|
Table of Content - Volume 4 Issue 2- November 2016
Vitamin D status in patients with hypothyroidism
Hari kishan jayanthi1, Sai Krishna Tulasi2*, Jagannadha Phaneendra D S3
{1Assitant Professor, 2Sr. Resident, Department of General Medicine} {3Assistant Professor, Department of Biochemistry} Kamineni academy of medical sciences and research, L. B. Nagar, Hyderabad, Telangana, INDIA. Email: drtsk86@gmail.com
Abstract Background: Vitamin D deficiency and hypothyroidism are common problems in India. Vitamin D not only has action on calcium metabolism, but its deficiency is considered as cause for autoimmune diseases. Currently, only animal trials are available, cause and effect relationship between vitamin D deficiency and autoimmune diseases is yet to be proved in human beings. Hypothyroidism is also known to have effects on calcium homeostasis. Our aim was to study vitamin D status in hypothyroid patients and compare it with normal controls. Subjects and Methods: We studied 50 patients with hypothyroidism and 50 normal controls who visited our outpatient department. Vitamin D levels and thyroid profile were sent in all 100 patients. Vitamin D deficiency was designated at <20ng/ml. Results: Vitamin D deficiency was found in 73% of patients with hypothyroidism. Even among hypothyroid patients, people with TSH under normal limits vitamin D deficiency prevalence (45% in hypothyroid patients) were comparable to that of normal controls (44% in controls). T test was applied between uncontrolled hypothyroid group and normal control group and p value was 0.0023, t= 2.9. There was no statistical significance difference between males and females t=1.3, p=0.08. There was negative correlation between TSH levels and vitamin D levels in patients with hypothyroidism suggesting the uncontrolled the hypothyroidism the lower would be the vitamin D levels. Conclusion: Vitamin D levels must be checked in all hypothyroid patients, specifically in people with age 50-59 years, uncontrolled hypothyroidism as both uncontrolled hypothyroidism and vitamin D deficiency may present with similar nonspecific complaints. Key Words: Vitamin D deficiency, Hypothyroidism, normal controls.
Calcitriol (vitamin D3) exerts its biologic functions by binding to a nuclear receptor, which then regulates transcription of DNA into RNA1. Long-standing vitamin D deficiency results in hypocalcemia accompanied by secondary hyperparathyroidism, impaired mineralization of the skeleton and proximal myopathy. Vitamin D deficiency also has been shown to be associated with an increase in overall mortality rates, including cardiovascular causes2. In Hypothyroidism, the exchangeable pool of calcium and its rate of turnover are reduced, reflecting decreased bone formation and resorption. In hypothyroidism levels of parathyroid hormone are often slightly increased with some degree of resistance to its action, levels of 1,25(OH)2D (dihydroxyvitamin D) are also increased3. Kozai et al showed in their experimental study in mice that thyroid hormones decrease plasma 1α,25-dihydroxyvitamin D levels through transcriptional repression of the renal 25-hydroxyvitamin D3 1α-hydroxylase gene (CYP27B1)4.
MATERIALS AND METHODS Inclusion Criteria
Exclusion Criteria
Study Area: The study was done in Kamineni hospital L.B.Nagar, Hyderabad. Kamineni Hospitals Pvt Ltd is a teritiary care super speciality hospital with a bed strength of more than 350. The General medicine OPD receives a daily average of about 40 patients and the daily inpatient ranges around 20 patients a day. Study Population: The study was done on 50 patients with Hypothyroidism (Test group) and 50 Non- Hypothyroid people (control group). In hypothyroid patients, who were on regular follow up and, also who had nonspecific complaints like generalized body pains and generalized weakness, Vitamin D levels and TSH were sent In normal patient coming to outpatients, having nonspecific complaints like generalized body pains, generalized weakness. Vitamin D and TSH were sent During the course of study in people who are non hypothyroid, on evaluation if, found to be hypothyroid they were included under the test group. Study Size: 50 people with hypothyroidism and, 50 people who are not known hypothyroid. Data Collection Technique and Tools: Vitamin D and TSH reports were collected from all the 100 cases and tabulated. Data Analysis: Data analysis was done using percentages, graphs and matched T test. Study Type: It’s an observational prospective study.
