|
Table of Content - Volume 4 Issue 2- November 2016
Carotid intimo-medial thickness in type 2 diabetes and its correlation to coronary risk factors
Sanjay T Thorat1, Mayur Kondewar2, Omkar R Patil3*
1Associate Professor, 2,3Jr. Resident, Department of Medicine, Krishna Institute of Medical Science, Karad, Maharashtra, INDIA. Email: mayurkon@gmail.com
Abstract Background: Diabetes mellitus also accelerates atherosclerosis. An increased carotid intimo-medial thickness (CIMT) was observed in type 2 diabetic patients. Furthermore, asymptomatic hyperglycemic subject were shown to have significant IMT in comparison with healthy control Material and Method: 102 Patients reporting in Medicine ward were studied. The study was undertaken with following objectives. Patients of more than 35 years of age with type II diabetes mellitus according to the criteria of World Health Organization (WHO) are included and critically ill patients and type I diabetes mellitus patients are excluded. The study was designed to identify Carotid intimomedial thickness in Type 2 with coronary risk factors. Results: In type-2 DM patients with CHD, the mean R-CIMT was 1.06 ±0.20, mean L-CIMT was 1.09 ± 0.18 and mean of M-CIMT was 1.08 ±0.18.In type-2 DM patients without CHD, the mean R-CIMT was 0.77 ±0.13, mean L-CIMT was 0.82 ± 0.18 and mean of M-CIMT was 0.80 ±0.15.The age was significantly higher in patients with CHD group as compared to patients without CHD (p=0.001). The weight and BMI were also significantly higher in patients with CHD group as compared to patients without CHD (p=0.001). Height and WHR were comparable in both the groups (p>0.05).Similarly, duration of diabetes was significantly higher in patients with CHD group as compared to patients without CHD (p=0.01).R-CIMT, L-CIMT and MCIMT were significantly higher in patients with CHD group as compared to patients without CHD (‘p’=0.001). Conclusion: There is a correlation of carotid intimomedial thickness with coronary risk factors particularly triglyceride and micro-albuminuria. Patients having known hypertensive, high triglycerides and high microalbuminuria are shown to have high carotid intimomedial thickness.IMT of the common carotid artery is an excellent non-invasive measure of generalized atherosclerosis and is also a surrogate marker of coronary artery disease and is a strong independent predictor for new cardiovascular events. Key Words: Carotid Doppler, carotid intimo-medial thickening, coronary artery disease, diabetes mellitus type2.
INTRODUCTION Various studies showed that the patients with diabetes are two to four times more likely to develop cardiovascular disease than those in the general population and have a two to five time's greater risk of dying from these diseases.8,9 In the worldwide INTERHEART study of patients from 52 countries, diabetes accounted for 10% of the population attributable risk of first MI.I-10. Diabetes mellitus also accelerates atherosclerosis. An increased carotid intimo-medial thickness (CIMT) was observed in type 2 diabetic patientsI-11,I-12. Furthermore, asymptomatic hyperglycemic subject were shown to have significant IMT in comparison with healthy control subjectsI-13. It was suggested by the International Atherosclerosis Project that the atherosclerotic process occurs at the same time in the carotid, the cerebral and the coronary arteries. The CIMT, an established indicator of atherosclerosis and an important functional predictor of cardiovascular system can effectively be used to measure progress of atherosclerosis and also to assess the success of interventions. Measurement of CIMT by non-invasive B-mode ultrasonography can detect atherosclerosis at the earliest preclinical stage and help in the prediction and diagnosis of asymptomatic vascular disease. The assessment of carotid atherosclerosis by ultrasonographic measurement of CIMT took over as being the marker of atherosclerosis. A highly accurate, reproducible, reliable and valid estimate of the arterial wall thickness and a useful tool for detecting and monitoring changes in intima media thickness and assessing sub clinical atherosclerosis4-6 was now available. Today the progression of CIMT is an independent predictor of atherosclerotic events and a useful surrogate marker for coronary and other atherosclerotic events, and numerous studies have shown that CIMT is higher in type 2 diabetes mellitus patients than in non diabetic patients. Measurement of the intimal-medial thickness (IMT) of the carotid artery by B-mode ultrasound was found to be a suitable noninvasive method