|
Table of Content - Volume 4 Issue 3- December 2016
Clinico - mycological study of dermatophytosis in a tertiary care hospital in central India
Shaikh Waseemuddin Nayeemuddin1*, Jayesh Ishwardas Mukhi2, Kinjal Deepak Rambhia3, Rajesh Pratap Singh4
1Resident Doctor, 2Associate Professor, 3Assistant Professor, 4Professor and HOD, Department of Dermatology-Venereology-Leprosy, Government Medical College and Hospital, Nagpur, Maharashtra-440003., INDIA. Email: waseemgmc8854@gmail.com, jayesh.mukhi@gmail.com, kinjal_rambhia@hotmail.com, rpsingh13m@gmail.com
Abstract Background: Dermatophytoses are superficial fungal infection of skin, hairs and nails. It constitutes one of the major burden of dermatology clinic. Nowadays there is an upsurge in the incidence and treatment resistance has been increasing. Aim: To study the clinicoetiological profile of dermatophytic infections. Setting: Hospital based observational study Material and Methods: One hundred and ten clinically diagnosed cases of dermatophytoses were included. After taking detailed history and complete cutaneous examinations, 10 % KOH for skin and hairs, while 40% KOH for nail samples was done along with culture on Sabourads dextrose agar slant, containing 0.05% chloramphenicol and 0.5% cycloheximide. Results: Males are more affected than females with male : female ratio of 1.34. Most common age group affected in 20-40 yrs (47.27%). Out of 110 samples, 62 (56.36%) were KOH positive, while 48 (43.63%) were culture positive. Trichophyton mentagrophytes was the predominant species isolated, followed by Trichophyton rubrum. Also Trichophyton terrestre was isolated in 2 samples. Conclusions: There is changing etiological spectrum of dermatophytosis in central india. Key Words: Central India, Dermatophytosis, Trichophyton mentagrophytes, Trichophyton rubrum, Trichophyton terrestre
INTRODUCTION Dermatophytes (literal meaning skin plant) are causative agents of superficial fungal infections of the keratinized tissues namely skin, hair, and nails. Dermatophytes represent more than 40 closely related species of three genera Trichophyton, Epidermophyton and Microsporum, classified by habitat and host preferences into three classes - anthropophilic, geophilic and zoophillic. Dermatophytoses are one of the most common dermatological problems especially in developing countries like India. The etiological spectrum varies according to time and place, which may be attributed to changes in climatic and socioeconomic conditions. Recently there has been a surge in the incidence in the dermatophytosis. The reasons which could contribute to this increase might be the change in the etiological agent, with antifungal resistance also as a major factor. Surveillance is crucial for defining the burden of infection and changing trend; for evaluating the proper intervention. There are few studies in central India on dermatophytoses. Hence the present study was undertaken to study the clinicoepidemiological profile and etiological spectrum of dermatophytoses in a tertiary care centre; and to correlate the clinical diagnosis with potassium hydroxide smear and culture positivity.
MATERIALS AND METHODS 110 clinically diagnosed patients of dermatophytosis attending our outpatient department were included in this study after obtaining written informed consent. The patients were randomly selected for the study. Ethical clearance was obtained before the start of study from the institutional ethical committee. Patients of all age group above one year were included in the study. Patients who were not willing for consent, pregnant females, patient on systemic antifungal treatment within last 1 month, applying steroids and indigenous topical preparations were excluded from the study. Detailed history and clinical examination were performed in each case. Routine investigations were done in all cases. Based on the site of infection scales, nail scrapping or hair were collected by the standard set of procedures. Specimens were subjected to potassium hydroxide – 10% for skin and hair samples; while 40% for nail sample, for a demonstration of fungal elements. Irrespective of KOH findings, all specimens were subjected to culture on Sabourads dextrose agar slant, containing 0.05% chloramphenicol and 0.5% cycloheximide to eliminate bacterial and nondermotophtyic molds contamination. Culture tubes were incubated at 28°c for up to four weeks to label it as negative. Individual fungal isolates were identified based on macroscopic examination of the colony - morphology, pigmentation, growth rate, slide culture and lactophenol cotton blue mount. Special tests like hair perforation and urease test were done wherever required. Non dermatophytic moulds on culture were excluded and considered negative.
