|
Table of Content - Volume 4 Issue 2- November 2016
Study of correlation between dyslipidemia and cerebrovascular accidents in non-diabetic patients at tertiary health care center
Raju Talawar1, Darshna Makwana2*
1Assistant Professor, Department of General Medicine, J.N.M.C. Nehru Nagar, Belagavi, Karnataka-590010, INDIA. 2Assistant Professor, Department of General Medicine, B.J.M.C. Asarwa, Ahmedabad, Gujarat, INDIA. Email: drrajutalawar@gmail.com
Abstract Background: According to the Indian Council of Medical Research there were 930,985 cases of stroke in 2004 in India. Aims and Objectives: to Study correlation between dyslipidemia and cerebrovascular accidents in non-diabetic patients at tertiary health care center. Methodology: All non-diabetic patients with features of stroke admitted to tertiary care hospital from December 2013 to December 2015 were taken for the study. Data will be collected by means of case record form. All non-diabetic patients of cerebrovascular accidents were enrolled in this study with informed consent and detailed patient information. Scale (mNIHSS)10, Modified Rankin Scale (MRS)11 etc. was used for the assessment of outcome of Stroke. The statistical analysis done by t-test calculated by SPSS 19 version software. The statistical analysis done by t-test calculated by SPSS 19 version software. Result: The mild mNIHSS scale contributes 64% of whole population, moderate and severe mNIHSS scale contributes 26% and 10% of study population. The p value of all other lipids is also significant but r value is not significantly high. MRS score showed a good clinical outcome with reduction in LDL levels and the corresponding P value is 0.26 and r value of 0.15 which is significant. Conclusion: It can be concluded from our study that there good co-relation is found with LDL i.e. good clinical outcome was with reduced level of it so the intervention should be directed specifically to reduce the level it. Key Words: Dyslipidemia, Cerebrovascular accidents, Modified National Institutes of Health Stroke, Scale (mNIHSS), Modified Rankin Scale (MRS).
INTRODUCTION According to the Indian Council of Medical Research there were 930,985 cases of stroke in 2004 in India 1 and the National Commission of Macroeconomics and Health has estimated that there will be 1.67 million stroke cases in India by 20152. Stroke is also a leading cause of morbidity, with 20% of survivors requiring institutional care after3 months and 15-30% remaining permanently disabled 3. Of all strokes, 88% are classified as ischemic, and the remainder 12% comprise of hemorrhagic, either subarachnoid (9%) or intracerebral (3%)4. Dyslipidemia has been a known major risk factor for coronary heart disease. However more recently, it has been established as a risk factor in cerebrovascular disease 5. Elevated low density lipoprotein cholesterol (LDL-C) is a risk factor for coronary artery disease whereas high levels of high-density lipoprotein cholesterol (HDL-C) are protective6-10.
MATERIAL AND METHODS All non-diabetic patients with features of stroke admitted to tertiary care hospital from December 2013 to December 2015 were taken for the study. Data will be collected by means of case record form. All non-diabetic patients of cerebrovascular accidents were enrolled in this study with informed consent and detailed patient information. Patients having diabetes mellitus type 1 or 2, impaired glucose tolerance, Patients with history of head injury, Patients on drug therapy such as OCP’s, steroids, diuretics and anticoagulant drugs, Patients already diagnosed with dyslipidaemia, Patients on lipid lowering agents, Diagnosed case of liver diseases, kidney diseases, pancreatitis, coronary artery disease and thyroid disease, Diagnosed case of malignancy, Patients lost for follow up were excluded from the study. In all the patients Serum Total cholesterol, Serum HDL cholesterol, Serum LDL cholesterol, Serum TG, Serum VLDL etc. was estimated. Modified National Institutes Of Health Stroke Scale(mNIHSS)10, Modified Rankin Scale (MRS)11 etc. was used for the assessment of outcome of Stroke. The statistical analysis done by t-test calculated by SPSS 19 version software.
