|
Table of Content - Volume 3 Issue 3- September 2016
A study of profile of snake bite patients and outcome at tertiary health care centre
Nitesh Suraj Chhajed1, Vinod Ramchandra Baviskar2*
1Assistant Professor, 2Associate Professor, Department of General Medicine, Dr. Ulhas Patil Medical College and Hospital, Jalgaon, Maharashtra, INDIA. Email: drniteshschhajed@gmail.com
Abstract Background: According to the World Health Organization (WHO), an estimated 5 million snakebite cases and about 100,000 deaths due to snakebite occur every year. The incidence is particularly high in rural areas of Africa, Asia, Oceania, and Latin America where venomous snakes are abundant and human activities, mainly agriculture, hunting, animal husbandry, and fishing, increase the risks of man/snake encounters. Aims and objectives: To Study the profile of Snake bite patients attending the tertiary care centre and its outcome. Materials and Method: In the present record based descriptive observational study all the cases of snake bite admitted in the institute during the January 2016 to December 2016 were enrolled. A total of 253 cases of snake bite were admitted in medicine wards during the study period. A detailed information regarding demographic and epidemiological parameters such as age, sex, residence, site of bite and place of bite, type of snake if identified, etc., was recorded. Clinical signs and symptoms were also recorded. Subsequent information regarding the outcome of the patient was also obtained from the case paper of the patient. Results: Majority of the patients (29.25%) were in the age group of 21-30years of age, followed by 31-40 years (21.34%) and 41-50 years (16.60%). Majority of the patients were male (64.03%). Majority of the patients (90.12%) with snake bite were from rural area. Giddiness was reported in 1.98% patients whereas drowsiness and unconsciousness was observed in 1.58% and 0.78% patients respectively. Majority of the cases of snake bite were observed during the monsoon season (63.24%) followed by winter season (21.34%) and summer (15.42%). The most common timing of snake bite was night time (36.36%). 75.49% bites were by non poisonous snakes whereas 18.18% bites were by vasculotoxic and 6.32% were by neurotoxic snakes. The case fatality rate of neurotoxic snake bite was 12.50% whereas that of vasculotoxic snake bite was 2.17%. Conclusion: Majority of the cases of snake bite were observed during the monsoon season and at night time. 75.49% bites were by non poisonous snakes whereas 18.18% bites were by vasculotoxic and 6.32% were by neurotoxic snakes. Giddiness, drowsiness, Ptosis, Altered sensorium and unconsciousness were the common presenting symptoms observed in poisonous bites. The case fatality rate of neurotoxic snake bite was 12.50% whereas that of vasculotoxic snake bite was 2.17%. Key Words: Snake bite, Outcome, neurotoxic snake bite, vasculotoxic snake bite.
INTRODUCTION Globally, snakebite envenomation is a serious health problem and according to the World Health Organization (WHO), an estimated 5 million snakebite cases and about 100,000 deaths due to snakebite occur every year.1,2 The incidence is particularly high in rural areas of Africa, Asia, Oceania, and Latin America where venomous snakes are abundant and human activities, mainly agriculture, hunting, animal husbandry, and fishing, increase the risks of man/snake encounters.3 The frequency of snake bites is high during agricultural activities and most bites are inflicted when the snakes are inadvertently trodden upon by humans.4,5 Additionally, increasing deforestation, human migration, and recreational and nature camps in forest areas also contribute toward snake bite envenomation.6 In light of these observations, the WHO has listed snake bite envenomation as a serious health problem and categorized it within the list of neglected tropical diseases.7India’s 70% population depends on agricultural occupation. Snakebite is major occupational health hazard specially related to farmers who work in open field in our country. On an average, nearly 2,00,000 persons fall prey to snake-bite per year in India and 35,000-50,000 of them die every year8. But data on the morbidity and mortality of snakebite is unreliable due to improper reporting system. Indian states with high incidence of snakebite cases are Tamil Nadu, West Bengal, Maharashtra, and Uttar Pradesh and Kerala9. Maharashtra reports an incidence of 70 bites per 100,000 population and a mortality of 2.4 per 100,000 persons per year10. A majority of deaths in India are caused by envenoming by Kraits and Cobras10. Considering an agricultural occupation and major annual incidence, it is important to study the clinical profile of neuroparalytic snake bite.
MATERIALS AND METHOD The present record based descriptive observational study was carried out in the Dr. Ulhas Patil Medical College and Hospital. For the study purpose all the cases of snake bite admitted in the institute during the January 2016 to December 2016 were enrolled. A total of 253 cases of snake bite were admitted in medicine wards during the study period. A detailed information regarding demographic and epidemiological parameters such as age, sex, residence, site of bite and place of bite, type of snake if identified, etc., was recorded. Clinical signs and symptoms were also recorded. Subsequent information regarding the outcome of the patient was also obtained from the case paper of the patient. Results were expressed as frequency percentages and presented with graphs and tables.
