|
Table of Content - Volume 20 Issue 2 - November 2021
Association between birth weight and dysmorphic features among newborns
Sunil O1*, Trinesh Gowda M S2
1,2Department of Anatomy, Mandya Institute of Medical Sciences, Mandya, Karnataka, INDIA.
Abstract Background: Congenital anomalies are important cause of neonatal mortality and morbidity. The frequency of congenital anomalies worldwide is 3-5 %, although it varies from region to region and based on the socioeconomic and educational status of the nation. Congenital anomalies contribute to increased morbidity and mortality among Low Birth Weight (LBW) infants and are often associated with expensive medical and surgical care that compounds medical problems related to LBW. Aim And Objective: To identify and record the birth defects (external dysmorphism) among newborns delivered in district hospital attached to Mandya Institute of Medical Sciences, Mandya for a period of one year and study the association between birth weight and the dysmorphic features among newborn. Methodology: After obtaining written informed consent of the parent, newborn was examined for birth defects (visible external dysmorphic features) and the details was recorded in the self- designed proforma and findings/data was tabulated and analyzed using appropriate statistical methods to study the association between birth weight and the dysmorphic features among newborn. Results And Conclusion: The prevalence rate of congenital anomalies in the present study was 3.4 %. Newborns with birth weight less than 2.5 kg showed more percentage of congenital anomalies (70.6 %). This study will form a guideline to conduct appropriate newborn screening for birth defects and also give feedback to the clinicians (obstetricians) to perform relevant antenatal investigations to prevent and detect the birth defects. Keywords: Anomalies, Dysmorphism, Malformation, Morbidity, Mortality
INTRODUCTION Congenital anomalies can be defined as structural or functional anomalies that occur during intrauterine life and can be identified prenatally, at birth, or sometimes may only be detected later in infancy and childhood, such as hearing defects.1 Serious birth defects can be lethal. For those who survive, these disorders can cause lifelong mental, physical, auditory or visual disabilities. Birth defects are a global problem, but their impact is particularly severe in middle and low income countries, where more than 94 % of the births with serious birth defects and 95 % of the deaths of these children occur.2 It accounts for 8-15 % of perinatal deaths and 13-16 % of neonatal deaths in India.3,4 The exact prevalence of Congenital anomalies varies in different areas and among different populations. Long-term survival of children with congenital anomalies is significantly lower than that for normal children.5 Despite of the high frequency of congenital anomalies the underlying causes for most remain obscure in 50 % of the cases. In 2010 congenital anomalies were estimated to be fifth largest cause of neonatal death.6 Around 40-60% of congenital anomalies are of unknown etiology, many are multi-factorial. Known factors are genetic, maternal, nutritional, behavioural, infectious and environmental.7 Preventive public health measures work to decrease the frequency of certain congenital anomalies through the removal of risk factors or the reinforcement of protective factors. Ensuring adolescent girls and mothers have a healthy diet, adequate dietary intake of vitamins and minerals, and particularly folic acid in adolescent girls and mothers, ensuring mothers avoid harmful substances, particularly alcohol and tobacco, eliminating environmental exposure to hazardous and teratogenic substances (such as heavy metals or pesticides) during pregnancy, increasing and strengthening education of health staff and others involved in promoting prevention of congenital anomalies and screening for infections, especially rubella, varicella, and syphilis, and consideration of treatment. Establishment of national capacity for surveillance and monitoring of common birth defects to make uniform policies and to allow for more robust evaluation of national interventions, such as fortification of the food supply with folic acid, iodine, vitamin D, vitamin A etc.6,8 Birth defects contribute to increased morbidity and mortality among LBW infants and are often associated with costly medical and surgical care that compounds medical problems related to LBW. An increasing number of statewide programs are being conducted for planning birth defect surveillance activities. LBW infants are at high risk for birth defects, targeting medical records of LBW infants should improve the overall ascertainment of birth defects in the population. And because a substantial proportion of LBW infants have associated birth defects, public health prevention strategies targeted at LBW should consider the etiology and pathogenesis of LBW and attempt to better delineate and prevent risk factors that influence the occurrence of birth defects.9 Peri-conception medical services assist women and their partners to attain optimal physical and mental health and well-being at the beginning of pregnancy to facilitate a normal pregnancy and delivery of a healthy infant. These include screening for the risk of genetic and teratogenic birth defects.10 Physicians, nurses and allied health professionals should be trained for early recognition of birth defects and knowing when to refer a patient for specialized treatment. Multidisciplinary approach is required for newborns with low birth weight for early detection and management of congenital anomalies.