to visualize the arterial walls and to monitor the early stages of the atherosclerotic process. The thickness of the Carotid artery was demonstrated to be related to cardiovascular risk factors and to the occurrence of CHD. The development of sonography technology has allowed the noninvasive evaluation of atherosclerosis in the carotid arteries. The initial manifestation of carotid atherosclerosis is characterized by a subtle increase in vascular IMT, the progression of which leads to plaque formation and vascular narrowing. Reflecting systemic atherosclerosis, increased CIMT is associated with a higher risk for stroke.I-14 In a case-control study,I-15 increased IMT was associated with an increased risk of stroke. In another study, an association between increased IMT and the risk of incident stroke was observed; the relative risk increased in a linear fashion with increasing IMT and was of the same magnitude as the relative risk for myocardial infarction. Several studies have demonstrated the potential value of CIMT and plaque score for assessing the risk of atherothrombotic infarction and lacunar infarction but not for other stroke subtypes, such as cardioembolic infarction, cerebral hemorrhage, and other or unclassified stroke. They demonstrated that atherosclerosis does not play an important role in cardioembolic infarction, cerebral hemorrhage, and other or unclassified stroke. A study by Agarwal et alI-16 examined the CIMT in Indian diabetic patients. The study found a higher CIMT in diabetics who had coronary artery disease (CAD), even when the CAD was not clinically overt. This led the authors to conclude that the CIMT is a reliable surrogate marker for subclinical CAD in diabetic patients. The cardiovascular health study collaborative research group has recently observed that the relative risk for myocardial infarction (MI) or stroke for the quantile with the highest IMT as compared with the lowest quantile was 3.87. IMT is a strong independent predictor for new cardiovascular events, even after statistical adjustment for other traditional risk factors.I-17 Mohan et al18 in the Chennai Urban Population Study (CUPS) in 2000 studied IMT of the carotid artery in South Indian diabetic and non-diabetic subjects and observed that the mean IMT value of the diabetic subjects (0.95 ± 0.31 mm) was significantly higher than those of the non-diabetic subjects (0.74 ± 0.14mm) (p<0.001). Both in the normal and diabetic subjects, these values increased with age. At any given age, the diabetic subjects had higher values than the non-diabetic subjects but the difference reached statistical significance after the age of 50 years (p<0.05). IMT showed a correlation with age and duration of diabetes in the diabetic subjects. Multivariate regression analysis showed that age and diabetes were the major risk factors for IMT. Keeping the implications of the above in mind, the present study was undertaken to know the relationship of CIMT with risk factors for atherosclerosis in type 2 diabetes mellitus patients. This is the first ever cross sectional analysis carried out in type II diabetic patients in the XX and surrounding region.
MATERIAL AND METHODS This was a Cross sectional study. The study was carried out at Krishna Hospital, Karad. 102 Patients reporting in Medicine ward were studied. The study was undertaken with following objectives. Patients of more than 35 years of age with type II diabetes mellitus according to the criteria of World Health Organization (WHO) are included and critically ill patients and type I diabetes mellitus patients are excluded. Study Procedures: The study was conducted on 102 patients with type II diabetes mellitus reported in Krishna hospital. The study was designed to identify Carotid intimomedial thickness in Type 2 with coronary risk factors. All patients with type II diabetes mellitus attending the Medicine ward were invited to participate in the study and written informed consent was taken. All patients underwent a standard clinical and laboratory evaluation. Demographic information such as age, sex, weight and height were requested. Information on duration of diabetes was taken. Following this, BMI, waist-hip ratio and other parameters such as arterial blood pressure was measured. Following inclusion criteria were considered: patient with type II diabetes mellitus as per the WHO criteria (age ≥35 years and absence of insulin requirement in the first 5 years after diagnosis).All patients further underwent through following procedure to confirm the diagnosis of coronary heart disease.
