|
Table of Content Volume 12 Issue 2 - November 2019
Study of sacral hiatus and its anatomical variation
Jyoti C Nayak1*, R V Dave2
1,2Assistant Professor, Department of Anatomy, B.J. Medical College Ahmedabad, Gujarat, INDIA. Email: drjyoti.c.nayak@gmail.com
Abstract Back ground: sacrum is the large wedge shape bone which support the vertebral column form by fusion of five sacral vertebra. Sacral canal is form by superimposed vertebral foramina of the sacral vertebra and its lower end open at sacral hiatus. It is usually located inferior to the 4th or 3rd fused sacral spines or lower end of median sacral crest. Anatomical determination of the sacral hiatus is very important for performing successful caudal block. Aim: Morphology and Morphometry of Sacral hiatus are important clinically as well as surgically. Material and Methods: in this study 100 dry human sacra were used from Gujarat region, to know the anatomical variations of sacral hiatus. Anatomical measurements were performed on these specimens by using Vernier Calliper with accuracy of 0.1 mm. To interpret the data was analyzed statistically Result: Various shapes of sacral hiatus were observed which included inverted- U 45(45%), inverted- V 40 (40%), irregular 10 (10 %), dumbbell5 ( 5%) and bifid 0 (0%).The apex of sacral hiatus was commonly found at the level of 4th sacral vertebra in 50 (50%)at S3 sacral vertebra in 40(40%) and S5 in 8(8%) and at S1 level in only two (2%) of the sacral vertebra studied. Base of the hiatus was commonly found at the level of S5 in 61(61%) at S4 in 32(32%), C1 level in 7(7%) and at C2 in none of sacral vertebra. Length of sacral hiatus ranged between 10.0 mm to 56 mm, breadth at base was 9 mm to 23mm and anteroposterior diameter at apex was 4 mm to 9 mm. Conclusion: There are many anatomical variations seen in the sacral hiatus and the knowledge of these variations can improve the success of caudal epidural Block Key Word: sacrum, Sacral hiatus, Apex, Pelvic sacral foramina, sacral canal.
INTRODUCTION Sacrum is a triangular bone forming the caudal end of the vertebral column, formed by fusion of five vertebrae. Sacrum is considered to be most variable portion of spine1 it articulates on either side with hip bone to form sacro iliac joint.2. The sacrum consists of trabecular bone enveloped by a shell of compact bone of varying thickness1 It presents concave anterior or pelvic surface and convex posterior surface. The broad base is directed above and the apex is at the lower end. The sacral canal is formed by sacral vertebral foramina, and is triangular in section. Its upper opening, seen on the basal surface, appears to be set obliquely. The inclination of the Sacrum means that it is directed cranially in the standing position. Each lateral wall presents four intervertebral foramina, through which the canal is continuous with pelvic and dorsal sacral foramina. Its caudal opening is the sacral hiatus. The canal contains the cauda equina and the filum terminale, and the spinal meninges. Opposite the middle of the Sacrum, the subarachnoid and subdural spaces close: the lower sacral spinal roots and filum terminale pierce the arachnoid and dura mater at that level. The filum terminale with its meningeal coverings emerges below the sacral hiatus and passes downwards across the dorsal surface of the fifth sacral vertebra and sacrococcygeal joint to reach the coccyx. The fifth sacral spinal nerves also emerge through the hiatus medial to the sacral cornua, and groove the lateral aspects of the fifth sacral vertebra.3 Sacral hiatus is identified by palpation of sacral cornua. Sacral cornua are felt at the upper end of natal cleft 5cm above the tip of coccyx. Structures emerge from sacral hiatus are the filum terminale, fifth sacral nerves and coccygeal nerves. The hiatus provides access to the extradural space in the sacral canal.4 The route of access to the caudal epidural space is via the sacral hiatus. The space is therefore entered below the level of termination of the dural sac, i.e. the subarachnoid space and its contained CSF, which usually extends to the level of the second sacral segment. Occasionally the dural sac ends as high as the fifth lumbar vertebra, and very rarely it may extend to the third part of the Sacrum, in which case it is occasionally possible to enter the subarachnoid space inadvertently during the course of a sacral nerve block.3
