Type II DM without any complications attending the medicine outpatient department of tertiary care center were taken as cases. 140 age and sex matched healthy subjects as controls. Study duration was one year. Informed consent was taken from the subjects. Patients were diagnosed as Type II DM on the basis of Clinical history and WHO criteria. Age group between 30 years to 70 years was included in the study. Pregnant and lactating women, subjects currently taking nutritional supplements, magnesium containing laxatives, diuretics/alcohol were excluded in both groups. A sample of 3 ml venous blood was collected in both fasting and post prandial state. FBS and PPBS were estimated by using Glucose oxidase peroxidase method. Serum magnesium was estimated by Xylidyl Blue method. Estimations were done using semi auto analyser Stat Fax 3300. Glycated hemoglobin was estimated using Nycocard Reader II. Data was expressed in terms of mean ± SD. Chi- square test was applied to estimate the difference between the two groups of population. Unpaired ‘t’-test was used to study the changes in serum magnesium levels. Pearson correlation between the study variables is performed to establish the relationship. P value <0.05 was considered significant.
RESULTS This was a comparative case control study conducted on 140 patients with clinically diagnosed type II diabetes mellitus and 140 healthy controls. Serum magnesium was estimated, analyzed and correlated with duration of diabetes and treatment modality. The results are expressed as mean ± standard deviation.
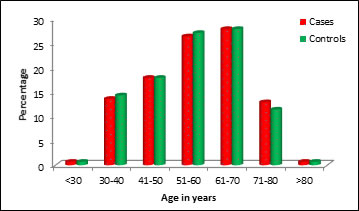
Table 1: Age distribution of cases and controls
Figure 1: The age distribution of cases and controls is depicted in Table 1. The mean age (in years) of 140 cases was 57.06±12.77and that of 140 controls was 56.67±12.70Samples are age matched with P=0.800, Student t test.
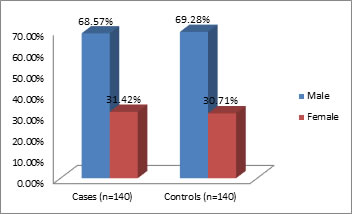
Table 2: Gender distribution of cases and controls
Figure 2: Gender distribution among the study population
Out of 140 cases, 96 (68.57%) were males and 44 (31.42%) were females. Out of 140 controls 97 (69.28%) were males and 43 (30.71%) were females and it was not significant. (‘p’ = 0.4) (Table 2)
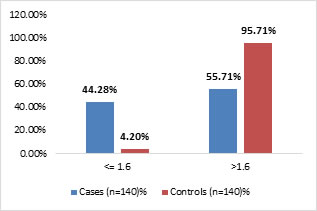
Table 3: Comparison of serum magnesium levels between controls and cases
Test: Unpaired ' t' test, Result: p<0.0001 Comment: There is highly significant difference in mean values of serum magnesium levels as observed in diabetic and nondiabetic individuals. In the present study the values below 1.6 mg/dl are considered as low.