Those patients who were positive in either TMT or 2D-ECHO were labelled as patients with Coronary Heart disease and patients with negative findings in TMT and 2D-ECHO were considered as normal patients. Carotid Doppler were performed in all patients to measure the Carotid intimo-medial thickness using Ultrasonographic scanning of the Ccarotid arteries on the pulse Doppler, with an machine equipped with colour flow imaging and electrical linear transducer. The scanning session will be for an average of 30 minutes. The IMT, as defined by Pignoli et al,6 will be measured as the distance from the leading edge of the first echogenic line to the leading edge of the second echogenic line. The first line represents the lumen intimal interface and the second line is produced by the collagen containing upper layer of the tunica adventitia. The image will be focussed on the posterior far wall and four images of the left and right common carotid arteries each will be recorded at least 15 mm proximal to the bifurcation. The CIMT will be calculated as the mean of eight measurements. IMT values below 0.8 mm are considered as normal. The presence of plaques and degree of stenosis will be noted and analysed. Plaque is defined as a localized lesion of thickness > 1.0 mm; stenosis defined as > 50% occlusion with systolic frequency peak > 4.0 KHz and spectral broadening. Carotid intimo-medial thickness of both right and left carotid arteries were measured; and mean carotid intimo-medial thickness was calculated. All the data were captured in the pre-printed pro-forma.
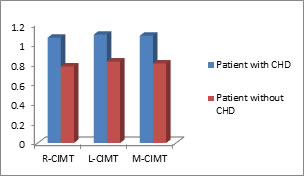
OBSERVATIONS AND RESULTS Table 1: Carotid intimo-medial thickness in type-2 DM patients with CHD
In type-2 DM patients with CHD, the mean R-CIMT was 1.06 ±0.20, mean L-CIMT was 1.09 ± 0.18 and mean of M-CIMT was 1.08 ±0.18.
Table 2: Carotid intimo-medial thickness in type-2 DM patientswithout CHD
In type-2 DM patients without CHD, the mean R-CIMT was 0.77 ±0.13, mean L-CIMT was 0.82 ± 0.18 and mean of M-CIMT was 0.80 ±0.15.
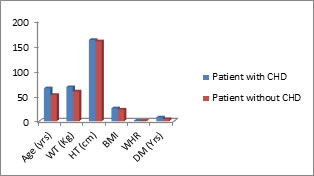
Table 3: Comparison of demographic characteristics of type-2 DM patients with and without CHD
“t test” is applied. P value is significant if < 0.05.
Legend Figure 1: Comparison of demographic characteristics of type-2 DMpatients with and without CHD Figure 2: Comparison of carotid intimo-medial thickness of type-2DM patients with and without CHD The age was significantly higher in patients with CHD group as compared to patients without CHD (p=0.001). The weight and BMI were also significantly higher in patients with CHD group as compared to patients without CHD (p=0.001). Height and WHR were comparable in both the groups (p>0.05). Similarly, duration of diabetes was significantly higher in patients with CHD group as compared to patients without CHD (p=0.01).
Table 4: Comparison of carotid intimo-medial thickness of type-2DM patients with and without CHD
“t test” is applied. ‘p’ value is significant as (‘p’< 0.05) R-CIMT, L-CIMT and MCIMT were significantly higher in patients with CHD group as compared to patients without CHD (‘p’=0.001).