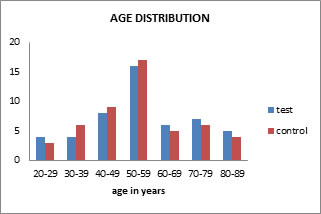
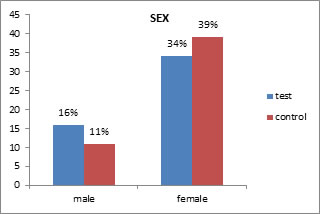
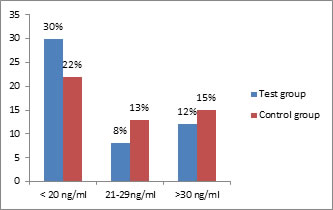
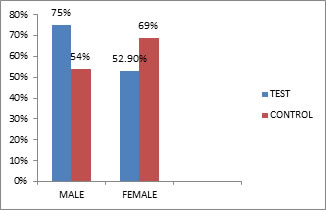
RESULTS Total 50 patients and 50 controls were studied. Maximum number of cases belonged to age 40-60 years in both test and control (Figure-1), 32% were in age group 50-59 years. 68% were females in test group and 78% were females in control group (Figure-2). Among the hypothyroid patients 40% patients were having normal TSH levels, 8% had TSH less than 0.34 uiu/ml, 52% had TSH >5.6 uiu/ml (table-1). In hypothyroid group 60% patients had vitamin D deficiency, 16% had vitamin D insufficiency. In control group 44% had vitamin D deficiency, 26% had vitamin D insufficiency (figure-3). Among age group 50-59 years 50% had vitamin D deficiency and 12.5% had vitamin D insufficiency. 73% of the hypothyroid patients with TSH > 5.6 uiu/ml had vitamin D deficiency, 15% had Vitamin D insufficiency. Amongst the hypothyroid patients with normal TSH levels, 45% patients had hypothyroidism, 20% had vitamin D insufficiency, this result was comparable with the normal controls were 44% had vitamin D deficiency, 26% had vitamin D insufficiency(table-1). T test was applied between vitamin D levels in people with uncontrolled hypothyroidism and control t= -2.9, P value was 0.0023. T test was applied between vitamin D levels in hypothyroid with normal TSH and control t= -0.5, P value was 0.28. Similarly T test was applied between vitamin D levels and TSH levels in normal controls t= 0.32, p= 0.37. In our study 75% of the males with hypothyroidism had vitamin D deficiency, where as in females with hypothyroidism it was 52.9%, in controls too, 54% of males had vitamin D deficiency, where as in females it was 41% (figure-4). T test was applied to vitamin D levels between males and females in hypothyroidism t-value was 1.37 and p-value was 0.087. T test was applied between vitamin D levels of males and females in control t-value were 0.66 and p-value 0.256. We have compared vitamin d levels between males with hypothyroidism and male controls t-value was 1.5 and p-value was 0.07. Similarly T test between hypothyroid females and female control showed t-value -0.78 and p-value 0.21. Correlation coefficient was calculated between TSH and vitamin D levels in hypothyroid patients, a negative correlation was obtained, R= -0.28, p=0.04. This means as the TSH value increases vitamin D levels increase. The same correlation coefficient was statistically insignificant between TSH and vitamin D levels in normal control R= 0.120, p= 0.4.