RESULT
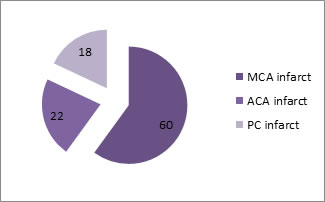
Table 1: CT Scan Of Brain (Territory Infarct Distribution)
Severity of ischemic stroke at onset was measured using NIHS Scale. Mild (0-6)- 32 pts, Moderate (7-14)- 13 pts, Severe (<14)- 5 pts. Among the whole population mid mNIHSS scale (0-6) was found in 32 patients, moderate NIHSS scale (7-14) was observed in 13 patients and severe mNIHSS scale (>14) was found in 5 patients. The mild mNIHSS scale contributes 64% of whole population, moderate and severe mNIHSS scale contributes 26% and 10% of study population
Table 1: Co-relation between mNIHSS score and Lipid profile:
The study showed significant correlation between NIHSS measured by Pearson correlation value and p value of lipid abnormalities at onset of stroke. The study showed significant p value for LDL (0.00) and also high r value for LDL (0.49). The p value of other lipids is also significant but r value is not significantly high.
Table 3: Co-relation between MRS and Lipid profile
MRS score showed a good clinical outcome with reduction in LDL levels and the corresponding P value is 0.26 and r value of 0.15 which is significant.
DISCUSSION Epidemiological studies suggest that patients with elevated lipid levels are at higher risk for CVA. Although serum lipids have been incriminated in the pathogenesis of atherosclerosis, very little is known concerning the possible inter-relationship between abnormal levels of serum lipids and development of vascular complications. Belief in the possibility of such interrelationship arouse in part from the observation that lipid composition of the intima of the arteries resembles that of serum. Hence Dyslipidemia has emerged clearly as a major risk factor associated with increased risk of atherosclerosis. The relationship between atherosclerosis and elevated serum lipids is well established and aggressive treatment of dyslipidemia decreases the risk of stroke.1 Recent studies have shown that distribution of triglycerides and cholesterol within major lipoprotein classes are of importance for the development of atherosclerosis, which is the precursor to stroke.2 Hypercholesterolemia is a moderate risk factor for stroke.2 Elevated plasma concentration of low density lipoproteins (LDL) and low high density lipoprotein concentration (HDL) are associated with an increased risk of atherosclerosis.2 While there is an overwhelming amount of evidence relating high levels of serum total and LDL cholesterol and low levels of HDL cholesterol with coronary atherosclerosis, the relation between serum lipids, lipoproteins and cerebrovascular atherosclerosis is less clear.3 Studies of cholesterol levels in stroke patients have revealed results varying from insignificant changes to a moderate elevation. The mild mNIHSS scale contributes 64% of whole population, moderate and severem NIHSS scale contributes 26% and 10% of study population. Severity of ischemic stroke at onset was measured using NIHS Scale. Mild (0-6)- 32 pts, Moderate (7-14)- 13 pts, Severe (<14)- 5 pts.Among the whole population mid mNIHSS scale (0-6) was found in 32 patients, moderate NIHSS scale (7-14) was observed in 13 patients and severe mNIHSS scale (>14) was found in 5 patients. The mild mNIHSS scale contributes 64% of whole population, moderate and severe mNIHSS scale contributes 26% and 10% of study population. In our study there was significant p value for LDL (0.00) and also high r value for LDL (0.49). The p value of other lipids is also significant but r value is not significantly high.MRS score showed a good clinical outcome with reduction in LDL levels and the corresponding P value is 0.26 and r value of 0.15 which is significant.MRS score showed a good clinical outcome with reduction in LDL levels and the corresponding P value is 0.26 and r value of 0.15 which is significant. K Sreedhar found in 32 patients had elevated serum total cholesterol levels, of which 81.3% had ischaemic stroke and the rest haemorrhagic stroke. 10 patients had elevated serum triglyceride levels, of which 80% had ischaemic stroke and the rest haemorrhagic stroke. 33 patients had elevated serum low density lipoprotein levels of which 75.8% had ischaemic stroke whereas the remaining had haemorrhagic stroke
CONCLUSION It can be concluded from our study that there good co-relation is found with LDL i.e. good clinical outcome was with reduced level of it so the intervention should be directed specifically to reduce the level it.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home