RESULTS Out of 110 patients, 63 (57.27%) were males; while 47 (42.72%) were females with male female ratio of 1.34. Among various clinical presentations of dermatophytes, tinea corporis was most common in 31 (28.18%), followed by mixed pattern in 23 (20.90%) of patients. Most common age group affected was 20-40 yrs with 52 (47.27%) cases. Students were most common group affected, i.e 31 (28.18%). Family history / Contact history was given by 32 (29.09%) of cases. Among 110 samples given for KOH and culture, 62 (56.36%) were KOH positive, while 48 (43.63%) were positive on culture considering only dermatophytes. 8 samples were positive on culture but negative on KOH mount. Trichophyton mentagrophytes was most common isolate in 19 (40.42%) out of 48 culture positive samples, followed by Trichophyton rubrum in 11 (26.19%). Other dermatophytes grown on culture were T.Verrucosum, T.Tonsurans, T.Violaceum, E.Floccusum, Trichophyton terrestre, Microsporum ferrugineum, Trichophyton sondanse, Trichophyton Schoenleinii. Table 1
Table 2
Table 3
Table 4
Table 5
Table 6
Table 7
Others: Trichophyton terrestre, Microsporum ferrugineum, Trichophyton sondanse, Trichophyton Schoenleinii
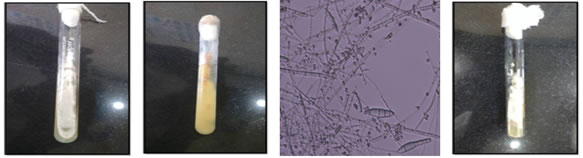
Figure 1: Figure 2: Figure 3: Figure 4: Figure 5: Figure 6: Figure 7: Figure 8:
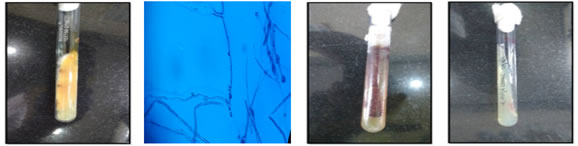
Figure 9: Figure 10: Figure 11: Figure 12:
Figure 13: Figure 1: T.mentagrophytes ; Thallus color: white to sandy to butter yellow; Figure 2: T.mentagrophytes; Reverse: white to tan, rarely reddish brown; Figure 3: T.mentagrophytes; Round microconidia in grape-like clusters, spiral hyphae, +/- cigar shaped, thin walled macroconidia, narrowly attached to hyphae; Figure 4: T.rubrum; Thallus color: white to pale pink; Figure 5: T.rubrum; Reverse: blood red to reddish brown; Figure 6: T.rubrum; Few pyriform, lateral microconidia pencil shaped , macroconidia uncommon,‘birds on wire’ appearance; Figure 7: T.Violaceum; Thallus color: purplish red with white sectors; Figure 8: T.Violaceum; Reverse: lavender to purple; Figure 9: T.Verrucosum; Thallus color: white, grey or yellow; Figure 10: T.Verrucosum; Reverse: colorless; Figure 11: T.terrestre; Thallus color: white to yellow; Figure 12: T.terrestre; Reverse: yellow, occasionally red; Figure 13: T.terrestre; Microconidia pyriform to elongate, often on pedicels
DISCUSSION Present study is carried in central India, where climate is hot and humid, thereby facilitating growth of fungus. Males are more affected than females with male female ratio of 1.34, a finding that is well correlated with previous studies done by Noronha et al.1, Amin et al.2 and Singh et al.3 The reason for less incidence in females might be due to social restrictions, personal inhibitions preventing them for reporting. The most common age group is 20-40 yrs of age. This finding is in collaboration with studies by Chaudhary et al.4, Aggrawal et al.5 and Grover et al 6. Both of these facts can be explained by outdoor physical activity increasing the exposure. The most common clinical presentation is Tinea corporis followed by mixed pattern. This can be partly attributed by fact that people are not reporting early so many present mixed pattern at presentation. This is in accordance with the studies done by Surekha et al7., Nagabhusanam et al.8 and Patwardhan et al.9 and few other studies.10-13 We got 20.3% of mixed infection, a finding correlated with Siddappa et al.(23%)14, which can be explained by delay in reporting. Also we found that Tinea capitis affected only children less than 10 yrs of age, a similar finding reported by Grover et al. 14, more common in males than female. This can be explained by increased fungistatic triglyceride content of sebum in adults.15 Short hairs in male facilitates the growth of fungus, while regular use of vegetable oil is associated with low incidence of Tinea capitis in females.16 Most common group affected were students. Unskilled workers were more affected than skilled workers. Both the facts can be attributed by fact that they are more exposed to outdoor environment. Family history was given by 32 (28.18 %). Bindu et al17 reported family history in 30 cases - 20%. In our study KOH positivity was seen in 62 (56.63%), while culture positivity 48 (43.63%). 22 (20%) samples were KOH positive, culture negative. 8 samples were KOH negative, culture positive which can be due to error in reporting the KOH mount or insufficient sample. 40 samples (36.36%) were both KOH and culture negative. Comparable findings were reported by Noronha et al.1, Chaudhary et al.4, Bindu et al.17, Kumaran et al.18 hence we can assume that both KOH mount and culture should be done to prevent false negative reporting. Trichophyton mentagrophytes was the most common species isolated on culture (40.42%), followed by T.rubrum. Similar findings have been reported by Noronha et al1, Kumaran et al.18 Agrawal et al.19 kumaran et al.18 It was undoutedtly proven that T.rubrum was most common causative organism for dermatophytosis.3,4,7-9,11,12,20,21 But recently there has been change in etiological spectrum with most common cause T.mentagrophytes, a zoophillic from an anthropophillic species, T.rubrum. However Grover et al.6 had reported T. tonsurans (20.5%) as the commonest isolate. It could be explained on the basis of different climatic conditions and geographic distribution. In our study, geophillic species, T.terrestre was isolated in 2 cases. After reviewing the literatrure, we found that there has been only one case report of T.terrestre in india.22 It has been stated that lesions of zoophillic and geophillic species are more inflammatory than those of anthrophillic infection. We can assume that there has been change in morphology of dermatophytes to more inflammatory type of lesions.23 Also there has been studies regarding antifungal succepptibility of both of these species, indicating lower efficacy of fluconazole, while higher with griseofulvin and ketoconazole of T.mentagrophytes as compared to T.rubrum.24,25,26
CONCLUSION There is changing pattern of etiological spectrum of dermatophytosis. There might be change in the clinical presentation. Also there might be change in antuifungal sensitivity. Both of these facts are to further justified by more large scale studies.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home