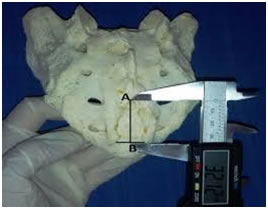
MATERIAL AND METHODS This study was performed in Department of Anatomy of B.J. medical college Ahmedabad Gujarat. This study consists of 100 dry, undamaged human sacrum of unknown sex was used. Anatomical measurements were performed on these specimens by using Vernier callipers with accuracy of 0.1 mm. To interpret the data was analyzed statistically. The different parameter of each sacrum was studied under the following headings:
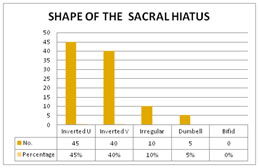
RESULTS AND OBSERVATION Table 1: Shape of sacral Hiatus
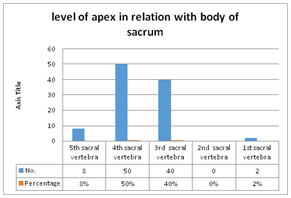
In table 1 the study show shape of the sacrum was Inverted U shape in maximum number and no bifid shape was found. Graph 1 Table 2: Apex Location ( level of Sacral vertebra)
Graph 2: Graph 2 shows level of apex in relation with body of sacrum found 4th sacral vertebra found maximum percentage in this study. Table 3
In table 3 shows level of base in relation with body of sacrum maximum at 5th sacral vertebra. Table 4: Morphometry of Sacral Hiatus
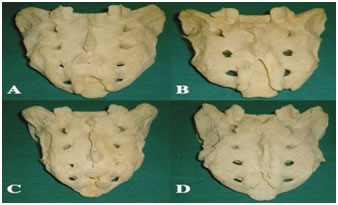
Figure 1 Figure 2 Figure 1: (A) Inverted U shaped. (B) Inverted V shaped (C) Dumbbell shaped, and (D) Irregular shaped; Figure 2: Measurement of length of sacral hiatus DISCUSSION Study on the variation in anatomical features of sacral hiatus and the dorsal wall of sacral canal is related with regards to its clinical application in caudal epidural anaesthesia. There were five shapes of Sacral Hiatus in our study: inverted U, inverted V, irregular, bifid and Dumbell. Nagar SK and Vandana et al also noted that most common Sacral hiatus being inverted U in 41.5 % and inverted V in 27% sacrum and 33% (Both U and V) respectively .Bifid hiatus was seen in 0% in present study which has not been reported in earlier studies. In the present study the most common shape of Sacral Hiatus was in inverted U and inverted V both are 45 % and 40% of sacrum respectively which was almost similar to Nagar S K5 and vandana et al6. Like Vinodkumar et al (1992)7 noted various shapes of sacral hiatus, most common being inverted V and inverted U in 76.23% sacra. Other Author has been mentioned various shapes of Sacral hiatus.8 In the present study the apex of sacral hiatus was seen most commonly (50%) at the level of 4th sacral vertebra. many studies have shown similar results like Vinod Kumar et al (1992)7 reported in his series that the apex of sacral hiatus was most commonly (76.23%) present against 4th sacral segment, Sekiguchi M et al (2004)9 noted the apex of sacral hiatus at S4 level in 64% cases. The base of sacral hiatus was seen at level of S5 vertebra in 61 % sacra, similar to Vinod kumar et al (1992, 83.17%)7. In our study the Length of sacral hiatus ranged between 10.0 mm to 56 mm, breadth at base was 9 mm to 23mm and AP diameter at apex was 4 mm to 9mm.which was nearly similar to Vandana et al6. Our study is similar to study by A. Agrawal et al10.
CONCLUSION Present study concludes in support of other studies regarding variability in the anatomical structure of sacral hiatus. Variations in the shape and level of the hiatus may lead to failure of Caudal Epidural Anaesthesia. The incidence of variations may be due to genetic and racial factors.
REFERENCES
|
|
 Home
Home