MATERIALS AND METHODS Newborns delivered in the district hospital, Mandya Institute of Medical Sciences, Mandya for a period of 1 year were examined after obtaining written informed consent from parents, the newborn were examined for visible external dysmorphic feature and the details was recorded in the pre-designed proforma and findings/data was tabulated and analysed using appropriate statistical methods to study the association between birth weight and the dysmorphic features among newborn. Descriptive statistics comprising proportion and percentage was used to describe the data with graphical representation (bar diagrams, pie charts, line graph etc.). Photographs of the newborns with external birth defects/dysmorphism were taken for keeping record of the defect. Prior institutional ethical clearance was obtained from the Institutional Ethics Committee (IEC), Mandya Institute of Medical Sciences, Mandya for conducting the study and examining the newborns.
RESULTS This hospital based cross-sectional study was done at Tertiary Care Centre of Mandya Institute of Medical Sciences, Mandya for a period of 1 year on live newborns. The population for study were selected by using simple random method keeping in view the operational feasibility, 502 live newborns were examined physically for external dysmorphic features.
Table 1: Total number of external dysmorphic features among newborn
During the study period, 502 live newborns were examined at the district hospital Mandya Institute of Medical Sciences, of which 17 of the cases presented with external dysmorphic feature. The prevalence of the external dimorphism in the present study is 3.4%.
Table 2: Association with Birth weight and congenital dysmorphism
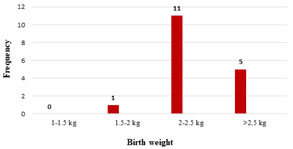
Figure 1: Association with Birth weight and congenital dysmorphism In the present study, the incidence of congenital malformations was significantly high among the Low Birth Weight babies in comparison to normal weight babies.
DISCUSSION During the study period, 502 live newborns were examined of which 17 (3.4%) of the cases presented with external dysmorphic features, which is a consistent with the proportion of cases observed by other investigators around the globe (3-6%). Worldwide prevalence is 3-5% but varies from country to country. In the present study prevalence rate is relatively low compared to 8% reported in Pakistan and in hospital neonatal unit based study of countries like Nigeria that has 3.7%, in Taiwan 4.3% and higher than European countries, Oman 2.46% and of Bahrain 2.7%.10 Various studies shows conflicting results in the developing countries like India, One such studies conducted by Sarkar et al.11 in Eastern India and Adnan et al.12 in Peshawar, Pakistan showed a prevalence rate of 2.22 % and 2.9 %. In the present study, the incidence of congenital malformations were significantly higher among the LBW babies in comparison to normal weight babies. This association of LBW and malformations has been well documented in other studies,13,14,15,16 which is consistent with the previous studies reported from Iran and Egypt. Devassy et al.17 and other studies also reported a greater incidence of congenital malformations among newborns with prematurity and LBW. The study conducted by Koumi et al.18 reported a high incidence of external dysmorphism in male neonates born with low birth weight and on the contrary Mekonen et al.19 in his study conducted in Ethiopia reported high incidence of congenital dysmorphism in female neonates born with very low birth weight.
CONCLUSION In the present study, out of the 502 newborn cases which were subjected for examination, 17 cases showed congenital external dysmorphism of various type. The prevalence rate in the present study was 3.4 %. Newborns with birth weight less than 2.5 kg showed more percentage of congenital anomalies (70.6 %). Birth defects contribute to increased morbidity and mortality among LBW infants and are often associated with costly medical and surgical care that compounds medical problems related to LBW. An increasing number of statewide programs are being conducted for planning birth defect surveillance activities. LBW infants are at high risk for birth defects, targeting medical records of LBW infants should improve the overall ascertainment of birth defects in the population. This study will form guideline to conduct appropriate new born screening for birth defects and also give feedback to the obstetricians to perform relevant antenatal investigations to prevent and detect the birth defects and take appropriate measures in the perinatal period/childhood period, to help the child to grow into productive and healthy individuals for the nation. CONTRIBUTIONS I, Dr.Sunil O have made contributions to acquisition of data, or analysis and interpretation of data; Dr. Trinesh Gowda have been involved in drafting the manuscript have given final approval of the version to be published. The source of funding is self.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home