|
Table of Content - Volume 3 Issue 3- September 2016
Study on complications following ischemic stroke in a tertiary care hospital in South India
Geeta Panicker1, Edwin J George2*, G George3, Deepak K P4
Department of Medicine, Amala Institute of Medical Sciences, Thrissur, Kerala, INDIA. Email: edwin_edzz@yahoo.co.in
Abstract Background: Patients with acute Ischaemic stroke are at risk for Neurological and Medical complications. Identifying the frequency of complications could enhance timely treatment and improve clinical outcome. Methods: We analysed the frequency of the complications following Ischaemic stroke in 100 consecutive patients diagnosed in Medical and Neurology wards of Amala Institute of Medical Sciences. Results: Complications during hospital admission were recorded in 100 stroke patients. Specific complications were as follows. Neurological Complications – Recurrent stroke (2.8% of patients), seizure (5.6%), haemorrhagic transformation (2.8%), brain edema (2.8%) Acute confusional state – 5.6% Medical complications: Urinary tract infection in 23.1%, Pneumonia in 4.9%, Electrolyte imbalance –Hyponatraemia in 36.4%, Hypokalemia in 13.3%, Acute coronary syndrome in 0.7%, pressure sores is 0.7%. Conclusion: Our Prospective study has confirmed that post stroke complications particularly infections are common. However we have also identified complications relating to Electrolyte imbalance that are potentially preventable and may previously have been under estimated.
INTRODUCTION Cardio vascular diseases include some of the most common and devastating disorders, ischaemic stroke, haemorrhagic stroke and cerebro vascular anamolies like intracranial aneursym and arteriovenous malformation. A stroke is defined as an abrupt onset of focal neurological deficit that is attributable to a vascular pathologic processes Stroke is a major cause of morbidity and ranks third as a cause of death worldwide. The incidence of stroke varies among countries and increases exponentially with age. In western societies about 80% of strokes are caused by focal cerebral ischemia due to arterial occlusion and the remaining 20% are caused by haemorrhages. Thirty day case fatility rates of ischaemic stroke in western societies generally ranges between 10 and 17%. The likelihood of a poor outcome after stroke increases with increasing age, with the co- existence of disease such as ischemia heart disease, diabetic mellitus and with increasing size of infarct and according to the infarct site. Mortality in the first month after stroke has been reported to range from 2.5% in patients with lacunar infarcts to 18% in patients with space occupying hemispheric infraction. Patients who have had an acute stroke are at risk of developing a wide range of complications secondary to their stroke. These complications are important because they cause death or delay successful rehabilitation. Several studies have shown that although deaths within a few days of stroke are usually the direct consequence of brain damage, those occurring over the following weeks are mainly due to potentially preventable problems . Acute stroke patients are at risk of developing a wide range of medical complications secondary to stroke. These complications may either directly lead to death or prevent optimal recovery. Previous studies have shown that medical complications are both common and are related to a poor outcome. It has also been suggested that attention to potential medical complications after stroke may reduce mortality and disability resulting from stroke. It has also been suggested that the effectiveness of organized stroke care in reducing mortality may be due to improvement in the prevention, identification and treatment of secondary complication. Complication rate may also be useful measure of outcome in comparative studies and they have been used in both non randomized and randomized controlled trails of stroke units. Most of the published studies on post stroke complications have focused on individual problems in isolation such as seizure, venousthromboembolism or depression. Data from randomized and other trials indicate that patients who receive care in a stroke unit are more likely to survive, regain independence and return home than are those who do not receive such care.
MATERIAL AND METHODS All stroke patients were treated in Neurological and medical wards. Diagnosis of stroke was based on history of disease, physical examination and confirmed by Neuroimaging. Electrolytes analyzed in this study was sodium and potassium. Sodium level in a range of 135-153 meq/L was defined as normal. Potassium level in a range of 3.5-5meq/L was defined as Normal. Hyponatraemia was defined when the level of sodium was below 135 meq/L. Hypokalaemia was the level of potassium below 3.5 meq/L. Hyperkalaemia was the level above 5meq/L. Hypernatraemia was the level of sodium above 153 meq/L. Patients with stroke are particularly vulnerable to UTI, due to increased risk from bladder dysfunction and increased foley’s catherter use . UTI is associated with poor Neurological outcomes, longer hospital stays and increased cost of care after stroke. According to a study by Davenport et al UTI was noted in 16% of patients following acute stroke. Post stroke pneumonia has been used to describe pneumonia that occurs early after stroke. The term stroke associated pneumonia has been used for the first time by Hilken et al. referring to this concept. Stroke associated pneumonia is described as early when it happens in the first 72 hrs of admission to the hospital. stroke associated pneumonia is divided into Acute (When pneumonia develops within a month of stroke) and chronic (When it occurs later than a month) according to one classification. In this study we deal only with Acute complication ie complication occurring within one month following stroke. Traditionally stroke associated pneumonia is thought to be secondary to aspiration. Aspiration and its related risk factors such as impaired level of consciousness and dysphagia have been found to be important risk factor for stroke associated pneumonia across different clinical studies. According to a study by Welmar et al., pneumonia was one of the most frequent complication (7.4%) following acute Ischaemia stroke. Patients with stroke have a relatively high risk of deep vein thrombosis because of immobility and increased prothrombotic activity. DVT in paralysed leg of a stroke patient was described as early as 1810 by Feriar. DVT develops most often between 2-7 days after stroke. About 80% of all DVT’s occur within the first 10 days. In a study by SKAF et al., DVT was noted in 0.74% of patient with Ishaemia stroke. About a quarter of the patients who survive their stroke have a recurrent stroke within 5 yrs Approximately 9% of patients with acute cerebral infarction have a Myocardial infraction at the same time or within a few days following this event. The co-existence of coronary artery disease with cerebral ischaemia influence the prognosis. Myocardial infraction or sudden death is the leading cause of death in patients with cerebrovascular disease. Early mobilization, frequent turning and skin examinations and use of alternating pressure mattress should be considered to prevent skin damage after Ischaemia stroke. Following an Ischaemia stroke patients are at risk of multiple neurological complication including cerebral edema, seizure, haemarrhagic conversion of an ischaemia stroke. Of these complications, cerebral oedema is the leading cause of death in these patients.