DISCUSSION Patients with diabetes mellitus suffer unduly from premature and severe atherosclerosis. The Framingham study pointed out that diabetic individuals have higher serum concentrations of lipids and more hypertension, obesity, and thus are more prone to advanced atherosclerosis and it’s sequelae, namely coronary artery disease (CAD), cerebrovascular disease, aortic atherosclerosis, and peripheral vascular disease. Ultrasonographic assessment of easily accessible arteries has been advocated as a surrogate marker for less accessible vessels, such as coronary and cerebral arterial systems. Ultrasound imaging, which can provide information on intimal-medial thickness (IMT), plaque presence and type, calcification, and wall diameter, offers the ability to examine pre-symptomatic lesions, assess atherosclerotic burden and hence the risk of cardiovascular events. Intimal-medial thickness of the common carotid artery is considered to be an excellent non-invasive measure of generalizedatherosclerosisD-1,D-5 and also a surrogate marker of coronary arterydisease.D-6,D-7 It is also extensively used to examine the stage of atherosclerosis and to evaluate the regression of atherosclerotic lesions. following intervention therapies.[D-8,D-10] The international atherosclerosis project has suggested that the carotid and cerebral arteries and the aorta undergo the atherosclerotic process approximately at the same age as the coronary arteries.[D-11] Moreover, there is good agreement between histological examination and the ultrasonographic evaluation of the carotid arteries.D-12 The current study was undertaken primarily to determine the carotid intimomedial thickness in Type II Diabetes Mellitus patients with coronary heart disease (CHD) as compared to Type II Diabetes Mellitus patients without coronary heart disease (CHD). The correlation of carotid intimomedial thickness with coronary risk factors in patients with Type II Diabetes Mellitus was the secondary objective. The mean CIMT in our study group of a total of 102 cases with type 2 diabetes was 0.98 ± 0.21 mm. The value was higher than the non-diabetic patients. The age, weight, BMI were significantly higher in patients with CHD group as compared to patients without CHD (p=0.001). Height and WHR were comparable in both the groups (p>0.05). Similarly, duration of diabetes was significantly higher in patients with CHD group as compared to patients without CHD (p=0.01). The finding was in the line with the published literature. Mohan et alD-13 in the Chennai Urban Population Study (CUPS) in 2000 studied IMT of the carotid artery in South Indian diabetic and non-diabetic subjects and observed that the mean IMT value of the diabetic subjects (0.95 ± 0.31 mm) was significantly higher than those of the non-diabetic subjects (0.74 ± 0.14 mm) (p<0.001). Both in the normal and diabetic subjects, these values increased with age. At any given age, the diabetic subjects had higher values than the non-diabetic subjects but the difference reached statistical significance after the age of 50 years (p<0.05). IMT showed a correlation with age and duration of diabetes in the diabetic subjects. In a study by Aggarwal et al, the mean CIMT in study group of a total of 111 cases with type 2 diabetes was 0.840 ± 0.18 mm. This was lower than the value reported by Mohan et al in the CUPS study (0.95 ± 0.31 mm), yet higher than normal. Multivariate regression analysis showed that age and diabetes were the major risk factors for IMT. Kawamori et alD-3 (1992) in their study on the prevalence of carotid atherosclerosis in diabetic subjects concluded that IMT is linearly related with age in diabetic subjects (IMT = [0.0155 x age] + 0.32450). Multivariate regression analysis of 275 type 2 diabetic cases indicated that smoking, hyperlipidaemia, duration of diabetes, hypertension and age were factors determining thickness of the carotid arterial wall. In our study, in type-2 DM patients with CHD, the mean R-CIMT was 1.06 ± 0.20, mean L-CIMT was 1.09 ± 0.18 and mean of M-CIMT was 1.08 ± 0.18. In type-2 DM patients without CHD, the mean R-CIMT was 0.77 ± 0.13, mean L-CIMT was 0.82 ± 0.18 and mean of M-CIMT was 0.80 ± 0.15. We found significantly higher R-CIMT, L-CIMT as well as Mean CIMT in patients with CHD group as compared to patients without CHD (p=0.001). In a study in 2001 by Jadhav et al,[D-14] an IMT greater than 0.8 mm was observed in CAD patients (whether diabetic only, hepertensive only, or both), as against those without CAD; this difference was most marked in the hypertensive group (22.2% vs. 3.6%) and contributed to the increased arterial thickness in diabetics with concomitant hypertension. Multivariate regression analysis revealed CIMT to be associated with CAD with an odds ratio of 2.40. In a study by Aggarwal, CIMT was found to be very strongly and significantly correlated with the prevalence of CAD (p<0.0001). Among