Figure 3: Comparison of serum Mg++ level in case and control population
Table 4: Correlation of serum magnesium with duration of diabetes mellitus
The mean serum magnesium level was maximum in patients with lesser duration of illness (1-6 years), while that was minimum (1.53 ± 0.19) in patients with duration of illness more than 12 years. This difference was statistically significant (‘p’ < 0.001)
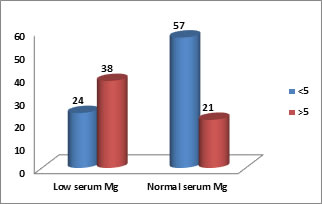
Table 4(a)
This table is showing there are 24 diabetic patients out of 81 diabetic patients having low serum magnesium whose duration of diabetics is <5 and 38 diabetic patients out of 59 diabetic patients having low serum magnesium whose duration of diabetes is >5 years. Longer duration of diabetes has statistically significant influence on low levels of serum magnesium in diabetic subjects under study. (X2=15.353, R.R=0.46; ‘p’<0.0001) Applying chi square test, ‘p’<0.0001, shows significance
Figure 4: Correlation of serum magnesium with duration of diabetes mellitus
Figure 4 a: Correlation of serum magnesium with duration of diabetes mellitus
Table 5: Correlation of serum magnesium with treatment modality in diabetes mellitus
51.5% patients among < 1.5 mg% Mg group, was taking Insulin as compared to 30.2% receiving only OHAs. While 56.6% among those who had normal Serum Mg level received OHAs. The Mean Serum Mg level of Only Insulin group was lowest (1.60±0.28) followed by OHA+ Insulin group and highest in Only OHA group. This difference was statistically significant (‘p’ < 0.05)
Table 5(a)
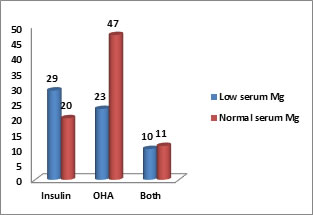
In our study there are 29 out of 49 diabetic patients having low serum magnesium level with treatment with insulin and 23 out of 70 diabetic patients having low serum magnesium level with OHA and 10 out of 21 diabetic patients having low serum magnesium level with both treatment modalities. Amongst patients serum magnesium levels are significantly low in insulin treated patients as compared to those with OHA. (X2=5.884, R.R.=1.632, ‘p’=0.01) Applying chi square test, ‘p’=0.01, shows significance
Figure 5: Correlation of serum magnesium with treatment modality in diabetes mellitus
DISCUSSION Diabetes mellitus is a complex and multifactorial disease indulging severe insulin dysfunction in conjunction with gross abnormalitiesin glucose homeostasis, lipid and protein metabolism. Many trace elements are important for human metabolic function. Numerous studies have demonstrated the essential roles of elements such as magnesium carbohydrate metabolism10. In view of this, the present study had been taken up to assess clinical utility of promising biochemical marker like serum magnesium which is inexpensive and can be of some diagnostic and prognostic significance. In this case control study, we have compared the above biochemical parameter in 140 cases with type II diabetes mellitus and 140 apparently healthy age and sex matched normal controls. The significance of the parameter between the two groups and its correlation with duration and treatment modality is analyzed and discussed. The present study shows that longer duration of diabetes mellitus has significant influence on serum magnesium levels. The groups with duration of diabetes > 5 years are showing increased number of cases with low serum magnesium as compared to group with duration of diabetes <5 years. Haquea et al.11 found a mean diabetic duration of 6.34 years in hypomagnesemic patients and concluded that serum magnesium level has no direct relationship with diabetic duration if the diabetes is well controlled. Longer duration of diabetes is associated with higher incidence of complications due to longer duration of uncontrolled diabetic status associated with lower magnesium levels. In our study, out of 49 patients receiving treatment with insulin, 29 are showing low serum magnesium level and out of 70 patients receiving treatment with OHA, 23 are showing low serum magnesium levels and out of 21 patients receiving treatment with both (insulin + OHA) , 10 are showing low serum magnesium levels and the association is statistically significant. Mohamed MurtuzaKause studied 50 diabetic and 50 non diabetic controls and concluded that a serum magnesium levels were significantly lower in insulin treated group compared to OHA treated group. The mean serum magnesium levels in oral hypoglycemic (OHA) group, insulin group and insulin + OHA group were 2.02 mg/dl, 1.59 mg/dl, 1.25 mg/dl respectively.12 In our study it is 1.75 mg/dl, 1.60 mg/dl, 1.70 mg/dl respectively.
CONCLUSIONS Serum magnesium levels are significantly low in diabetes mellitus type II as against age and sex matched non-diabetic individuals. Age and sex has no significant influence on serum magnesium levels in diabetes. Longer duration of diabetes mellitus is found to be significantly associated with decreasing levels of serum magnesium, in this study. There is negative correlation between serum magnesium level and duration of diabetes mellitus type II. Serum magnesium levels are significantly low in insulin treated patients as compared to those with OHA.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home