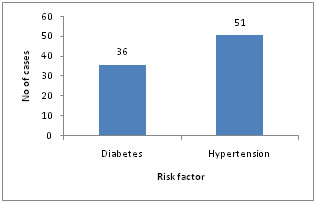
RESULTS During the 6 months study period, 100 Ischaemic stroke patients were identified and enrolled in the study. In this study, 48.3% were males. The mean age was 75.5 yrs. The commonest risk factor was hypertension with 51 patients followed by diabetes mellitus with 36 patients out of 100. On admission the mean systolic blood pressure was 153.38 and diastolic blood pressure 87.78.
Figure 1:
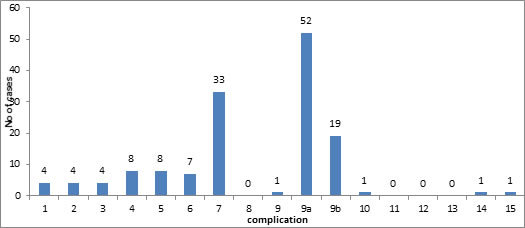
Figure 2
Complications
All the complication developed within one month after stroke with an early onset seen particularly for infection and electrolyte imbalance. As acute complications were being studied some complications like bedsores were least noted.
DISCUSSION In this study, the incidence of electrolyte imbalance was high. This is comparable with study by Mieke, et al, where 45.9% of patients with electrolyte imbalance were noted. 8.2% of which had sodium disturbance, 40% with potassium disturbance Hyponatraemia, Hypokalaemia are the commonest type of disturbance. Even though there are some data about large number of electrolyte disturbances in acute stroke setting. Reports on association between electrolytes imbalance and severity of acute stroke are still in limited number. In our study, urinary tract infection was noted in 23.1% patients. According to a study by Davenport et al, UTI was noted in 16% of patients following acute stroke. Pneumonia was seen in 4.9% of patients of all patients. According to a study by Welmar et al, pneumonia was one of the most frequent complication (7.4%) following acute Ischamaeic stroke. DVT was not seen in any of the patients in our study. This is comparable with study by SKAT et al, who have recorded a low frequency of DVT in 0.74% of patients with Ischaemia stroke. Our findings appear to confirm previous studies that showed that there are relatively low frequency of the symptomatic complications of recurrent stroke, post stroke seizure, clinical deep vein thrombosis. We have also confirmed the relatively high frequencies of urinary tract infection, chest infection and electrolyte imbalance. Various studies have concluded that there is a strong association between post stroke complications and poor outcome and have suggested that complications may act as barriers to recovery. This raises the possibility that rigorous attention to detail in the prevention and early treatment of complications could, improve the stroke outcome. Prevention Patients with Neurologic deficits leading to immobility are at higher risk of pneumonia. Patients following Ischaemic stroke should be mobilized early in the hospital stay. Medications that reduce the level of consciousness should be discontinued unless specifically indicated. Electrolyte imbalances are common after stroke, steps for detection and correction of the same should be taken as early as possible. Urinary tract infections, following the usage of indwelling catheters are commonly seen, which should be avoided if possible or removed at the earliest. Early mobilization, frequent turning and skin examinations and use of alternating pressure mattresses should be considered to prevent skin damage after ischaemic stroke. Anti platelet therapy is a corner store for secondary prevention of Ischaemic stroke. Statins has been found to be useful in secondary prevention of Ischaemic stroke. The benefit of blood pressure reduction, management of Diabetes Mellitus, following an ischaemic stroke is useful for secondary prevention of ischaemic stroke. Counselling regarding life style modification is important following an ischaemic stroke. In short, prevention comprises of Respiratory and cardiac care, fluid and metabolic management, blood pressure and diabetic control ,avoidance of smoking and alcohol intake and care to avoid Deep vein thrombosis, Urinary tract infection and bedsores.
Table 1:
CONCLUSION Our prospective study has confirmed that post stroke complication particularly infections are common. However we have also identified complications relating to electrolyte imbalance that are potentially preventable and may previously have been under estimated.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home