RESULTS Table 1: Agewise distribution of patients (n=253)
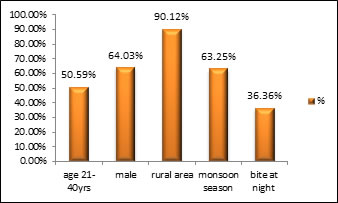
It was observed that there were total 253 patients of snake bite admitted in the institute and it was seen that majority of the patients (29.25%) were in the age group of 21-30years of age, followed by 31-40 years (21.34%) and 41-50 years (16.60%). It was seen that majority of the patients were male (64.03%). It was observed that majority of the patients (90.12%) with snake bite were from rural area.
Table 2: Distribution of patients according to symptom
*Multiple responses were obtained It was observed that majority of the patients were conscious and well oriented (95.23%). Giddiness was reported in 1.98% patients whereas drowsiness and unconsciousness was observed in 1.58% and 0.78% patients respectively.
Table 3: Distribution of patients according to season, month and type of Bite
It was seen that majority of the cases of snake bite were observed during the monsoon season (63.24%) followed by winter season (21.34%) and summer (15.42%). The most common timing of snake bite was night time (36.36%) followed by evening (26.69%) and morning hours (20.16%). It was observed that 75.49% bites were by non poisonous snakes whereas 18.18% bites were by vasculotoxic and 6.32% were by neurotoxic snakes.
Figure 1: Distribution according to associated factors
Table 4: Case fatality rate of snake bite
It was observed that out of total 253 cases of snake bite; death was reported in 3 cases. Thus the case fatality rate in the present study was 1.57%. The case fatality rate of neurotoxic snake bite was 12.50% whereas that of vasculotoxic snake bite was 2.17%.
DISCUSSION Snake-bite is an important and serious medicolegal problem in many parts of the world, especially in South Asian countries. It has been estimated that 5 million snake-bite cases occur worldwide every year, causing about 100,000 deaths.11 It was observed that there were total 253 patients of snake bite admitted in the institute and it was seen that majority of them were young patients. 29.25% were in the age group of 21-30years of age, followed by 31-40 years (21.34%) and 41-50 years (16.60%). Similar findings were also observed by Gaurav Bhalla et al12, Halesha B.R et al13 and Punde DP et al.14 It was seen that majority of the patients were male (64.03%). It was observed that Males are affected more often than the females, as they are actively engaged in farming and other outdoor activities. Our finding swere comparable with findings reported by Basu J15, Bhat RN16, Gaurav Bhalla et al12, Halesha B.R et al13 and Saini RK17 in their studies. Men are the dominant earning members of the family in India, working outdoors and sleeping in the farmyards during harvesting. This could probably be the main cause of the male preponderance which was seen in our study. It was observed that majority of the patients (90.12%) with snake bite were from rural area. As predominantly rural population that was dependent on agriculture as an occupation and more porn for snake bite. Our findings concurred with those of earlier studies 14,18-21. It was observed that majority of the patients were conscious and well oriented (95.23%). Giddiness was reported in 1.98% patients whereas drowsiness and unconsciousness was observed in 1.58% and 0.78% patients respectively. It was seen that majority of the cases of snake bite were observed during the monsoon season (63.24%) followed by winter season (21.34%) and summer (15.42%). Similar findings were also reported by Arshad Anjum et alRB-24, Virendra Patil et al22 and Monteiro FNP et al23. Most of the human snakebites occur during the monsoon season, because of the flooding of the habitats of the snakes and their prey. The most common timing of snake bite was night time (36.36%) followed by evening (26.69%) and morning hours (20.16%). The findings were comparable with findings observed by Bhavesh Jarwani et al24 and Arshad Anjum et al25 in their studies. It was observed that 75.49% bites were by non poisonous snakes whereas 18.18% bites were by vasculotoxic and 6.32% were by neurotoxic snakes. The findings were comparable with the findings reported by Rekha Thapar et al26 and Sudhir Prabhu Haladi et al27. It was observed that out of total 253 cases of snake bite; death was reported in 3 cases. Thus the case fatality rate in the present study was 1.57%. The case fatality rate of neurotoxic snake bite was 12.50% whereas that of vasculotoxic snake bite was 2.17%. Kulkarni ML28, IF Inamdar 29 and Hati AK18 reported similar findings in their study.
CONCLUSION Thus we conclude that snake bite has higher prevalence among the young male from rural area. Majority of the cases of snake bite were observed during the monsoon season and at night time. 75.49% bites were by non poisonous snakes whereas 18.18% bites were by vasculotoxic and 6.32% were by neurotoxic snakes. Giddiness, drowsiness, Ptosis, Altered sensorium and unconsciousness were the common presenting symptoms observed in poisonous bites. The case fatality rate of neurotoxic snake bite was 12.50% whereas that of vasculotoxic snake bite was 2.17%.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home