Figure 1: Showing age distribution among test and control Figure 2: Showing sex distribution among test and control
Figure 3: Showing number of people with Vitamin D deficiency Figure 4: Showing vitamin D deficiency among males and females in test and control group
Table 1: Showing number of people with hypothyroid and vitamin D levels in individual groups
DISCUSSION Total 50 patients and 50 controls were studied. Maximum number of cases belonged to age 40-60 years both test and control. 32% were in age group 50-59 years. 68% were females in test group and 78% were females in control group. Our results were similar to another study done in Cochin by Usha menon V et al where it was found that in women, the prevalence was higher (11.4%), when compared with men (6.2%). The prevalence of subclinical hypothyroidism increased with age5. Study done by Unnikrishnan AG et al showed that prevalence of hypothyroidism was higher in female when compared to males and older age group compared to younger6. In hypothyroid group 60% patients had vitamin D deficiency, 16% had vitamin D insufficiency. In control group 44% had vitamin D deficiency, 26% had vitamin D insufficiency. Study done by Sudha K et al showed that 75% of patients with subclinical hypothyroidism had suboptimal vitamin D levels7. A study conducted in Saudi Arabia by Dr. Amal Mohammed Husein Mackawy et al showed that, Vitamin D was significantly lower in hypothyroid patients than in controls (t=-11.128, P =0.000)8. Another study by S Kivity on Vitamin D status in hypothyroidism in people with autoimmune thyroid disorder showed that 72%, particularly in patients with Hashimoto’s it was 79%[9]. Similarly study done on vitamin D levels in Hashimoto’s disease by Tamer G et al had shown that prevalence of vitamin D deficiency was 92% amongst Hashimoto’s patient group10. Among the hypothyroid patients 40% patients were having normal TSH levels, 8% had TSH less than 0.34 uiu/ml, 52% had TSH >5.6 uiu/ml. Another significant observation was made where 73% of the hypothyroid patients with TSH > 5.6 uiu/ml had vitamin D deficiency, 15% had Vitamin D insufficiency. Amongst the hypothyroid patients with normal TSH levels, 45% patients had vitamin D deficiency, 20% had vitamin D insufficiency, this result was comparable with the normal controls were 44% had vitamin D deficiency, 26% had vitamin D insufficiency. T test was applied between vitamin D levels in people with uncontrolled hypothyroidism and control P value was 0.0023. T test was applied between vitamin D levels in hypothyroid with normal TSH and control P value was 0.28, T test between vitamin D levels and TSH in normal control showed p= 0.37. Uncontrolled hypothyroid patients have a higher prevalence of vitamin D deficiency when compared to those with controlled hypothyroidism. But vitamin D deficiency can still, be seen in hypothyroid patients with normal TSH, but their prevalence becomes equal to normal controls. In adults, Harinarayan et al studied vitamin D levels in women of reproductive age and postmenopausal women from South India. 76% of reproductive age women and 70% of post-menopausal women were reported to be vitamin D deficient [11]. Studies from Lucknow (Central India) by Sachan A etal have also shown that 84.3% urban women and 83.6% rural women suffered from vitamin D deficiency12. In another study from Kashmir (North India) by Daga RA et al, 58.5% of adults were vitamin D deficient13. In our study 75% of the males with hypothyroidism had vitamin D deficiency, where as in females with hypothyroidism it was 52.9%, in controls too, 54% of males had vitamin D deficiency, where as in females it was 41%. T test was applied to vitamin D levels between males and females in hypothyroidism p-value was 0.087. T test was applied between vitamin D levels of males and females in control t-value p-value 0.256, vitamin d levels compared between males with hypothyroidism and controls p-value was 0.07 and T test between hypothyroid females and control showed p-value 0.21. This suggests that though according to percentage males showed higher prevalence of vitamin D deficiency, this difference was statistically not significant. In the study by Sudha K et al vitamin D deficiency in subclinical hypothyroidism showed that, there was no significant difference in vitamin D deficiency prevalence among sexes7. Wacker M et al in their study -Sunlight and Vitamin D: A global perspective for health, shown that solar UVB radiation (280-320 nm) is an initiator of Vitamin D3 production in the human skin14. Balasaraswathy P et al in their study- UVA and UVB in sunlight, Optimal Utilization of UV rays in Sunlight for phototherapy have shown that UVB radiation was maximum between 12 pm-1am and ideal time for UVB phototherapy was 11 am to 2pm15. Because of the changing life style and working hours, most people are inside buildings during the maximum UVB irradiance; this may explain the increased prevalence of vitamin D deficiency in males in our subpopulation. There was negative correlation between vitamin D levels and TSH in hypothyroid patients suggesting the more the TSH value that is the uncontrolled hypothyroidism is the lower would be the vitamin D levels. Similar correlation was not seen among normal controls.
CONCLUSION Vitamin D levels must be checked in all hypothyroid patients, specifically in people with age 50-59 years, uncontrolled hypothyroidism as both uncontrolled hypothyroidism and vitamin D deficiency may present with similar nonspecific complaints.
RECOMMENDATIONS
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||
 Home
Home