the CAD patients, hypertriglyceridaemia (HTG) was significantly correlated to mean CIMT (p<0.001). Temelkova-Kurktschieu et alD-15 observed that postprandial HTG correlates with increased IMT in type 2 diabetics. In our study, the SBP and DBP were significantly higher in patients with CHD group as compared to patients without CHD (p=0.001). Further, though, the parameters like BSLF, BSLPP, HbA1c, BUL, creatinine, total cholesterol, LDL, VLDL and HDL were comparable in both the groups (p>0.05); TRG and M-ALB were significantly higher in patients with CHD group as compared to patients without CHD (p=0.001). In type-2 DM patients with CHD, mean of total cholesterol was 171.55 ± 43.54, and the mean M-ALB was 158.42 ± 182.22. In type-2 DM without CHD, the mean of total cholesterol was162.63 ± 30.57, and the mean value of M-ALB was 26.95 ± 25.77. The findings are in the line with published literature. Chen et alD-16 investigated the association of fasting and postprandial triglyceride levels with CIMT among type 2 diabetic patients in Southeast China. The CIMT in patients with postprandial HTG was significantly greater than that in patients with postprandial normo-triglyceridaemia (p<0.05). The cardiovascular health study collaborative research group has recently observed, in 4476 subjects without clinical cardiovascular disease followed over 6 years, that the relative risk for myocardial infarction (MI) or stroke for the quantile with the highest IMT as compared with the lowest quantile was 3.87. IMT is a strong independent predictor for new cardiovascular events, even after statistical adjustment for other traditional risk factors. In a case control study of 772 persons selected from the ARIC population to evaluate adults free of clinical cardiovascular disease, case subjects, identified on the basis of carotid arterial wall thickness, had consistently higher values for atherogenic risk factors (age, body mass index, systolic and diastolic blood pressure, pack years of smoking, total triglycerides, low-density lipoprotein (LDL cholesterol), and low high density lipoprotein (HDL cholesterol) than control subjects. Carotid IMT (CIMT) has been shown to be independently associated with CAD in Indian subjects. This fact was reinforced by our study wherein CIMT was found to be very strongly and significantly correlated with the prevalence of CAD (p<0.0001). In our study, among the CAD patients, triglyceride and micro-albuminuria was significantly correlated to mean CIMT (p<0.001). Nagai et al,D-17 in 1998, compared CIMT in asymptomatic older subjects with exercise - induced myocardial ischaemia. They observed that exercise induced ST-segment depression was associated with increased IMT (p<0.0001) independent of age and manifest CAD. After adjustment for age, IMT values progressively increased from healthy subjects to asymptomatic subjects with positive exercise ECG alone to those with concordant positive ECG and thallium scintigraphic findings who had virtually identical IMT to subjects with manifest CAD. Each 0.1 mm increase in IMT was associated with a 1.91 fold increased risk for concordant positive exercise tests or manifest CAD, independent of other significant predictors of CAD. Aggarwal et al., also found a strong and significant correlation between mean CIMT and prevalence of silent ischaemia, (p<0.001). On multivariate regression analysis, keeping mean CIMT as the dependent variable, the predictors that were seen to affect IMT included serum creatinine, total cholesterol levels, serum triglyceride levels and microalbuminuria. Jadhav et alD-18 in their study on association of microalbuminuria with IMT and CAD observed that microalbuminuria had a strong association with high IMT in diabetic subjects. Aggarwal et al., also found in diabetics with silent ischemia are similar to their observations, as microalbuminuria had a significant correlation (p<0.05) with IMT in this subgroup.
CONCLUSION The present study comprised of 102 patients with type-2 diabetes. A high mean CIMT (>0.9 mm) was seen in the study. Comparison of type 2 diabetic patients with and without CAD revealed that the presence of CAD was significantly associated with age (p<0.001), weight (p<0.001), BMI (p<0.001), duration of DM (p<0.001), triglycerides (p<0.001), microalbuminuria (p<0.001), and mean CIMT (p<0.0001). There is a correlation of carotid intimomedial thickness with coronary risk factors particularly triglyceride and micro-albuminuria. As we can seen here, the patients having known hypertensive, high triglycerides and high microalbuminuria are shown to have high carotid intimomedial thickness. IMT of the common carotid artery is an excellent non-invasive measure of generalized atherosclerosis and is also a surrogate marker of coronary artery disease and is a strong independent predictor for new cardiovascular events.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home